1. Background
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in developed countries, contributing to disabilities, poor quality of life, and early death (1). In Iran, CVD is the most important cause of mortality, and 46% of all deaths are attributed to ischemic heart diseases (2). Restoring blood flow by CAB in a blocked coronary artery in the shortest duration is the main goal of treatment in patients with IHD (3). Postoperative pain is a complex process commonly caused by the stimulation of afferent neurons and central nervous system recognition induced by surgical trauma. It is one of the major concerns of patients undergoing heart surgery. Despite new techniques and modern analgesic treatments, postoperative pain is still one of the most important controversial issues (4). Many patients commonly tolerate moderate to severe pain after heart surgery (5-8). In a study, the results showed that 49%, 78%, and 62% of the patients had severe pain when resting, coughing, and moving, respectively, after CABG (6).
This pain can be caused by sternotomy, sternal retraction, chest tube, and aggressive procedures, such as removal of the saphenous artery and internal Mammillary artery. Moreover, performing endotracheal suction, coughing, and physiotherapy in ICU might be associated with a high degree of pain (9).
Pain may have a significant impact on pulmonary, endocrine, metabolic functions, and inflammatory responses to surgery. Inadequate control of postoperative pain may be accompanied by inappropriate outcomes such as tachycardia, increased oxygen consumption, hypercoagulability, pulmonary, and psychological complications. Proper pain control in patients undergoing heart surgery may accelerate patients recovery, improve sleep quality, reduce stress, decrease the duration of mechanical ventilation, reduce complications such as pneumonia and atelectasis, shorten the length of hospital stay, and reduce costs (10, 11). Management of the acute pain after surgery involves different health physicians, and various diets have been proposed for this purpose (9, 12-14). PRN medication is a common method in ICU patients that is usually based on intravenous route of opioid administration (7). Nowadays, long-acting opioids such as morphine are used as postoperative analgesics (15).
Great concerns regarding complications (respiratory depression, vomiting, etc.) and probable addiction are common reasons for nurses to limit the prescription of opioids. Furthermore, studies have shown that most nurses believe that cardiac surgery might not be very painful and incorrect estimation of pain might be the cause of insufficient analgesic prescription (16, 17)
The patient controlled analgesia (PCA) pump is an appropriate tool for pain control (12, 18, 19). Despite the acceptance and widespread use of pumps, and in spite of that it is a reliable analgesic method which may improve patients’ autonomy, reduce anxiety, and prevent personnel needle stick (12), yet there is a lot of controversies regarding the application of PCA pumps, and little information has been obtained about the use of this technique for heart surgery in Iran (18).
2. Objectives
Therefore, we aimed to compare the effectiveness of PCA pump and bolus morphine in controlling pain after CABG.
3. Methods
We conducted a randomized double-blind clinical trial in the anesthesiology research center of Guilan University of Medical Sciences in Rasht, Iran. Ethical approval was obtained from the ethics committee of GUMS and the study registered in the Iranian registry of clinical trials (IRCT) under the number IRCT2015012814359N3.
Inclusion criteria were 30 - 65 years of age, the American society of anesthesiologists class II-III, 3 vessel disease (3 VD), EF > 40%, no history of renal, liver, gastrointestinal, or pulmonary failure, no alcohol or drug addiction, and being scheduled for coronary artery bypass graft surgery under cardio pulmonary bypass pump.
Exclusion criteria were the pump time > 120 minutes, concomitant valve procedure and CABG, reoperation for controlling hemorrhage, and progressive heart failure (requiring high-dose postoperative inotrope or IABP).
The sample size was determined according to the following formula derived from the study by Guler et al. (20).
α = 0.05
β = 0.20
z1 - α/2 = 1.96
z1 - β = 1.28
s1 = 10.9
s2 = 16.2
µ1 - µ2 = 11.3
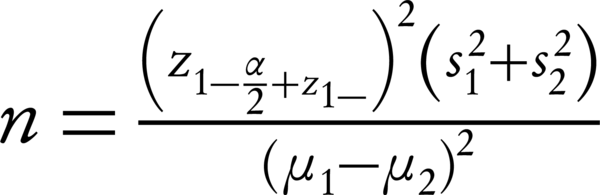
34 patients were designated for each group with the probable drop rate of 10%.
68 eligible patients were randomly allocated to either PCA group (P) or Bolus group (B) using randomized fixed quadripartite blocks. Our participants had an equal probability of being assigned to each of the two groups. The day before surgery, the type of surgery, anesthesia method, PCA pump and its method as well as visual analogue scale (VAS) criteria were explained at the bedside for patients by an anesthesiologist and informed consents were obtained from them. In order to make the study double blind, PCA pump was filled with morphine and normal saline in the group P and normal saline in the group B by a responsible anesthesiologist who monitored the patients and was aware of pump content. However, the patient and the investigator who recorded the data were blinded.
Patients were NPO for solid food from the night before surgery while they were allowed to consume soft drinks up to 2 hours before surgery. For premedication, 1 mg oral lorazepam was administered at both the night before surgery and an hour before transfer to the operating room. In addition, 0.1 mg/kg intramuscular morphine was given half an hour before transfer to the operating room. At the operating room, all patients underwent standard monitoring including 7 leads electrocardiography (ECG), pulse oximetry, blood pressure, and bispectral index (BIS). Before induction of anesthesia, the cardiac anesthesiologist inserted one peripheral venous catheter, left radial artery catheter, and central venous catheter under local anesthesia with lidocaine 1%.
Normal saline infusion was started at a rate of 5 - 7 cc/kg and all patients were pre-oxygenated with 100% oxygen for 3 minutes. Then, anesthesia was induced by 0.2 mg/kg etomidate premeditated by a low dose of this hypnotic agent (0.03 mg/kg) to blunt myoclonus (21) and sufentanil 1.5 µg/kg (during 10 minutes) followed by infusion of 0.2 mg/kg cisatracurium for muscle relaxation. After intubation, anesthesia was maintained by 50 - 75 µg/kg/min propofol, 0.2 µg/kg/h sufentanil, and 0.6 µg/kg/h atracurium. To maintain the preferred depth of anesthesia, BIS was preserved between 40 and 60 during surgery. Then, the patients underwent median sternotomy and a standard technique was used to establish the cardiopulmonary pump. Activated clotting time (ACT) was also measured following the administration of 300 µg/kg heparin. Cardiopulmonary bypass was initiated if ACT ≥ 480 seconds.
After the completion of the grafts and in case of stable vital signs, circulating heparin was antagonized by protamine, and the patient was separated from the pump. After the surgery, intubated patients were transferred to the intensive cardiac care unit to undergo mechanical ventilation. Sedation was established by infusion of 25 - 75 μg/kg/min propofol. The patients were extubated 6 - 8 hours after surgery based on the arterial blood gas analysis, clinical circumstances, and breathing status.
After the extubation in the group P, PCA pump including morphine (Silicone Balloon Infuser, Xinxiang City Tuoren Medical Device Co., China) with underlying infusion of 0.02 mg/kg/Qh, bolus dose of 1 mg, lockout time of 15 minutes and a maximum of 4 bolus of 0.02 mg/kg for one hour was administered. In the group B, PCA pump containing normal saline was established. During pump establishment for both groups, the existence of pain (VAS > 3) necessitated administering 0.02 mg/kg morphine as bolus while uncontrolled pain necessitated the second dose of bolus morphine, which could be continued to 4 times in an hour. For blinding in group B and P, the nurse pressed on the lockout interval bottom and respectively injected 0.02 mg/kg morphine and normal saline. Inappropriate response or existence of pain after administering appropriate dose of morphine required the administration of 15 mg/kg slow infusion of intravenous paracetamol (Cobel Darou Company). If the first dose of paracetamol did not control the pain and VAS > 3 was noted, NSAIDs such as 50 mg diclofenac suppositories would be administered. 4 hours after the first dose of paracetamol, the second dose could be administered. For both groups, pain was evaluated every 2 hours for the first 12 hours and every 4 hours for the remained 24 hours using VAS from score 0 (no pain) to 10 (the worst pain). Sedation score was determined based on the Ramsay sedation score (1: anxious, agitated, restless, 2: tranquil, cooperative, oriented, 3: responsive to commands only, 4: brisk response to light glabellar tap or loud auditory stimulus, 5: sluggish response to light glabellar tap or loud auditory stimulus and, 6: no response to light glabellar tap or loud auditory stimulus). Moreover, vital signs including blood pressure, heart rate, and incidence of complications such as hypoxia (O2 sat < 90%) and gastrointestinal complications were recorded. Adverse effects were treated as follows: pruritus with chlorpheniramine 10 mg IV, nausea and vomiting with ondansetron 4 mg IV, respiratory depression (respiratory rate less than 8/min) with naloxone 0.08 mg IV, hypotension (blood pressure decrease more than 20% of the baseline) with normal saline 5 mL/kg during 20 min, and dyspepsia with pantoprazole 40 mg every 12 hours. Finally, at the end of 24 hours stay in the ICU, the total amount of opioid (morphine) consumption in the two groups and the need for apotel and diclofenac were recorded.
3.1. Statistical Analysis
The collected data were entered SPSS version 17. The data were reported by descriptive statistics (number, percentage, mean, and standard deviation) and analyzed by chi-square test, independent T-test, Mann Whitney U test, and paired T-test. For intragroup comparison of variables after surgery, ANCOVA test was used. P value < 0.05 was considered statistically significant and 95% confidence interval was noted.
4. Results
Overall, 68 patients were enrolled of which, 3 patients were excluded. One patient in the group P and one patient in the group B were excluded due to bleeding that necessitated reoperation to be controlled. In addition, one patient in the group B was excluded due to requiring high-dose postoperative inotrope. Therefore, 33 and 32 patients participated in the groups P and B, respectively.
No significant differences were noted between the groups regarding age, sex, body mass index, cardiac output, duration of surgery, duration of pump, and aorta clamp time (Table 1). Assessing pain severity in the groups at different periods by T- Test showed a significant difference between the groups except at enrollment, and lower severity of pain was noted in the group P compared to the group B (P < 0.05) (Table 2 ). Results showed no significant difference between the groups regarding hemodynamic status in most periods (Table 3). In addition, there was no significant difference between the groups regarding sedation score (Table 4).
| Group P | Group B | P Value | |
|---|---|---|---|
| Gender (Male/Female) | 18/15 | 11/21 | 0.102 |
| Age, y | 56.72 ± 5.74 | 58.53 ± 5.52 | 0.202 |
| BMI | 25.48 ± 2.47 | 25.84 ± 1.73 | 0.508 |
| EF, % | 45.9 ± 3.78 | 47.28 ±3.98 | 0.16 |
| Operation time, h | 2.84 ± 0.39 | 2.89 ± 0.4 | 0.567 |
| Pump Time, min | 56.36 ± 8.59 | 57.03 ± 8.87 | 0.759 |
| Clamp Time, min | 37.12 ± 8.29 | 35.93 ± 9.19 | 0.587 |
Comparison of Demographic Characteristics in Groupsa
| Time | Group P Mean± SD | Group B Mean ± SD | P Value |
|---|---|---|---|
| T0 | 5.48 ± 1.09 | 5.28 ± 0.92 | 0.42 |
| T2 | 3.42 ± 1.1 | 4.06 ± 0.87 | 0.013 |
| T4 | 2.36 ± 0.65 | 3.25 ± 0.91 | 0.0001 |
| T6 | 2.06 ± 0.42 | 3.15 ± 0.8 | 0.0001 |
| T8 | 1.66 ± 0.59 | 2.68 ± 0.82 | 0.0001 |
| T10 | 1.27 ± 0.71 | 2.71 ± 0.72 | 0.0001 |
| T12 | 1.12 ± 0.73 | 2.43 ± 0.71 | 0.0001 |
| T16 | 1.09 ± 0.8 | 2.12 ± 0.6 | 0.0001 |
| T20 | 0.93 ± 0.7 | 1.59 ± 0.61 | 0.0001 |
| T24 | 0.69 ± 0.8 | 1.75 ± 0.62 | 0.0001 |
Comparison of Changes In pain Severity Based on VAS Score in Groupsa
| Time | Group P | Group B | P Value | ||
|---|---|---|---|---|---|
| Heart Rate** | Systolic Blood Pressure* | Heart Rate** | Blood Pressure* | ||
| T0 | 84.81 ± 11.91 | 120.87 ± 12.18 | 86.4 ± 8.54 | 120.21 ± 8.51 | 0.801*; 0.538** |
| T2 | 86.81 ± 10.46 | 124.0 ± 9.84 | 90.81 ± 8.04 | 121.03 ± 15.03 | 0.348*; 0.089** |
| T4 | 89.57 ± 8.05 | 119.57 ± 11.94 | 94.34 ± 9.64 | 125.93 ± 8.1 | 0.015*; 0.035** |
| T6 | 88.93 ± 13.99 | 121.21 ± 12.63 | 97.0 ± 13.78 | 125.65 ± 13.08 | 0.169*; 0.022** |
| T8 | 90.3 ± 8.42 | 121.21 ± 10.14 | 95.59 ± 11.39 | 122.0 ± 10.98 | 0.756*; 0.038** |
| T10 | 86.78 ± 10.7 | 120.72 ± 14.4 | 90.0 ± 12.41 | 122.31 ± 9.53 | 0.604*; 0.269** |
| T12 | 86.81 ± 11.91 | 121.12 ± 7.68 | 90.15 ± 13.38 | 121.53 ± 11.17 | 0.864*; 0.293** |
| T16 | 83.75 ± 10.92 | 119.12 ± 10.28 | 86.43 ± 8.80 | 118.0 ± 14.35 | 0.719*; 0.281** |
| T20 | 81.57 ± 8.05 | 117.42 ± 11.12 | 82.37 ± 10.86 | 119.65 ± 14.61 | 0.492*; 0.737** |
| T24 | 79.3 ± 10.99 | 116.33 ± 9.2 | 81.68 ± 7.41 | 118.28 ± 10.95 | 0.44*; 0.311** |
Comparison of Hemodynamic Parameters Between Groups
| Time | Group P | Group B | P Value |
|---|---|---|---|
| T0 | 1.78 ± 0.54 | 1.68 ± 0.64 | 0.501 |
| T2 | 1.93 ± 0.42 | 1.75 ± 0.67 | 0.183 |
| T4 | 1.72 ± 0.62 | 1.56 ± 0.56 | 0.269 |
| T6 | 1.841 ± 0.83 | 1.59 ± 0.49 | 0.14 |
| T8 | 2.15 ± 0.93 | 1.75 ± 0.62 | 0.051 |
| T10 | 1.96 ± 0.76 | 1.68 ± 0.64 | 0.114 |
| T12 | 2.03 ± 0.84 | 1.81 ± 0.73 | 0.273 |
| T16 | 2.06 ± 0.78 | 2.09 ± 0.68 | 0.857 |
| T20 | 1.96 ± 0.68 | 1.71 ± 0.52 | 0.101 |
| T24 | 1.84 ± 0.71 | 1.65 ± 0.54 | 0.226 |
Comparison of Change in Ramsay Score Between Groupa
Mann- Whitney U test showed a significant difference between the groups in terms of the mean consumption of morphine, diclofenac, and apotel after surgery. A higher morphine consumption in the group P and a higher diclofenac and paracetamol consumption in the group B were noted (P < 0.05) (Table 5). Using Fisher’s Exact test, the results showed that no statistically significant relationship was observed in the incidence of nausea, vomiting, gastrointestinal bleeding, and hypoxia between the groups at any periods of the study (P > 0.05). Although the complication rate was higher in the pump group, nausea occurred in 18.18% of the group P and 9.37% of the group B (P = 0.47). Moreover, vomiting was noted in 9.09% and 3.12% of the groups P and B, respectively (P = 0.613).
| Variable | Group P | Group B | P Value |
|---|---|---|---|
| Morphine, mg | 38.12 ± 2.36 | 17.12 ± 3.85 | 0.0001 |
| Diclofenac, mg | 28.78 ± 37.56 | 62.5 ± 47.51 | 0.003 |
| Paracetamol, g | 0.57 ± 0.75 | 1.25 ± 0.95 | 0.003 |
Comparison of Mean Consumed Morphine, Apotel, and Diclofenac Between Groups
Tree hypoxia in the group P was noted and there was no significant difference between the groups regarding saturation drop. No gastrointestinal bleeding was noted.
5. Discussion
Pain is described as an unpleasant feeling and emotional experience associated with actual or potential tissue damage. The stimulation of afferent neurons and activation of the autonomic nervous system and other reflexes by pain can cause endocrine metabolic responses and consequently induce organs dysfunction. Decreasing the pain can be a powerful technique to modulate surgical stress responses. Up to now, different pharmacological and non-pharmacological interventions have been carried out to control pain, inflammatory responses, and complications (9, 13, 14, 21-32). In addition, recent studies have examined different techniques of anesthesia to control inflammatory responses (33, 34). Induced pain during the first hours after cardiac surgery may be severe, requiring a high amount of analgesics. Thus, pain control and administering analgesics are needed to maintain the hemodynamic stability, decrease oxygen use by myocard, and prevent the ischemic situation after heart surgery (18, 35). The inappropriate control of pain may delay the recovery and exert long-term effects on the quality of life, all of which show the importance of pain control in these patients (35).
The use of PCA pump has been a way to control pain in recent years (18). Opioids are commonly used in pumps. Pharmaceutical effects of opioids are applied through the interaction between three types of opioid receptors (mu, delta, and kappa). These receptors can be found in the sites of periphery, pre-synaptic, and post-synaptic dorsal horn of the spinal cord, brain stem, and cerebral cortex with ascending transmission system and descending inhibitory pain systems that modulate pain at the spinal cord. Opioids cellular effects include reduced release of pre-synaptic transmitter, postsynaptic elements, hyperpolarization, and disinhibition. Among opioids, morphine (mu receptor agonist) is typically used in PCA pump and shows a relatively slow onset and long duration of action (36).
Our study showed that PCA pump of morphine compared to bolus of morphine could be a more effective pain controller especially in the early hours after extubation. Consistent with our results, the findings of a study by Lakdizaji et al. (18) showed that PCA pump controlled pain better than nurse-controlled analgesia (NCA) did. In contrast to the mentioned studies, Tsang and Brush (10) indicated no considerable preference for PCA pumps over other methods. It should be noted that they compared the methods on a sample of patients undergoing different surgical procedures (CABG and valve surgery) in a wider age range (< 75 years), both of which likely affected their results.
Studies have shown that age and gender are important factors that could affect pain and analgesic requirement after cardiac surgery. Patients aged > 65 years may have less pain compared to younger participants (7, 37). In our study, both groups had similar mean age and there was no significant difference between the groups regarding sex. Vaccarino et al. (37) investigated the effect of gender on recovery after CABG and found that women had harder recovery than men did after heart surgery. Therefore, sex and age can be effective in patient's pain. Therefore, in this study, there was no sex and age difference between the groups, which may affect patients’ pain and might increase the power of our study.
In previous studies, it was shown that by the use of underlying infusion in the PCA pumps, the use of narcotic drugs would increase. Our study showed a significant difference between the groups regarding the opioid use. The consumed amount of morphine was 38.12 ± 2.36 mg in the group P and 17.12 ± 3.85 mg in the B group and based on VAS, the pain especially after two hours of extubation was clearly lower in the group P. Guler et al. (20) mentioned that the consumed morphine rates in the pump group with underlying infusion and in the bolus pump group were 61 mg and 34 mg, respectively. The difference in the morphine consumption in our study compared to other studies might be because of administering maximum dose of morphine and the use of acetaminophen and diclofenac alongside morphine. Nevertheless, in a study by Dal et al. (38), the amount of morphine consumed was 32.8 mg in the pump group and 18.5 mg in the group receiving bolus of morphine, which were consistent with our results. Lakdizaji et al. (18) showed that consumed morphine was significantly higher in the pump group than in the group receiving morphine bolus (28.43 vs. 8.37). The lower dose of consumed morphine in their study compared to our study may be due to administering lower doses of morphine bolus (0.01 mg/kg) versus 0.02 mg/kg used in this study. However, Tsang and Brush (10) found no significant difference between PCA pump and other methods regarding the amount of used morphine. As mentioned before, different surgical procedures (CABG and valve surgery) and wider age range of patients might be considered effective factors.
In our study, although the amount of morphine was significantly higher in the group P, higher doses of diclofenac and paracetamol were administered to control pain in the group B. Paracetamol is a safe analgesic to control pain after surgery (9, 14, 15). Its analgesic effects commonly begin after 5 - 10 minutes and its half-life is about 1-4 hours. Results suggest that paracetamol is highly specific for cyclooxygenase 2 (COX-2). It is primarily metabolized in the liver to non-toxic products. Up to now, no complication has been reported by using opioid and non-steroidal anti-inflammatory drugs (NSAIDs) with paracetamol (15).
Investigations showed that using NSAID might decrease opioid requirement, thus reducing complications in many surgical procedures. NSAIDs act by blocking the peripheral synthesis of prostaglandins through inhibiting the cyclooxygenase 1 (COX-1) although a central mechanism has been recently proposed. Moreover, these drugs may block prostaglandin synthesis by inhibiting COX-2, which can cause platelet dysfunction. It also may lead to redistribution of blood flow in the kidneys and cause kidney failure and gastrointestinal symptoms (39). Regarding the noted concerns, it is not used widely for patients with coronary surgery although various investigations have assessed the effect of these drugs in heart surgeries (40). In this study, if morphine and paracetamol could not control pain, diclofenac would be used. In our study, the use of diclofenac was significantly higher in the group B than in the group P (P = 0.003) In addition, the consumption of paracetamol was significantly higher in the group B than in the group P (P = 0.003).
In this study, we compared hemodynamic changes in the two groups. Although heart rate was lower in the group P in different durations of assessment, no significant difference was noted in the most assessment periods. In addition, there was no significant difference between the groups regarding systolic blood pressure. However, during the first hours after extubation, blood pressure in the group P was lower. Lower heart rate and blood pressure might be because of better pain control in patients. This is because pain can increase blood pressure and heart rate by sympathetic stimulation.
Consistent with previous investigations, there was no significant difference between the groups regarding the level of sedation (18).
Respiratory depression, as the most important side effect of morphine PCA, may be more common (1.1 to 3.9% incidence) when a background infusion is added. Results showed that 20 µg/kg morphine could significantly increase complications including respiratory depression, sedation, vomiting, and nausea. However, a background infusion of morphine 0.5 mg/h did not induce significant respiratory depression after extubation in patients with cardiac surgery (38). In this study, 0.02 mg/kg/h morphine was administered as an analgesic drug in PCA pump and no significant difference was noted regarding respiratory depression. Guler et al. (20) mentioned no respiratory depression and hypoxemia by administering 0.03 mg/kg/h.
Regarding the occurrence of nausea in different periods, 3 patients in the group B and 6 patients in the group P had nausea, which showed no significant difference. Mota et al. (12) mentioned no significant difference between the groups regarding nausea and vomiting. Moreover, in our study, no gastrointestinal hemorrhage was observed, which was similar to Guler et al. study (20).
In this study, we assessed analgesic effect on patients after extubation, which may be a limitation. It is recommended to assess analgesic effect on extubation time. Since one of the most common complications of CABG is respiratory disease, paying enough attention to extubation and weaning off the mechanical ventilation are essential. Furthermore, post-operative problems can be associated with tracheal tube and mechanical ventilation. Hence, increased problems can induce higher risk of complications and increase duration of hospitalization and costs (41). In addition, further investigations on the effect of other opioid and non-opioid drugs on PCA pump and their analgesic effect are recommended to determine the most appropriate drug with the least complication.
5.1. Conclusions
Results showed that more morphine would be used in patients with PCA pump after extubation following heart surgery, and this increased dose of opioid was associated with better pain control and lack of complication. Therefore, PCA pump with underlying infusion could be effectively used in patients undergoing CABG directly assessed in ICU. Regarding the higher effectiveness of PCA pump compared to bolus morphine, it can be considered as a preferred method in coronary surgery; however, regarding the high dose of morphine administered in this method, it cannot be administered in other surgeries that do not require ICU stay; thus, further investigations are needed regarding other types of surgeries.
