1. Background
Postoperative nausea and vomiting (PONV) is common in post-anaesthesia care units (1). PONV prevalence in patients untreated with antiemetic medicines is about 30% (2), while fatigue originating from PONV is about 38% (3). Sometimes, the annoyance caused by PONV is more than the postoperative pain after asmall and ambulatory surgery. Therefore, PONVi n ambulatory operations may hospitalize the patient, which is economically important (4). The incidence of PONV after major gynaecologic surgeries is about 60% - 70% (5); in women undergoing gynaecological laparoscopy, it is 50% (6).
Laparoscopy is an ambulatory and semi-invasive surgery that is being increasingly used. The reasons for using laparoscopy include reduced post-operative symptoms, shorter hospitalization duration, and early recovery to normal activities. Women who undergo diagnostic gynaecological laparoscopy are usually young and healthy; therefore, they can tolerate variations in cardiovascular, respiratory, and endocrine activities caused by gynaecological laparoscopy (5).
To prevent or treat PONV, different drugs are used, such as Metocloperamide and Ondansetron (6). These drugs can cause side effects like drowsiness, hypotension, and extrapyramidal symptoms (1, 7). Non-pharmacological methods are also used, such as acupuncture, electrical stimulation of acu-points, acu-plaster, acupressure, and stimulation of PC6 (Neiguan), All of these methods have only minor side effects (6-8). Acupuncture is an effective non-pharmacological and non-invasive method for the reduction of PONV (9). Acupuncture has been practiced for thousands of years in clinical activities. However, scientific research is useful for the further application of acupuncture.
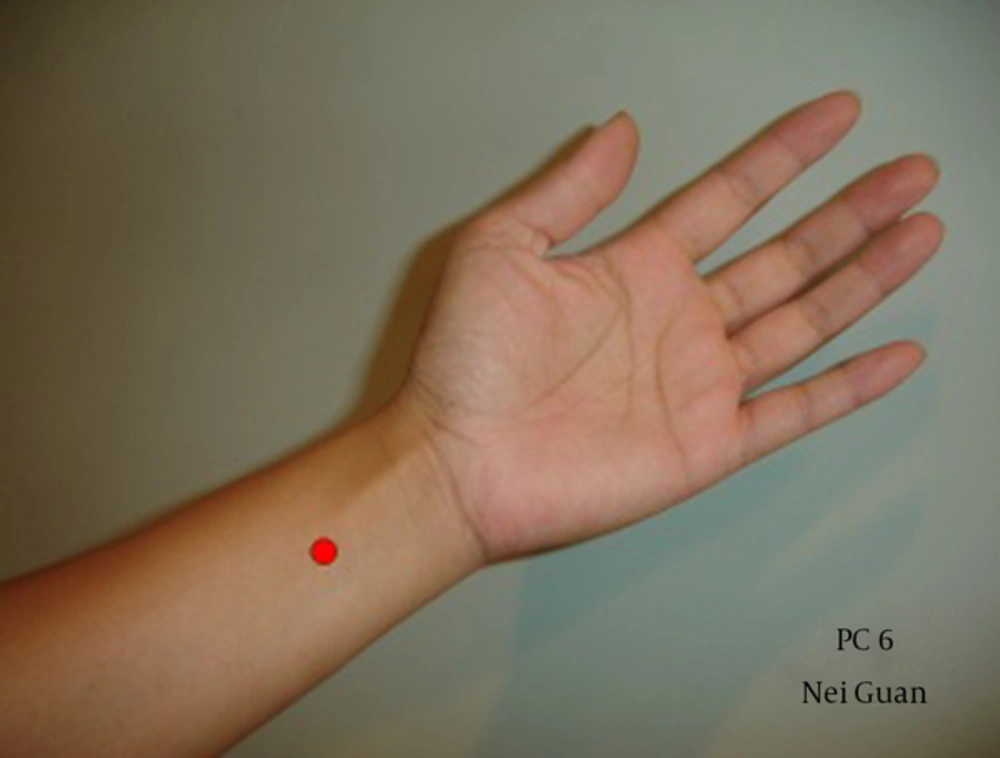
The Eastern Pacific regional arm of the world health organization (WHO) encourages member states to carryout research for evaluating the safety and effectiveness of traditional medicine (acupuncture and herbal) based on the principles and concepts of modern medicine (9). Acupuncture may relieve pain and treat some diseases, symptoms, and patients problems through the penetration of needles at determined points of the body (10). The location of PC6 is 2 cun above the wrist crease, between the tendons of palmaris longus and flexor carpi radialis (6, 10-12). The results of different studies show that acupuncture and acupressure at PC6 acupoint alleviate PONV in general after anaesthesia and caesarean section (13-18). It has also been reported that acupressure at P6 point reduces the incidence of PONV in the first three months of pregnancy (19). Most studies have been conducted in the field using acupressurein Iran (13, 14, 16, 19). Gynaecological laparoscopy is an outpatient surgery that requires patients to be discharged after a short time without any complications. Moreover, acupuncture has none of the side effects (like drowsiness, hypotension, and extrapyramidal symptoms) of antiemetic drugs. The literature review shows that there are very few studies comparing acupuncture and metoclopramide on PONV; even the few studies that have been conducted show conflicting results. No similar study in this field has been done in Iran.
2. Objectives
The aim of this study is to compare the effect of acupuncture and metoclopramide on PONV after gynaecological laparoscopy in Iran.
3. Methods
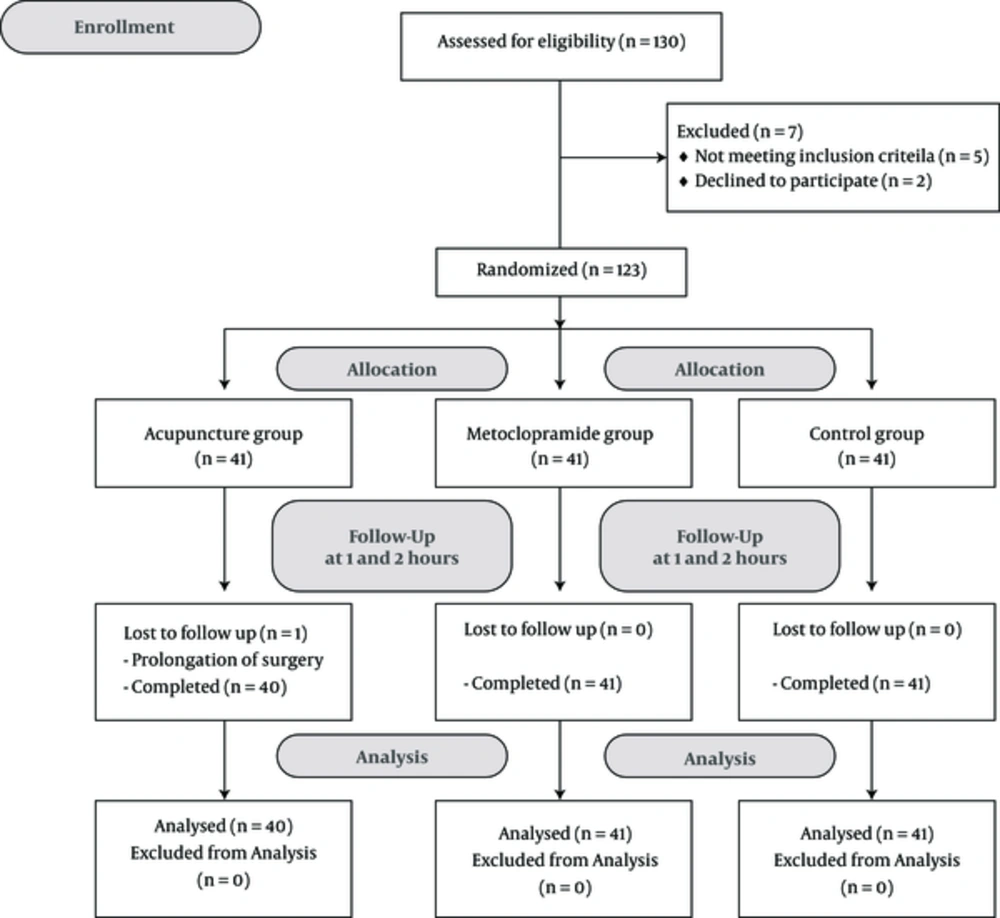
A double-blind, randomized clinical trial study was conducted at the Imam Khomaini hospital (General and referral hospital), Ahvaz, Iran. The study has been approved by the ethics committee of Ahvaz Jundishapur University of Medical Sciences (in compliance with the Helsinki declaration) and registered in the Iranian registry of clinical trials with the ID: IRCT2017012217268N4. Written informed consent was obtained from all patients. We enrolled 122 female patients who were candidates for gynaecological laparoscopy in order to compare the effects of acupuncture and metoclopramide on PONV, one and two hours after surgery.
The sample size was calculated by the following parameters: α error = 0.05; β error = 0.2; p1 = 30%; p2 = 27.5%.The sample size was calculated for each group, which comprised of at least 36 patients.
3.1. Patients
The eligible participants were candidates for gynaecological laparoscopy who met the inclusion criteria. The inclusion criteriastipulate that participants can be female patients with ASA I (American society of anaesthesiology), aged between 19 and 46 years. The exclusion criteria were as follows: smoking, history of motion sickness, obesity (BMI > 30 kg/m2), history of gastrointestinal disorder or ear diseases that may lead to nausea or vomiting, prolongation of surgery for longer than two hours, medication with antiemetic or antihistaminic medicines in the 24 hours before the surgery, occurrence of PONV in the preceding week, presence of scar or infection at the site of needling on the wrist or elbow and epileptics or patients receiving other drugs which are likely to cause extrapyramidal reactions.
3.2. Randomization and Blinding
Subjects were randomized into three groups- group I (acupuncture, n = 40), group II (metoclopramide, n = 41), and group III (control, n = 41)) using a computer-generated randomization list. In group I, acupuncture was done by inserting a special needle (sterile, with 0.25 mm diameter, length 25 mm) with depth 5 - 7 mm from skin at point P6 (Figure 1) in front of the elbow immediately after induction of anaesthesia and removing it before extubation and transfer of the patient to the recovery room. In group II, metoclopramide 0.2 mg/kg (IV) was administered immediately after induction of anaesthesia. In the control group, we did not use medicine or anything else to prevent nausea and vomitingonly normal saline (1 mL/IV) was used as placebo.
The physicianswho conducted the intervention were different from the anaesthetists who examined the patients for frequency of nausea and vomiting. The examiner was not aware of the intervention. All interventions, including acupuncture, injection of metoclopramide and normal saline, were done after the induction of anaesthesia. Thus, the patients were unconscious during the intervention. Therefore, the trial was double-blinded (Figures 2 - 6).
3.3. Study Protocol
The aim of this research was explained to the patients and their entourage before the surgery. Patients joined the study after signing the informed consent form. For all patients, we took note of the age, BMI, and duration of surgery. The vital signs, including systolic and diastolic arterial pressure, pulse (heart rate), SaO2, and End-Tidal CO2, were monitored before and during anaesthesia. All patients were pre-medicated with 1 mg of Midazolam and patients fasted for at least eight hours prior to the surgery. Thiopental (5 - 7 mg/kg), Atracurium (0.6 mg/kg), and Fentanyl (1 µg/kg) were administrated for the induction of anaesthesia. After intubation, anaesthesia was maintained with 1 MAC in 50% N2O-O2 with controlled ventilation. The effects of neuromuscular blockers were reversed using Prostigmine (0.05 mg/kg) and Atropine (0.025 mg/kg).
For patients in the acupuncture group, acupuncture was performed by inserting a special needle (sterile with 0.25 mm diameter, length 25 mm) with depth 5 - 7 mm into skin at point P6 (Figure 1) in front of the elbow immediately after induction of anaesthesia and removing it before extubation. Then the patient was transfered to the recovery room. The location of PC6 is 2 cun above the wrist crease, between the tendons of palmaris longus and flexor carpi radialis. The “cun” is the standard unit of measurement for the body used in acupuncture, where 1 cun = width of the thumb, in the middle, at the crease. One cun is also equal to the space between the distal interphalangeal joint and the proximal interphalangeal joint on the middle finger (9). A trained acupuncturist inserted needles at the P6 point of both forearms, rotate them and stimulate of P6 point for five second, and then kept them in placeup to end of surgery. Needles were removed before patients awoke. There was no side effect in patients receiving acupuncture.
Those who had complexity that needed special anaesthesia or needed special medication during anaesthesia were excluded from the study (patients with special disease are prescribed long-term drug treatment that maybe interactions with anaesthetic agents and result in increased anaesthetic requirements). In the recovery room, all patients were monitored and immediately treated by metoclopramide (10 mg i.v) if they experienced vomiting. For postoperative analgesia, all patients received 100 mg sodium diclofenac suppository immediately after arrival to the recovery room.
3.4. Assessment
The occurrence of nausea and vomiting during the period of stay in recovery room (one and two hours after surgery) were recorded through questioning or clinical observation by an anaesthesia assistant who did not know the trial technique. The following definitions were used. Nausea: an uneasiness of the stomach that often precedes vomiting without muscle spasms; vomiting: an uncontrollable reflex that expels the contents of the stomach through the mouth.
3.5. Statistical Methods
Statistical analysis was conducted with SPSS V. 19. By using descriptive statistics, the mean and standard deviation of demographic data (age, BMI, duration of surgery) were calculated. The incidences of nausea and vomiting were recorded as frequencies (n) and percentages (%). In this study, to compare the incidence of nausea and vomiting between the threegroups, Chi-squared or Fisher’s exact tests were applied. P < 0.05was considered the significant level.
4. Results
Patients were compared in terms of age, BMI, duration of anaesthesia and duration of surgery in three groups. In this study, no statistically significant difference between the groups was found with regard to demographic data (Table 1).
| Acupuncture (n = 40) | Metoclopramide (n = 41) | Control (n = 41) | P Value | |
|---|---|---|---|---|
| Age, y | 26.44 ± 9.13 | 25.68 ± 8.32 | 27.06 ± 9.51 | 0.76 |
| BMI, kg /m2 | 22.1 ± 1.52 | 21.7 ± 1.44 | 22.3 ± 1.35 | 0.85 |
| Duration of anesthesia, min | 95 ± 11.12 | 100 ± 13.15 | 92 ± 12.14 | 0.54 |
| Duration of surgery, min | 72 ± 14.63 | 75.30 ± 17.25 | 71.30 ± 19.11 | 0.63 |
aValues are expressed as mean ± SD.
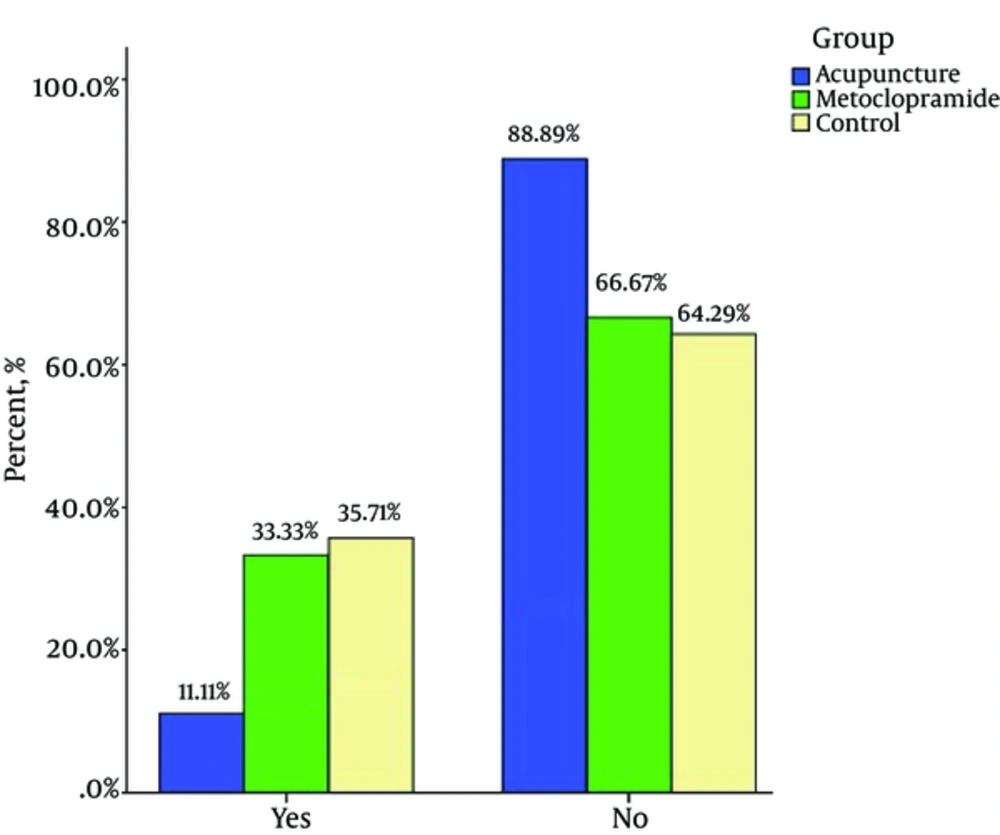
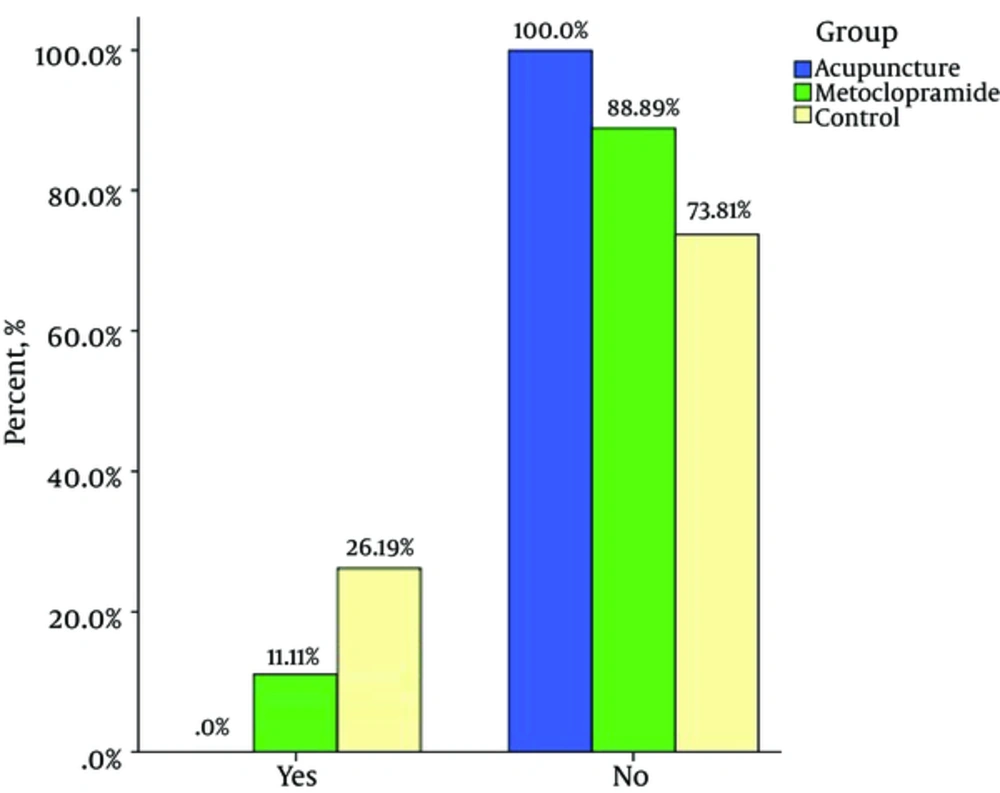
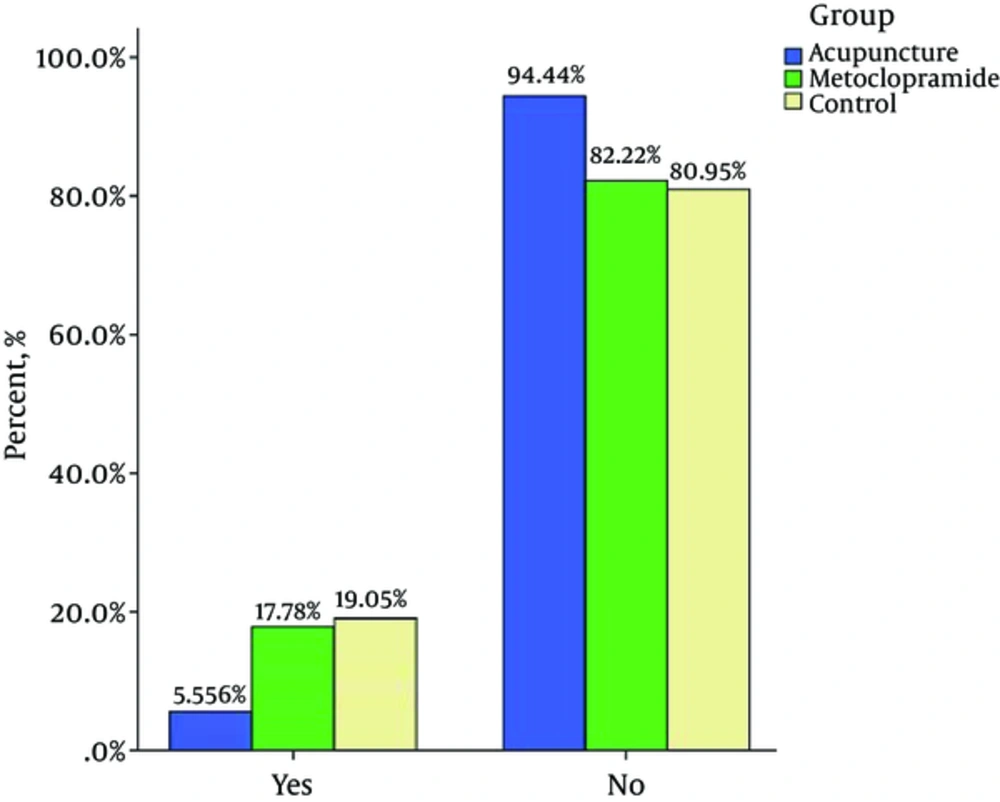
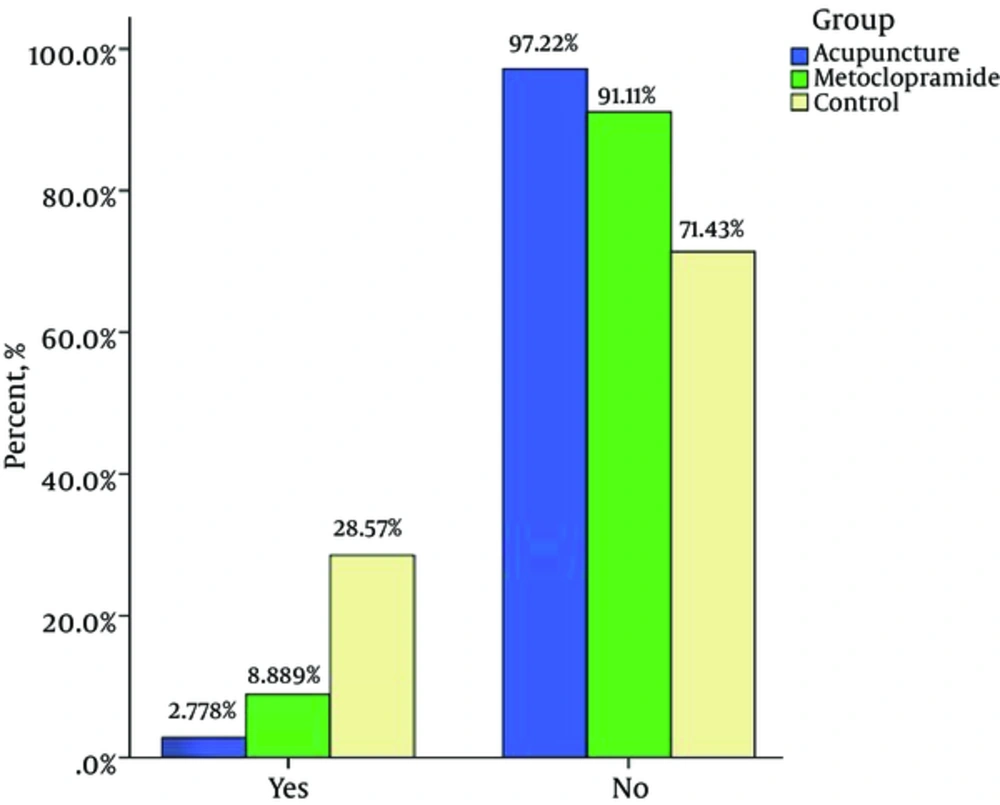
In the present study, the incidence of nausea one hour after surgery was 35.7%, 33.3%, and 11.1% (P = 0.03)* and two hours after surgery was 26.1%, 11.1%,and 0% (P = 0.003)* in control, metoclopramide, and acupuncture groups respectively (lowest incidence in the acupuncture group). The incidence of vomiting one hour after surgery was19%, 17.7%, and 5.5% (P = 0.18* and two hours after surgery was 28.5%, 8.8%, and 2.7% (P = 0.002) * in control, metoclopramide and acupuncture groups respectively (Table 2) (Lower incidence in the acupuncture group). In this study, it was noted that the acupuncture group showed a significant decrease in the incidence of nausea onehour after surgery compared to the metoclopramide group (P < 0.05), but two hours after surgery there was no significant difference. A comparison between the acupuncture and metoclopramide groups proved no significant difference between the acupuncture and metoclopramide groups in terms if postoperative vomiting (POV) incidence one and two hours after surgery (Table 2).
aValues are expressed as No. (%).
bP value of am = acupressure to metoclopramide; P value of ac = acupressure to control; P value of mc = metoclopramide to control.
c1 hour after surgery.
d2 hour after surgery.
We did find a significant decrease in the incidence of postoperative nausea (PON)oneand two hours after surgery, between the acupuncture and control groups (P < 0.05), but there was no significant decrease between the acupuncture and control groups in the incidence of vomiting one hour after surgery; however, the difference two hours after surgery was significant (Table 2).
Furthermore, in the present study, no significant differences between the metoclopramide and control groups were found in the incidence of nausea one and two hours after surgery. Similarly, no significant differences were found between the metoclopramide and control groups in the incidence of vomiting one hour after surgery; However, the difference two hours after surgery was significant (P < 0.05) (Table 2).
5. Discussion
The present study was designed to compare the effects of acupuncture and metoclopramide on PONV after gynaecological laparoscopy (one and two hours after surgery). Our study results indicate that the stimulation of P6 acupoint reduces the incidence of PONV to a greater extent compared to metoclopramide and no intervention. PONV and the need for antiemetic treatment is reduced with the stimulation of P6 acupoint (17, 18). Reduction in PONV and the need for antiemetic drugs with acupuncture in P6 acupoint may decrease costs such as antiemetic drug cost and length of stay in hospital and may also improve patient care quality (17, 18). In the present study, the incidence of nausea an hour after surgery was35.7%, 33.3%, and 11% and two hours after surgery was 26.2%, 11.1%, and 0% in the control, metoclopramide, and acupuncture groups respectively (lower incidence in the acupuncture group). Moreover, the incidence of vomiting one hour after surgery was19%, 17.8%, and 5.6% and two hours after surgery was26.2%, 8.9%, and 2.8% in the control, metoclopramide, and acupuncture groups respectively (lowest incidence in the acupuncture group). These findings are in accordance with a number of previous studies, which showed a lower incidence of PONV in acupuncture and acupressure groups (P6 point stimulation) compared to metoclopramide and control groups after various types of surgery (20-22). Streitberqer et al. conducted a randomized, placebo-controlled, patient- and observer-blinded trial to determine whether acupuncture at the point P6 is effective in preventing PONV compared to placebo acupuncture. The difference between acupuncture and placebo for patients after gynaecological surgery was significant (P = 0.07). Also, the results of this study confirm our study results (23). Ouyang et al. carried out a study in China to explore the prophylactic effect of stimulation of P6 acupoint on PONV laparoscopic surgery. They randomly divided 100 patients into an acupuncture group and a control group. Patients were observed at 6 hours, 12 hours, 24 hours, and 48 hours to record the incidence rate of nausea, retching, and vomiting. Results showed that the incidence rate of nausea and retching in the acupuncture group were lower than those in the control group. They concluded that acupuncturing PC6 can reduce the incidence rates of nausea and retching after laparoscopic operation, especially in 24 hours. This study also confirms our study results (24). Kim et al. conducted a study on 264 patients who had undergone laparoscopy hysterectomy and were being evaluated for PONV. In this study, the effects of some neuromuscular monitoring modes such as single twitch (ST), train-of-four (TOF), double-burst stimulation (DBS), and tetanus were evaluated at the P6 acupoint for PONV. They found that sixhours after the stimulation of titanic, incidence of PONV was significantly reduced (P = 0.022), as were the number of patient-controlled analgesia (PCA) requests (P = 0.009) and total PCA volume (mL) (P = 0.042) in the treatment group compared tothe control group. Moreover, patients of the tetanus group were more satisfied with PONV management compared to patients of the control group. The results of this study confirm the results of our study (25). Lee et al. carried out a study titled ‘Electroacupuncture on PC6 prevents opioid-induced nausea and vomiting after laparoscopic surgery’ on 178 patients, who had received PCA with Fentanyl (IV) and were divided randomly to three groups using random number tables: preoperative electro-acupuncture (PrEA), postoperative electro-acupuncture (PoEA), and non-acupuncture control (NC). This study shows that PC6 electro-acupuncture is effective in the prevention of PONV and PrEA is more effective than PoEA. The present study shows that preoperative acupuncture at the PC6 point reduces PONV after surgery (26). In the study by Yang et al. 157 women who underwent elective gynaecological laparoscopic surgery were assigned into three groups: Group Acu (electroacupuncture combined with dexamethasone), Group Trp (tropisetron combined with dexamethasone), and Group Dxm (only dexamethasone). PONV prophylactic effect of electroacupuncture or tropisetron combined with dexamethasone was found to be more effective than dexamethasone alone in women who had undergone gynaecological laparoscopic surgical operation (27). Seevaunnamtum et al. investigated the effect of intraoperative electroacupunctureon the prevention of PONV in 64 female patients undergoing gynaecological surgery. The results of this study reveals that the incidence of PONV was reduced in the electroacupuncture group compared to the control group (28).
We did find significant decrease in the incidence of PON one and two hours after surgery between acupuncture and control groups. Our results confirm previous study findings, which revealed that the stimulation of P6 acupoint was effective in reducing the incidence of PON (4, 29). Fry et al. investigated the effectiveness of acustimulation of PC6 on attenuating PONV. They studied 200 patients undergoing laparoscopic cholecystectomy. Results showed that the incidence of nausea two hours after surgery (early nausea) was significantly less in the acustimulation group (29%) than in the sham group (42%); (P = 0.043). The results of this study also are similar to our findings (30).
Despite the lower incidence of PONV in the acupuncture group compared to the metoclopramide group, no statistically significant difference was found among the acupuncture and metoclopramide groups in PONV except a significant decrease in the incidences of nausea one hour after surgery (P = 0.027).
Butkovic et al. compared three groups: Group І (laser acupuncture on PC6 acupoint + saline infusion, Group ІІ (metoclopramide 0.1 mg/kg (IV) + sham laser), and Group ІІІ (sham laser + saline infusion). There was a statistically significant difference between the control group and other groups, but there was no difference between the laser acupuncture and metoclopramide groups. The results of this study are similar to that of our study (31). Leeshows that there is no significant difference between acupuncture on the PC6 point and antiemetic drugs to prevent PONV (32). Saleh performed a double-blind investigation on 60 patients who underwent strabismus surgery and found no statistically significant difference between the acupuncture group and ondansetron group in PONV at any time (1 - 12 hours) (33). Soltani et al. carried out a placebo-controlled study on 200 patients undergoing strabismus surgery and revealed that the incidence of PONV was not significantly different between acupressureat P6 point, metoclopramide, and ondansetron groups in the recovery ward (24 hours after surgery) (34).
Yang (27) in his study compared effect dexamethasone alone vs in combination with transcutaneous electrical acupoint stimulation for prevention of postoperative nausea and vomiting in gynaecological patients undergoing laparoscopic surgery but in present study compare the effects of acupuncture and metoclopramide on post-operative nausea and vomiting (PONV) after gynaecological laparoscopy.
In Yang et al. study (27) incidence of nausea, vomiting and need for rescue antiemetics was recorded 2, 6, 24, and 48 hours after surgery. In Frey et al. study (30) incidence of nausea and vomiting was recorded 2, 6, 24 hours after surgery. In present study incidence of nausea and vomiting was recorded 1, 2 hours after surgery. Perhaps, if a longer time had been spent for the therapeutic method (acupuncture) and was longer follow up time, better results would have been obtained.
The present study, Yang et al. (27) and Lee et al. study (26) conducted three groups and were double-blind. The present study and Lee et al. study (26) one group is considered as the control group that received no drug treatment while in Yang study (27) all 3 groups received dexamethasone at least. Ouyang et al. study (24) was conducted in two groups (acupuncture/control).
In Lee et al. (26) and Frey et al. study (30) acupuncture is performed both pre-operative and post-operative while in present study, Yang et al. (27) and Ouyang et al. (24) study acupuncture is performed pre-operative. In Lee study was concluded pre-operative acupuncture is more effective than post-operative acupuncture. But in Ferry study (30) were shown timing of (pre and post- operative) acustimulation had no significant effect on PONV reduction.
In Ferry study (30) stimulation at the point p6 was performed through the active ReliefBand device while in present study stimulation at the point p6 was performed through traditional acupuncture (through a needle).
Butkovic study (32) is similar present study. Both studies compared the effects of acupuncture and metoclopramide in prevention PONV after surgery. But presnt study sample comprised adult women undergoing gynaecological laparoscopy wihle Butkovic study (31) sample comprised children undergoing hernia repair, circumcision or orchidopexy. In Butkovic study laser acupuncture were used while in present study traditional acupuncture (through a needle) were used. The difference between present study and other studies is effective on the results.
It has also been suggested that α- and β-fibres, which make synapses in the dorsal corona, are activated via sensory receptors of the skin and cause a low-frequency stimulation, terminating the increase in the secretion of endorphins in the hypothalamus. An augmentation of the cerebro-spinal fluid level of β-endorphin following acupuncture has been demonstrated (35, 36). Alternatively, it has been proposed that this technique activates the serotonergic and norepinephrinergic fibres and possibly changes in the serotonin levels, which have a preventive effect on PONV (35, 36).
Conclusions
Acupuncturing p6 point reduced PONV incidence rate in gynaecological laparoscopy compared to the control group. Though there was no statistically significant difference between the acupuncture group and the metoclopramide group, subjects receiving acupuncture experienced less PONV compared to subjects in the metoclopramide group. Hence, acupuncture is effective method for reduction of PONV after gynaecological laparoscopy. It has no side effects and is economically affordable.
Suggestions and limitations
Results restricted to female gender and a short follow up time was the reason that your findings could not generalized to whole population. It is suggested that a study be carried out on both genders and longer follow up time.