1. Background
Postoperative sore throat (POST) syndrome is commonly observed after tracheal intubation, with an incidence rate of 14.5 - 50% (1-5). Its incidence after tracheal intubation varies from 6.6 to 90% (6). POST is the second most prevalent complaint following anesthesia, i.e., secondary to nausea/vomiting (4, 5).
Pharyngeal packs prevent swallowing blood and secretions that could induce Postoperative Nausea and Vomiting (PONV) among patients undergoing nasal surgery (5). However, in some studies, it has been mentioned that using pharyngeal packs may increase POST incidence due to local stimulation (7).
Various articles have reported several risk factors for POST, including female gender, smoking, difficulty intubation, using Succinylcholine, high intra-cuff pressure, airway suctioning, prolonged intubation, wearing laryngeal masks, damaged airway mucosa during laryngoscopy and using an oral airway and large endotracheal tubes (2, 3, 6-9).
Although the etiology of POST has not yet been fully understood, the inflammatory process appears to play an effective role (3). The tracheal mucus secretes inflammatory mediators due to cellular damage, which could affect the airway sensory nerves. The exact anatomical location of the sore throat has not yet been determined (1, 3). POST is a common complication that causes discomfort and dissatisfaction among patients and postoperative disorders following general anesthesia (3).
Various methods can be used to prevent POST, including applying lidocaine (over the tube cuff, intravenously, or as a gel on the exterior of the tube and as an aerosol spray) and steroids, the most common type of which is Dexamethasone (2, 3). Also, using Dexamethasone (IV) at a dose greater than 0.1 mg/kg is beneficial for reducing the severity of POST (3). Nonsteroidal anti-inflammatory drugs (NSAIDs) such as Benzydamine hydrochloride has antibacterial properties when used topically (2).
Several studies have examined the effect of Benzydamine in different ways: spraying at the endotracheal tube or inside the tube, gargling, and applying it to the oropharynx and tracheal cuff. The results showed a moderate reduction in the severity of POST (2). Regarding other NSAIDs, gargling 350 mg of Aspirin reduced sore throat at two h after surgery. Intravenous Diclofenac did not affect reducing sore throat, but topical Diclofenac diminished the incidence of POST (3).
Studies have evaluated the effect of licorice, with the scientific name Glycyrrhiza glabra. This plant has been used in conventional and modern medicine due to its anti-inflammatory properties (10).
POST causes patient dissatisfaction and poor pain control. Several interventions could be performed to increase patient satisfaction and reduce sore throat, which may not be convenient for all patients, such as gargling or sprays (5). Use of different pharyngeal packs ( dry vs. wet/ saline soaked / tampons impregnated with lidocaine, normal saline, and chlorhexidine) was reviewed (7).
Zinc is a group IIb metal involved in various physiological activities such as growth, immune system, and tissue repair; it acts as an anti-inflammatory factor and prevents oral mucositis and chemotherapy-induced pain (3). And it was useful as lozenges in POST incidence (3).
It was reported that patients undergoing high-dose chemotherapy could benefit from gargling and swallowing zinc or taking it as a lozenge. Although, some patients refused to take zinc sublingual tablets due to their metallic taste. Moreover, this pill could cause side effects such as retching, vomiting, diarrhea, gastritis, and bowel inflammation (5).
2. Objectives
Despite advancements in anesthesia, postoperative sore throat continues to occur despite using some methods. As a primary outcome, this study compared the incidence of POST among all three groups. The secondary outcome was to evaluate the incidence of PONV among the studied groups.
3. Methods
This study was approved by the Ethics Committee of Guilan University of Medical Sciences with reference no. I.R.GUMS.REC.1398.429 on November 30, 2019. In total, 220 patients who were candidates for septorhinoplasty (class I or II according to A.S.A.) in Amir–Al Momenin Academic hospital under general anesthesia (G.A.) placed under endotracheal intubation (Inclusion criteria) were randomly included in this single-blind study. Exclusion criteria were those with a history of sore throat, URI (upper respiratory tract infections), those who had taken preoperative analgesia, drug abuse, and difficult intubation or having an allergy to zinc. The sample size required to compare the incidence of POST was divided into four groups. According to the study by Marais and Prescott (11), the confidence interval of 95% and the test’s power of 80% were determined to examine the significant difference between the groups (n = 55 per group).
1-
1-
Percentage of sore throat: Gauze (P1 = 54.5%); Control (P2 = 25%)
n = 31.8
The patients were randomly divided into four groups. The sampling method in this study was based on gradual reference, and the allocation of blocks was done by random allocation software. The anesthesia resident responsible for the participants' follow-up was unaware of the groups to which the patients belonged. But the anesthesiologist was aware of the groups of participants. After anesthesia and endotracheal intubation, normal saline- and zinc solution-impregnated pharyngeal gauzes were used for the first and second groups, respectively. Normal saline- and zinc solution-impregnated vibrils were applied to the third and fourth groups. The gauze used as the pharyngeal pack was prepared by Kaveh Bandage, Gauze and Cotton Co. (Iran) with the following characteristics:
- Gauze size 10 × 10 cm made of English thread 20/1
- Number of threads per square centimeter according to standard 3061
- Warp density per 10 cm according to standard 3061
- Weft density per 10 cm according to standard 3061
- The minimum diameter of gauze thread is 0.5 mm
The vibril used as the pharyngeal pack was prepared by Bandhaye Pezeshki Iran (B.P.I.) Vibril Manufacturing Company. The white and water-soluble zinc sulfate heptahydrate solution manufactured by Behsan Sar Company impregnated the gauze and vibril.
Vibrils were cut the same size as gauze. In order to prepare the pack, the gauze and vibril were placed in containers containing 0.9% normal saline and zinc sulfate heptahydrate solutions until they were uniformly impregnated.
The same anesthetic technique was employed for all the patients, i.e., all the patients received standard TIVA anesthesia with controlled hypotension (systolic blood pressure in the range of 90-95 mmHg). Intubation and pharyngeal packing were performed by the third-year anesthesiology resident who participated in the thesis. Participants were excluded from the study if more than two attempts were required for their intubation.
The standard size of the endotracheal tube was considered, i.e., tubes with diameters of 7 and 8 mm were used for female and male patients, respectively. The initial cuff pressure of the endotracheal tube was recorded during anesthesia. Cuff pressure was maintained at about 20-22 cm H2O. Number of laryngoscopy and blood on the laryngoscope blade were recorded at the end of the laryngoscopy.
The patient’s position and exact duration of surgery and anesthesia were recorded. At the end of the surgery, the oropharynx was aspirated with a 14 G green suction catheter (maximum twice). The patient was extubated and transferred to the recovery unit (PACU) in a conscious state and then immediately evaluated regarding the sore throat using the standard rating system presented by Farhang and Grondin. The POST severity was divided into four categories as follows (3):
0: Absence of sore throat
1: Mild discomfort expressed only by asking questions
2: Moderate sore throat self-reported by the patient
3: Severe sore throat causing voice changes and hoarseness
Assessments were performed after 0 (immediately), 2, 4, 6, and 24 hours post-operatively. Furthermore, they were performed by telephone for those patients discharged from the hospital before 24 h. PONV was evaluated by a verbal rating scale (VRS.), through which the patients reported their condition as none, mild, moderate, and severe. For a more accurate evaluation of PONV, the patients did not receive prophylactic medication for nausea and vomiting during surgery. Ondansetron 4 mg was used for the treatment in case of nausea and vomiting (12). And finally, age, gender, BMI (Body Mass Index), ASA class, Mallampati class, smoking status, POST at the studied times, and PONV at the same times were recorded.
3.1. Statistical Analysis
The data were analyzed using SPSS 21.0. The incidence and severity of POST were compared among the four groups by Chi-square and Kruskal-Wallis tests, respectively. The Bonferroni test was performed for pairwise comparisons. A p-value of less than 0.05 was considered statistically significant.
4. Results
In this study, 220 patients were divided into four groups. The mean age of the patients was 27.7 ± 7.9 years old (P = 0.537). The age frequency distribution was the same in the four groups, and no statistically significant difference was observed (P = 0.791). Most of the patients (84.5%) undergoing surgery were female. There was no statistically significant difference in the frequency distribution of gender among the four groups (P = 0.613). The mean body mass index (B.M.I.) was 24.2 ± 4 (mean ± SD). The mean B.M.I. (P = 0.197), as well as the status of BMI (P = 0.103), were the same in the four groups, and no statistically significant difference was observed in this regard (Table 1).
| Variables | Studied Groups | P-Value b | ||||
|---|---|---|---|---|---|---|
| Gauze + Normal Saline | Gauze + Zinc | Vibril + Normal Saline | Vibril + Zinc | Total | ||
| Age | 0.791* | |||||
| < 20 | 11 (26.19) | 12 (28.57) | 10 (23.81) | 9 (21.43) | 42 (19.09) | |
| 20 - 29 | 24 (26.37) | 21 (23.08) | 19 (20.88) | 27 (29.67) | 91 (41.36) | |
| 30 - 39 | 15 (23.44) | 16 (25.00) | 17 (26.56) | 16 (25.00) | 64 (29.09) | |
| > 40 | 5 (21.74) | 6 (26.09) | 9 (39.13) | 3 (13.04) | 23 (10.45) | |
| Total | 55 (25.00) | 55 (25.00) | 55 (25.00) | 55 (25.00) | 220 (100.00) | |
| Age | 0.535 # | |||||
| Mean ± SD | 27.29 ± 7.85 | 27.32 ± 7.85 | 28.93 ± 8.64 | 26.81 ± 7.34 | 27.67 ± 7.93 | |
| Highest, lowest | (17.0, 47.0) | (16.0, 45.0) | (16.00, 48.0) | (17.0, 44.0) | (16.0, 48.0) | |
| Gender | 0.613* | |||||
| Male | 11 (32.35) | 9 (26.47) | 6 (17.65) | 8 (23.53) | 34 (15.45) | |
| Female | 44 (23.66) | 46 (24.73) | 49 (26.34) | 47 (25.27) | 186 (84.55) | |
| Total | 55 (25.00) | 55 (25.00) | 55 (25.00) | 55 (25.00) | 220 (100.00) | |
| BMI | 0.103** | |||||
| Thin | 0 (0.00) | 1 (12.50) | 1 (12.50) | 6 (75.00) | 8 (3.64) | |
| Ideal | 34 (26.77) | 33 (25.98) | 30 (23.62) | 30 (23.62) | 127 (57.73) | |
| Overweight | 12 (18.75) | 16 (25.00) | 20 (31.25) | 16 (25.00) | 64 (29.09) | |
| Fat | 9 (42.86) | 5 (23.81) | 4 (19.05) | 3 (14.29) | 21 (9.55) | |
| Total | 55 (25.00) | 55 (25.00) | 55 (25.00) | 55 (25.00) | 220 (100.00) | |
| BMI | 0.197 # | |||||
| Mean ± SD | 24.79 ± 4.52 | 24.32 ± 4.09 | 24.61 ± 3.50 | 23.27 ± 3.76 | 24.26 ± 4.00 | |
| Highest, lowest | (18.59, 35.67) | (15.43, 39.54) | (18.00, 33.06) | (15.94, 33.06) | (15.43, 39.54) | |
a Values are expressed as No. (%) unless otherwise indicated. * Chi-square test; ** Fisher’s exact test; # One-way ANOVA.
b * Chi-square test; ** Fisher’s exact test; # One-way ANOVA.
Comparing the studied groups considering clinical factors indicated that 58.9% of the patients belonged to class II based on the Mallampati scale. However, according to the A.S.A. (American Society of Anesthesiology), most patients belong to class I. Only 5.5% had a history of Gastroesophageal Reflux Disease (GERD), and 15.1% were smokers. Also, 95.4% of the patients underwent laryngoscopy once. The frequency distribution of Mallampati (P = 0.349) and A.S.A. (P = 0.707) classes, GERD (P = 0.427), and smoking (P = 0.973) history and laryngoscopy (P = 0.401) was the same in the four groups, and no statistically significant difference was observed in this regard.
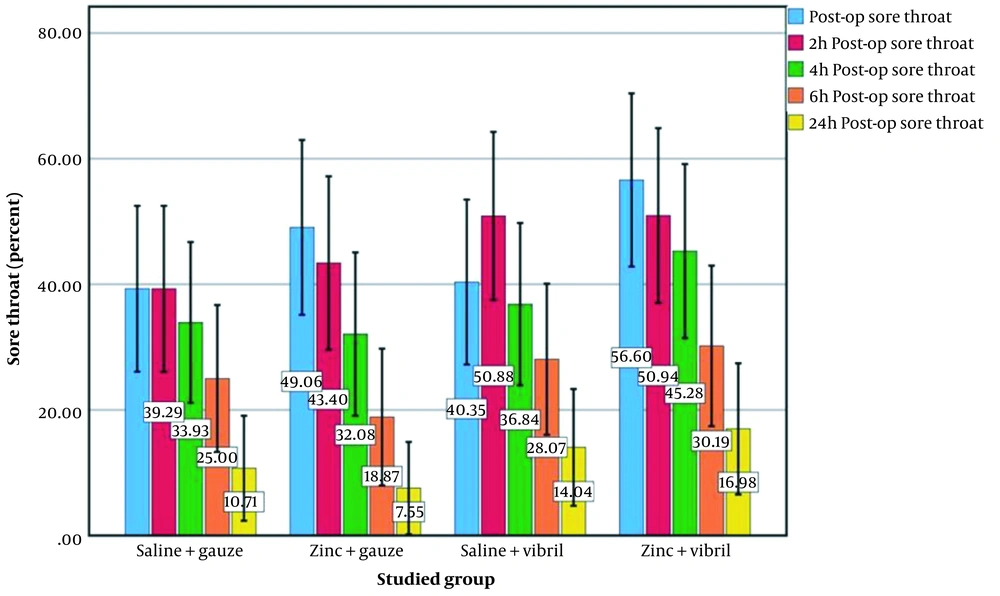
There was a significant difference in POST among the groups receiving gauze + normal saline (P < 0.001), gauze + zinc (P < 0.001), vibril + normal saline (P < 0.001), and vibril + zinc (P < 0.001) at 24 h postoperatively (Figure 1).
The highest incidence of sore throat was reported as 25% in the gauze + normal saline group at six h after surgery, 25.7% in the gauze + zinc group immediately after surgery, 29.6% in the vibril + normal saline group at 24 h after surgery and 33.3% in the vibril + zinc group at 24 h after surgery (Figure 1).
There was no statistically significant difference among the four groups in the sore throat immediately (P = 0.227), two h (P = 0.527), four h (P = 0.505), six h (P = 0.564), and 24 h (P = 0.481) after surgery. Moreover, the pairwise comparison results revealed no statistical difference between the groups receiving zinc and other groups.
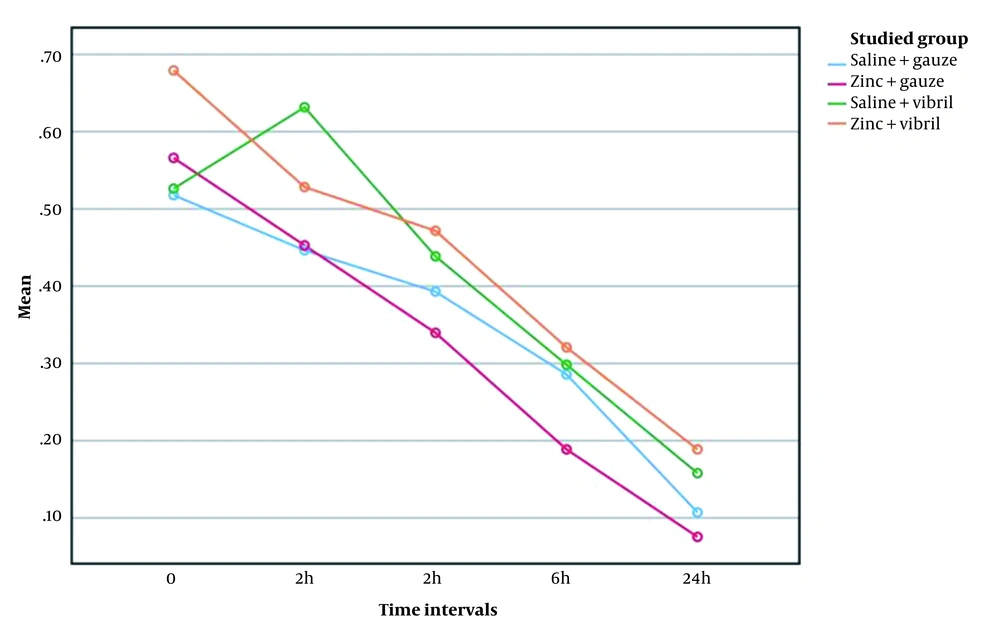
Comparing the severity of sore throat showed the highest mean severity was observed in gauze + normal saline and gauze + zinc groups immediately after surgery, vibril + normal saline group at two h after surgery, and vibril + zinc group immediately after surgery (Figure 2). Results of repeated measures ANCOVA test showed a significant difference in the severity of sore throat at 0 and 24 h after surgery. There was no statistically significant difference in the severity of sore throat among the four groups at 0 (P = 0.361), two h (P = 0.472), four h (P = 0.579), six h (P = 0.649) and 24 h (P = 0.465) postoperatively (Figure 2). The pairwise comparison results revealed no statistically significant dissimilarity between the groups that received zinc and conventional methods (P = 0.05).
As presented in Figure 2, the effect of time on sore throat was significant (P < 0.001).
However, the effect of the studied groups (P = 0.488) and the interaction of the studied groups with time (P = 0.562) was not statistically significant.
There was a statistically significant dissimilarity in PONV incidence among the groups receiving gauze + normal saline (P = 0.001), gauze + zinc (P < 0.001), vibril + normal saline (P = 0.001), and vibril + zinc (P < 0.008). A statistically significant difference was observed in the incidence of nausea at the studied times. The highest PONV incidence was reported as 20% and 30% in the groups receiving gauze + normal saline and gauze + zinc at four h after surgery, respectively, 55.6% in the vibril + normal saline group immediately after surgery and 31.3% in vibril + zinc group at six h after surgery. There was no statistically significant difference among the four groups in the incidence of PONV at 0 (P = 0.780), six h (P = 0.470), and 24 h (P = 0.999) postoperatively. A significant difference was observed in the incidence of nausea between the groups receiving gauze + zinc and gauze + normal saline at two h after the surgery (P = 0.045).
The incidence of nausea in the gauze + zinc group was almost twice that of the gauze + normal saline group (37.5% vs. 18.7%). There was a statistically significant difference between the vibril + zinc and gauze + zinc groups at this time. The incidence of nausea in the vibril + zinc group was about 20% lower than that in the gauze + zinc group (16.7% vs. 37.5%).
The severity of sore throat was evaluated in the four groups at the considered times, and the effect of the studied groups on the severity of sore throat was determined after controlling the effects of age, gender, A.S.A. class, Mallampati class, smoking status, and B.M.I. Results of repeated measures ANCOVA test showed the effect of adding zinc on reducing the sore throat was insignificant compared to the groups receiving the conventional method considering clinical and individual factors (P = 0.501, F = 0.789, DF = 3).
According to the partial eta-squared statistic, adding zinc's impact factor (IF) was very low (PE = 0.011). The results indicated the severity of sore throat was significantly correlated with gender (P = 0.021) and age (P = 0.002); however, other variables had no effect on the severity of sore throat. Women had more severe sore throats than men, and the severity of sore throats increased with age.
5. Discussion
POST and PONV are the most common complications reported by patients receiving general anesthesia. This study evaluated the effect of zinc as an anti-inflammatory drug. The sample size was determined to be 220 patients, which was almost similar to that of Meco et al.’s study in Turkey (n = 201) (13) and more than that of studies by Solmaz et al. and Naderian et al. and Basha et al. (n = 175, n = 120, and n = 100, respectively) (7, 8, 12). Most studies chose similar times for evaluating postoperative complications, i.e., 0, 2, 4, 6, and 24 h after surgery.
There were different pack types and added materials. Gauze packs (impregnated with normal saline and zinc) were compared with vibril packs (impregnated with normal saline and zinc), which were softer than sterile gauze. However, most studies examined either the presence/absence of the pack (12) or materials added to the tampon (8, 14).
Solmaz et al. and Basha et al. have found that applying a dry tampon without any anti-inflammatory or anesthetic agent increases the risk of POST. Naderian et al. reported that using packs during surgery reduced the incidence of a POST but had no effect on PONV (7, 8, 12).
In the present study, the severity of sore throat was significantly correlated with time. However, no significant correlation was observed between using zinc and the severity of sore throat in the studied periods. Results of repeated measures ANCOVA revealed that adding zinc to the severity of sore throat was insignificant compared to the conventional groups considering clinical and individual factors (P = 0.501, F = 0.789, DF = 3). Moreover, the severity of the sore throat was significantly correlated with gender (P = 0.0201) and age (P = 0.002); however, other variables had no impact on the severity of the sore throat. Women had more severe sore throats than men, and the severity of sore throats increased with age. The topical application of zinc had no impact on PONV.
There was no significant difference in the incidence of PONV at time 0 (P = 0.999) among the four groups. A statistically significant difference was observed in the incidence of nausea between the groups receiving gauze + zinc and gauze + normal saline two hours after surgery (P = 0.045).
The incidence of nausea in the gauze + zinc group was almost twice that of the gauze + normal saline group (37.5% vs. 18.7%). There was a statistically significant difference between the vibril + zinc and gauze + zinc groups at this time. The incidence of nausea in the vibril + zinc group was about 20% lower than that in the gauze + zinc group (16.7% vs. 37.5%). It could be argued that using vibril is probably more effective than sterile gauze in reducing PONV.
This study focused more on the effect of packing on sore throat after septorhinoplasty. Farhang and Grondin found that zinc tablets effectively diminished sore throat due to intubation in general anesthesia (3).
Sarkar and Mandal found that preoperative oral zinc tablets decreased the incidence of postoperative sore throat in the immediate postoperative period (15). But we concluded that applying topical zinc as a pack to the throat had no significant effect on reducing sore throat.
It could be concluded that applying softer materials such as vibril had at least a slightly higher effect on PONV than sterile gauze. However, further investigation should be conducted on POST, and other materials should also be examined.
5.1. Conclusions
Applying topical zinc as a soaked pack had no significant effect on reducing sore throat. However, a significant difference was observed in the incidence of PONV between the groups receiving zinc + gauze and gauze + normal saline at two h after surgery. Moreover, zinc and vibril significantly reduced PONV compared to the normal saline-impregnated gauze pack two hours after surgery.