1. Background
Postpartum hemorrhage (PPH), or excessive bleeding at or after childbirth, is a potentially life-threatening complication of both vaginal delivery and cesarean section (C-section) and is one of the leading causes of maternal morbidity and mortality worldwide (1), with a prevalence of 6% of all deliveries (2). The effects on maternal morbidity include fatigue, Sheehan’s syndrome, anemia, coagulopathy, and shock (3, 4). It is noteworthy that it contributes to almost half of all the postpartum maternal mortality (5); nevertheless, Hanson et al. revealed a PPH case fatality rate of 2.13% (6). The most common cause of PPH is uterine atony; therefore, it has been recommended to actively manage the third stage of labor (7, 8).
Oxytocin is recommended as the standard treatment for PPH (9). A previous Cochrane review deduced that syntometrine (oxytocin/ergometrine) is related to a considerable decrease in the PPH risk for loss of blood, which exceed 500 mL but not 1,000 mL when compared to using oxytocin alone. However, the side effects of syntometrine as nausea, vomiting, pain, and hypertension (with a high incidence of 20 - 30% in Western countries (10, 11)), retained placenta (12), coronary artery spasm (13), and intracerebral hemorrhage (14). These side effects are mainly due to the ergometrine component. Although the hemodynamic changes after either oxytocin alone or syntometrine could be well tolerated in healthy patients, they cannot be used in a significant proportion of the obstetric population due to coexisting comorbidities, such as preeclampsia and cardiac diseases. Many alternatives, such as prostaglandins, were offered. However, another review concluded that intramuscular prostaglandins are not preferable to conventional injectable uterotonics as part of the active treatment of the third stage of labor (15).
Carbetocin, an oxytocin derivative, has a four- to ten-times longer half-life than oxytocin and is thought to reduce the need for additional oxytocin (16). Clinical trials comparing the contractile action of oxytocin and carbetocin showed comparable adverse effects for the two drugs (17). Carbetocin produces a longer uterine response when given following childbirth regarding contractions’ amplitude and frequency. Carbetocin’s lack of relative gastrointestinal and cardiovascular side effects should confirm its recommendation to be used in comparison to Syntometrine and other ergot alkaloids (18). However, there is not enough clinical information regarding the hemodynamic side effects of carbetocin. Due to their use as a prophylactic treatment and the rising concern of high-risk parturients either due to pre-existing or pregnancy-related cardiovascular diseases, it is essential to investigate the hemodynamic profile of both drugs.
2. Objectives
This study aimed to compare carbetocin and oxytocin hemodynamic effects in preeclamptic patients undergoing an elective C-section under spinal anesthesia in a randomized, double-blind, controlled trial (RCT).
3. Methods
3.1. Ethical Statement
The present study was carried out at the Hospital of Beni-Suef University, Beni Suef Governorate, Egypt, after obtaining approval from the Department of Anesthesia and Committee of Local Ethics of Faculty of Medicine, Beni-Suef University, on May 21, 2017. Written informed consent was obtained from all trial participants, and the study period was extended from September 25, 2019, to January 20, 2020. The trial was registered at the Pan African Clinical Trial Registry (www.pactr.org, PACTR201909623653208) on September 23, 2019, before the start of recruiting patients. All methods were conducted according to the relevant approved regulations, guidelines, and declaration of Helsinki.
3.2. Sample Size Calculation
A sample size of 40 patients in each group was determined to achieve 80% power to detect a difference between the group proportions of 0.31 (odds ratio of 4.4) regarding BP. The proportions in group I were assumed to be 0.5 and 0.81 under the null and alternative hypotheses, respectively. The proportion in group II was 0.5. The two-sided Fisher’s exact test was used as a test statistic. The test was designed to have a significance level of 0.05. This design achieved a significant level of 0.03.
3.3. Study Design
In this single-center, prospective, randomized, double-blind study, the subjects were randomly allocated into two groups using a technique of sealed opaque envelope. The first group included the subjects receiving oxytocin (Syntocinon Novartis Pharmaceuticals Ltd., Switzerland) 5 IU as an intravenous bolus over 10 seconds in 10 mL 0.9% NaCl solution (18, 19). Nevertheless, the second group included the subjects receiving carbetocin (Pabal, Ferring pharmaceutical Ltd., Switzerland) 100 μg as an intravenous bolus over 10 seconds in 10 mL normal saline solution (18-20). Both drugs were prepared exactly 5 minutes before the C-section and were handed to an anesthesiologist.
3.4. Eligibility Criteria
This study included pregnant women with preeclampsia criteria undergoing elective C-section at term pregnancy with regional (spinal) anesthesia (i.e., mild preeclampsia). Preeclampsia was diagnosed if a woman was pregnant for > 20 weeks with BP ≥ 140 mmHg systolic or ≥ 90 mmHg diastolic with urine protein: creatinine of 30 mg/mmol (according to the National Institute for Health and Care Excellence guidelines). Of note, magnesium sulfate was not used for any patient because they were mild preeclamptic. The exclusion criteria included women with regional anesthesia refusal, regional anesthesia contraindications (e.g., coagulopathy diagnosed by the coagulation profile), conditions associated with an increased level of PPH risk, such as placenta previa, placental abruption, and multiple gestation, pregnancy-related complications as gestational diabetes, or pre-existing diseases as insulin-dependent diabetes, cardiovascular or renal diseases, and/or hypo/hyperthyroidism because these conditions might interfere with the hemodynamic parameters. Mild cases were only included since the vessels were less hypertrophied and spastic, with generally better response to vasodilators. Moreover, the vascular reactivity was better preserved in mild than severe cases.
3.5. Assessment Parameters
The primary outcome was BP, including mean BP, systolic blood pressure (SBP), and diastolic blood pressure (DBP). This study also evaluated other hemodynamic effects, such as the HR and O2 saturation before the operation and after 1, 5, 10, and 15 minutes, symptoms of myocardial ischemia (e.g., chest pain, shortness of breath, and/or feeling of heaviness in chest pain), and incidence of hypotension (defined as BP < 90/60 mmHg) following drug administration. In addition, this study assessed the intraoperative use of ephedrine (after the administration of the study drugs), the patients’ number who required an additional carbetocin or oxytocin dose, the PPH incidence (defined as the loss of more than 500 mL of blood), the amount of blood loss, and postoperative hemoglobin.
All patients had a preoperative full history taking and examination. On arrival at the operating theatre, continuous monitoring of electrocardiogram, noninvasive arterial BP, and pulse oximetry was carried out. An intravenous cannula was inserted, and fluid preload (lactated ringer solution 10 mL/kg) was administrated. In contrast, an intra-arterial cannula was inserted under local anesthesia in the radial artery of the non-dominant hand.
Spinal anesthesia was performed under strict aseptic technique in the sitting position at lumbar levels L3 - L4 or L4 - L5 space, with 3 mL heavy bupivacaine 0.5% (15 mg), and the patients were put in the supine position with left uterine displacement supplemented with oxygen 3 L/minute. The blood loss was estimated by soaked towels and blood in suction.
3.6. Statistical Analysis
The kurtosis and skewness tests were used for testing the continuous variables’ normal distribution. Student’s t-test was used for the normal distribution of continuous variables; however, the Mann-Whitney U test was used for continuous variables not normally distributed. A paired t-test was applied for the intragroup comparison of the mean values from preoperative to different intervals for each group of the interventions separately. Moreover, intergroup comparison (i.e., oxytocin group vs. carbetocin group) was performed to compare the mean values (i.e., the pre-intervention mean value and the mean of each interval of 1, 5, 10, and 15 minutes). SPSS software (version 17) and RStudio software (version 3.2.4) were used to analyze the data. The results were considered significant with P < 0.05.
4. Results
4.1. Patients’ Characteristics
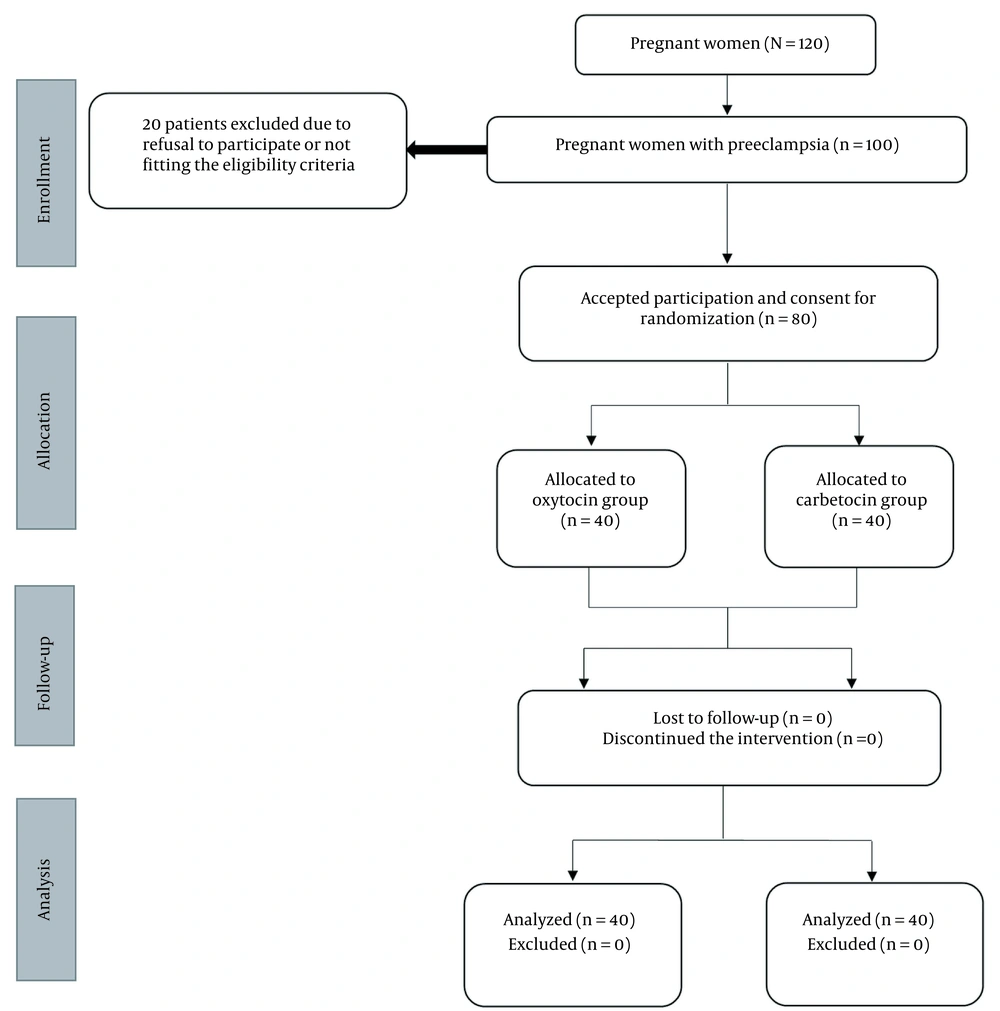
Out of 120 women screened for inclusion, this study enrolled 80 women with preeclampsia, fitting the eligibility criteria (Figure 1). Patients’ age, weight, and gestational age at delivery were similar between both groups (Table 1).
| Parameter | Oxytocin (n = 40) | Carbetocin (n = 40) | P-Value |
|---|---|---|---|
| Age (y) | 27.43 ± 6.73 | 27.75 ± 6.83 | 0.831 |
| Weight (kg) | 73.92 ± 12.67 | 73.8 ± 12.22 | 0.964 |
| GA (week) | 38.27 ± 1.11 | 38.35 ± 1.05 | 0.757 |
| Postoperative Hb (g/dL) | 9.92 ± 0.71 | 9.89 ± 0.74 | 0.863 |
| Blood loss (mL) | 851.25 ± 93.02 | 849 ± 87.64 | 0.912 |
Abbreviations: GA, gestational age; Hb, hemoglobin.
a Values are expressed as mean ± standard deviation.
4.2. Outcomes
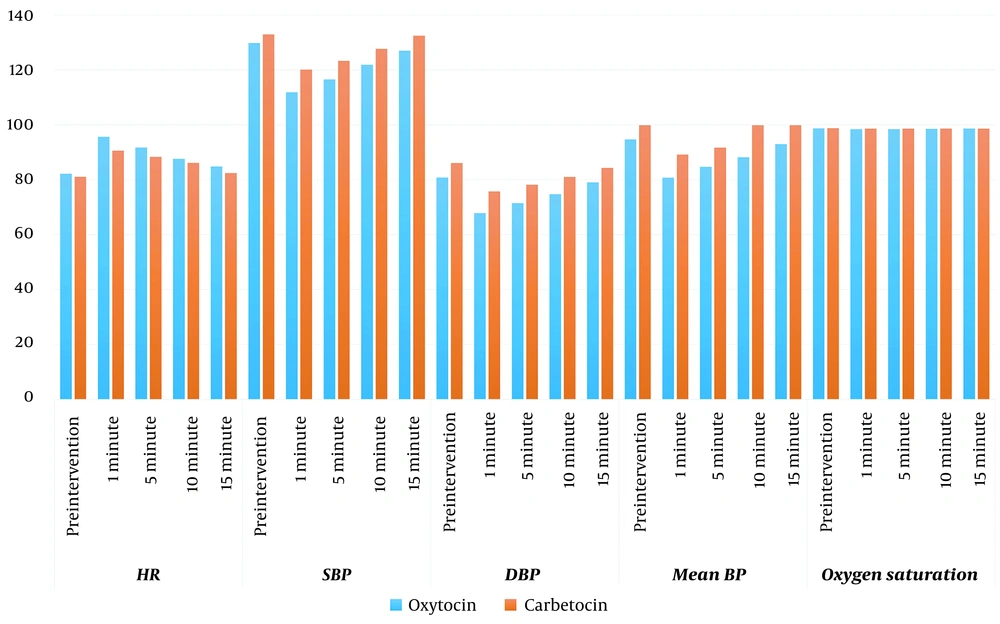
Firstly, based on the independent group comparison, there was a significantly higher SBP (at 1 and 5 minutes) and DBP and mean BP (both at 1, 5, 10, and 15 minutes) in the carbetocin group than in the oxytocin group (Table 2). Secondly, based on the intragroup comparison using paired t-test, there was a significant increase in HR and reduction in BP (including SBP, DBP, and mean BP) from the baseline to all intervals after the administration of both interventions except for the 15-minute interval after carbetocin administration; however, the SBP and mean BP returned to the same value before the intervention. Furthermore, there was a significant decline in O2 saturation in the oxytocin group after 1 and 5 minutes of drug administration; however, it returned to values similar to before the intervention (Figure 2 and Table 2).
| Parameter | Oxytocin (n = 40) | Carbetocin (n = 40) | P-Value b | P-Value c |
|---|---|---|---|---|
| HR | ||||
| Pre-intervention | 81.08 ± 10.27 | 81.08 ± 10.27 | 0.664 | - |
| 1 minute | 90.62 ± 10.56 | 90.62 ± 10.56 | 0.083 | < 0.001 d/< 0.001 d |
| 5 minutes | 88.33 ± 10.9 | 88.33 ± 10.9 | 0.205 | < 0.001 d/< 0.001 d |
| 10 minutes | 86.15 ± 9.91 | 86.15 ± 9.91 | 0.59 | < 0.001 d/< 0.001 d |
| 15 minutes | 82.4 ± 10.6 | 82.40 ± 10.6 | 0.359 | < 0.001 d/0.002 d |
| SBP | ||||
| Pre-intervention | 129.8 ± 15.91 | 132.93 ± 16.74 | 0.395 | - |
| 1 minute | 111.85 ± 11.28 | 120.12 ± 11.73 | 0.002 d | < 0.001 d/< 0.001 d |
| 5 minutes | 116.53 ± 12.29 | 123.33 ± 12.54 | 0.017 d | < 0.001 d/< 0.001 d |
| 10 minutes | 121.90 ± 13.35 | 127.70 ± 13.62 | 0.058 | < 0.001 d/< 0.001 d |
| 15 minutes | 127 ± 14.33 | 132.47 ± 14.82 | 0.097 | 0.002 d/0.569 |
| DBP | ||||
| Pre-intervention | 80.8 ± 12.5 | 86.08 ± 12.13 | 0.059 | - |
| 1 minute | 67.85 ± 10.21 | 75.72 ± 8.04 | < 0.001 d | < 0.001 d/< 0.001 d |
| 5 minutes | 71.42 ± 9.7 | 78.17 ± 8.74 | 0.002 d | < 0.001 d/< 0.001 d |
| 10 minutes | 74.7 ± 9.88 | 81.03 ± 8.92 | 0.004 d | < 0.001 d/< 0.001 d |
| 15 minutes | 79.03 ± 10.51 | 84.33 ± 9.54 | 0.021 d | 0.046 d/0.041 d |
| Mean BP | ||||
| Pre-intervention | 94.67 ± 13.14 | 99.85 ± 13.3 | 0.084 | - |
| 1 minute | 80.75 ± 10.42 | 89.15 ± 8.9 | < 0.001 d | < 0.001 d/< 0.001 d |
| 5 minutes | 84.72 ± 10.92 | 91.72 ± 9.25 | 0.003 d | < 0.001 d/< 0.001 d |
| 10 minutes | 88.2 ± 10.28 | 94.97 ± 10.03 | 0.004 d | < 0.001 d/< 0.001 d |
| 15 minutes | 93 ± 11.25 | 98.97 ± 10.49 | 0.016 d | 0.043 d/0.261 |
| O2 saturation | ||||
| Pre-intervention | 98.7 ± 1.02 | 98.78 ± 0.92 | 0.73 | - |
| 1 minute | 98.42 ± 1.13 | 98.6 ± 0.93 | 0.451 | 0.02 d/0.09 |
| 5 minutes | 98.45 ± 1.11 | 98.6 ± 0.84 | 0.497 | 0.023 d/0.07 |
| 10 minutes | 98.53 ± 1.01 | 98.67 ± 0.92 | 0.489 | 0.07/0.16 |
| 15 minutes | 98.65 ± 1.05 | 98.6 ± 0.93 | 0.822 | 0.323/0.09 |
Abbreviations: HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; BP, blood pressure.
a Values are expressed as mean ± standard deviation.
b P-value for comparison of each mean value in the same raw (i.e., between oxytocin and carbetocin groups) using the independent student’s t-test or Mann-Whitney U test as appropriate
c P-value for comparison of each interval value to the pre-intervention value for oxytocin and carbetocin groups, respectively
d Significant
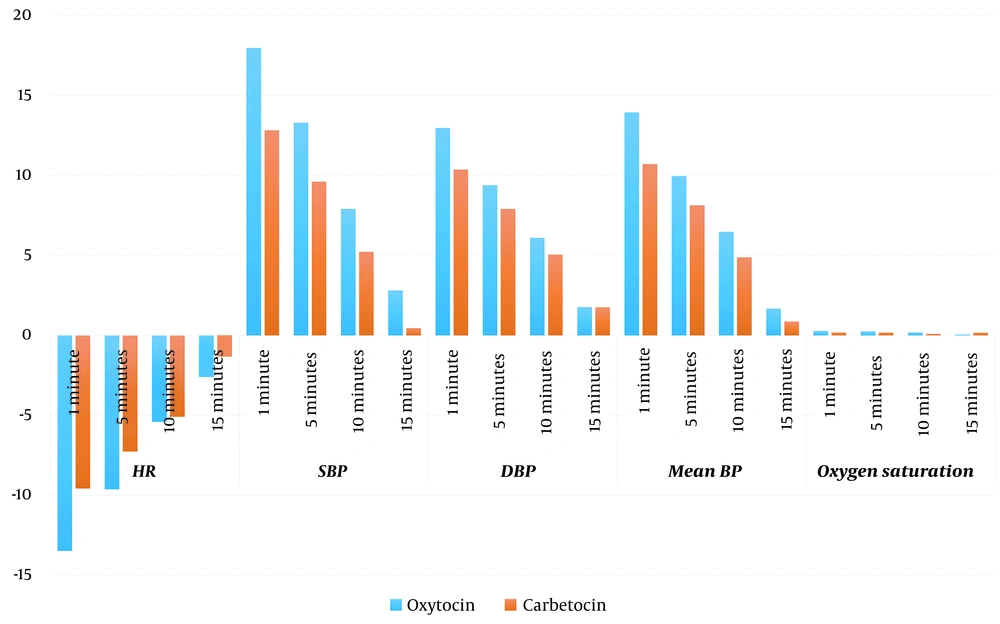
Moreover, based on the intergroup comparison, there was a significantly more increase in HR (at 1 minute); nevertheless, there was a significantly more decrease in SBP (at 1, 5, and 15 minutes) and mean BP (at 1 minute) in the oxytocin group than in the carbetocin group. Similarly, there was more increase in HR and more decrease in SBP, DBP, and mean BP in the oxytocin group in other time points; however, the difference was insignificant. On the contrary, there was no significant difference between both groups in O2 saturation (Figure 3 and Table 3).
Differences between mean values of study intervals and pre-intervention values. These values were calculated as follows: The mean of pre-intervention value – the mean of each interval (i.e., 1, 5, 10, and 15 minutes). Abbreviations: HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; BP, blood pressure.
| Parameter | Oxytocin (n = 40) | Carbetocin (n = 40) | P-Value c |
|---|---|---|---|
| HR | |||
| 1 minute | -13.45 ± 6.91 | -9.55 ± 4.66 | 0.004 d |
| 5 minutes | -9.6 ± 6.02 | -7.25 ± 5.58 | 0.074 |
| 10 minutes | -5.4 ± 4.83 | -5.08 ± 4.69 | 0.761 |
| 15 minutes | -2.6 ± 3.58 | -1.32 ± 2.59 | 0.072 |
| SBP | |||
| 1 minute | 17.95 ± 9.83 | 12.8 ± 6.74 | 0.008 d |
| 5 minutes | 13.28 ± 8.64 | 9.6 ± 7.27 | 0.043 d |
| 10 minutes | 7.9 ± 7.74 | 5.22 ± 6.31 | 0.094 |
| 15 minutes | 2.8 ± 5.25 | 0.45 ± 4.96 | 0.043 d |
| DBP | |||
| 1 minute | 12.95 ± 6.16 | 10.35 ± 6.78 | 0.076 |
| 5 minutes | 9.38 ± 6.34 | 7.9 ± 7.17 | 0.333 |
| 10 minutes | 6.1 ± 5.74 | 5.05 ± 5.81 | 0.419 |
| 15 minutes | 1.77 ± 5.46 | 1.75 ± 5.24 | 0.983 |
| Mean BP | |||
| 1 minute | 13.93 ± 7.26 | 10.7 ± 6.83 | 0.044 d |
| 5 minutes | 9.95 ± 6.86 | 8.12 ± 7.1 | 0.246 |
| 10 minutes | 6.47 ± 6.01 | 4.88 ± 5.45 | 0.216 |
| 15 minutes | 1.68 ± 5.07 | 0.88 ± 4.85 | 0.473 |
| O2 saturation | |||
| 1 minute | 0.28 ± 0.72 | 0.17 ± 0.64 | 0.511 |
| 5 minutes | 0.25 ± 0.67 | 0.17 ± 0.59 | 0.598 |
| 10 minutes | 0.17 ± 0.59 | 0.1 ± 0.44 | 0.524 |
| 15 minutes | 0.05 ± 0.32 | 0.17 ± 0.64 | 0.269 |
Abbreviations: HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; BP, blood pressure.
a Values are expressed as mean ± standard deviation.
b These values were calculated as follows: The mean of pre-intervention value - the mean of each interval (i.e., 1, 5, 10, and 15 minutes)
c P-value for comparison of differences between oxytocin and carbetocin groups using one-way analysis of variance
d Significant
No ephedrine was given after the administration of the study drugs; however, some cases had ephedrine after spinal anesthesia. Moreover, there were no significant differences in postoperative hemoglobin (9.92 and 9.89 g/dL, respectively) or blood loss (851.25 and 849 mL, respectively) between the oxytocin and carbetocin groups (Table 1).
4.3. Side Effects and Complications
Of note, no signs of myocardial ischemia were documented, and no patients needed a blood transfusion in the two groups. However, there were three and seven cases that required another dose of carbetocin and oxytocin, respectively. Moreover, one case developed PPH in the carbetocin group; nevertheless, two cases developed PPH in the oxytocin group.
5. Discussion
In this double-blind RCT, several interesting findings were obtained after documenting the hemodynamic changes after the administration of oxytocin or carbetocin in preeclamptic women undergoing an elective C-section under spinal anesthesia. This study revealed a good and safe hemodynamic profile in the carbetocin group; nevertheless, there was a significant increase in HR and a reduction in BP (including SBP, DBP, and mean BP) after the administration of both interventions. However, the carbetocin group returned to normal SBP and mean BP after 15 minutes, but the oxytocin group did not. Moreover, the increase in HR and the reduction in BP were more in the oxytocin group.
It is known that the hemodynamic effects of an oxytocin bolus include increased cardiac output and pressure of the pulmonary artery, hypotension, systemic vasodilation, and tachycardia, depending on the dose and rate of administration (17, 21, 22). Such hemodynamic impact, especially on patients with cardiovascular diseases or hypovolaemia, could result in myocardial ischemia (23), which is increasing due to the increase in the number of deliveries with potential risk factors. Some studies suggest that general anesthesia, preeclampsia, and eclampsia are contraindications to carbetocin; nevertheless, the findings of the current study propose a new threshold in the attempt to enlarge the therapy indications. Previous studies showed similar results (17, 18, 24-28). A recent study demonstrated that females treated with oxytocin have a more noticed hypotension and hemodynamic rebound than carbetocin-treated females (26).
In addition, this study indicated that more patients needed additional doses of oxytocin and developed PPH in the oxytocin group. Dansereau et al. reported similar findings with lower additional doses of uterotonics for the treatment of uterine atony in females taking carbetocin after delivery (19). Several studies described similar results (29-32).
The present study’s findings of the safe hemodynamic effects with less need for more uterotonics and the previous findings that repeated oxytocin administration led to significant hemodynamic changes (33) reinforcing the notion that carbetocin might become the treatment of choice as a more effective uterotonic drug than oxytocin for preventing PPH in females with preeclampsia, hypertension, or cardiac problems (26, 31).
Undoubtedly, oxytocin could be given as a slow infusion with the least possible dose (26) because rapid intravenous bolus has the potential to cause a risky hemodynamic collapse in females unable to mount compensatory increases in cardiac output, such as those with hypovolemia or cardiac diseases. Nevertheless, the manufacturer of carbetocin recommends a bolus carbetocin injection (34).
The present study revealed a significant decline in O2 saturation in the oxytocin decline but not in the carbetocin group, although both were still within normal levels. Finally, this study did not demonstrate any difference in the amount of blood loss or the drop in the hemoglobin level. Larciprete et al. shared similar findings (29).
Oxytocin briefly tends to cause hypotension accompanied by marked increases in cardiac output and HR in healthy females undergoing a C-section under spinal anaesthesia (17). It is assumed that the primary hemodynamic effect of oxytocin is vasodilation action via receptors on vascular endothelium that triggers the nitric oxide pathway (35). Therefore, it was proposed that the changes in HR and cardiac output represent compensatory mechanisms, without which hypotension would be more pronounced. Blood autotransfusion into the systemic circulation following oxytocin-produced uterine contractions could be considered a potential cause of the increase in cardiac output. However, a large increase in the preload to the heart would be expected to result in a compensatory slowing of HR, not the tachycardia that was noticed (17).
Of note, the small difference in the molecular structure of carbetocin and oxytocin could determine not only the uterotonic stronger and longer effect but also the difference in the biological function as the absence of antidiuretic or vasopressin-like effects, and this is an important result in the attempt to define a more comprehensive carbetocin profile (29). It is also noteworthy that the intramuscular injection of carbetocin induced tetanic contraction in < 2 minutes and for nearly 11 minutes, followed by rhythmic contraction for 2 more hours; nevertheless, the intravenous injections of carbetocin induced tetanic contraction of the uterus in 2 minutes and for nearly 6 minutes, followed by rhythmic contractions for 60 minutes. Additionally, the prolonged action of intramuscular injection was statistically significant, compared to intravenous administration (36). Therefore, it is the current study’s limitation. It is suggested to perform studies using the intramuscular route instead. Moreover, this study only compared the two drugs at a fixed dose without a titration curve of the two drugs.
5.1. Conclusions
The findings of the present study suggest using carbetocin instead of oxytocin as a uterotonic drug with high therapeutic potential and minimum hemodynamic impact on patients with preeclampsia undergoing a C-section. The minimal effect of carbetocin on patients’ hemodynamics could extend the use of this drug in patients who have preeclampsia, risk factors of hemorrhage, and/or hypertension.