1. Background
Chronic neck pain is a collective symptom confronted in pain centers, the source of which is usually the cervical facet joint (1, 2). A recent study showed that cervical facet joint pain prevalence was 49.3% (3). The pain characteristic of the cervical facet joint is designated as a facet referral pattern depending on the level of the cervical facet joint (4, 5). Continuous radiofrequency ablation (RFA) of the cervical medial branches has effectively handled cervical facet joint pain (6). Unfortunately, more than 40% of the patients undergoing RFA report adverse effects such as postprocedural pain, cutaneous numbness, dysesthesia, dizziness, and ataxia (7-9). As a result, pulse radiofrequency (PRF) was introduced to treat cervical facet joint pain to avoid any thermal reaction of RFA. However, the duration of pain relief is shorter following PRF than in RFA (10, 11).
2. Objectives
This study aimed to determine the effectiveness and postprocedural adverse effects between combined RFA and PRF vs RFA separately in cervical facet joint pain.
3. Methods
3.1. Patients
After receiving approval from the Institutional Review Board of the Medical Ethics Committee and enrolling in the Thai Clinical Trails Registry (TCTR20221015001), the medical records of those undergoing a cervical radiofrequency ablation procedure between June 2014 and June 2020 were reviewed. The RFA technique was performed until June 2017 but has been modified to combined RFA and PRF since June 2017. Inclusion criteria included patients presenting positive diagnostic cervical medial branches block defined as pain relief of more than 50% from baseline (12). Exclusion criteria were repeated cervical radiofrequency ablation, neck pain with radicular symptoms, severe cervical disc lesion, malignancy, psychological problem, language barrier, history of allergy to radio-opaque contrast solution, lidocaine or bupivacaine, and inadequate medical records.
3.2. Intervention
3.2.1. Diagnostic Procedure
The diagnostic protocol has been described in detail elsewhere (13), and a symptomatic facet joint was designated according to the pain referral pattern pronounced by Dwyer et al. (5). Also, medial branches were injected with 2% lidocaine at 0.3 mL per site.
3.2.2. Treatment Procedure
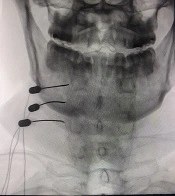
The posterior technique was first published in 1995 (7). All interventions assessed the intravenous saline lock on arrival at the outpatient department using pulse oximetry, noninvasive blood pressure, and electrocardiography monitoring. The resuscitating equipment and medications were prepared if intravenous sedation was required. Patients were assigned in a prone position under C-ARM fluoroscopic guidance (9900 Elite, Super C, OEC, UT, USA). The electrode pad of the radiofrequency equipment was attached to the ipsilateral side of the posterior thigh. After the skin was anesthetized with 1% lidocaine, a 20-gauge, 10-cm cannula with a 10-mm curved active tip (Diros RF Cannula, Diros Technology Inc., Canada) was inserted along a 15 to 30-degree angle to the sagittal plane (slightly posterior oblique approach) (14, 15). The cannula was applied until reaching the lateral part of the articular pillar (Figure 1). Then, the depth of the cannula was checked using a lateral view (Figure 2). A probe was inserted through the cannula and linked to a radiofrequency generator (Diros Technology OWL, Canada). After impedance was accomplished at below 500 Ohm, sensory stimulation was performed at 50 Hz, and the patient reported not feeling any tingling sensation along the dermatome distribution.
Consequently, a motor stimulation (2 Hz) was executed until multifidus twitching was presented at stimulation less than 1 volt, and no motor twitching was observed along the myotome. A nonionic contrast medium was injected to ensure the intravascular injection before 0.5 mL lidocaine 1% was injected after the needle reached the desired location. The study investigated two lesions due to the anatomical variation of the medial branches (9). Patients in the CRF group underwent RFA at 80°C for 90 seconds for two cycles. Patients in the CPRF group underwent RFA at 80°C for 90 seconds for one cycle, followed by PRF at 42°C for 120 seconds for one cycle. Also, 0.125% bupivacaine plus 2 mg of dexamethasone in a total volume of 1 mL was injected after lesioning had been performed.
3.3. Measurement
The demographic data, including age, sex, comorbidities, and body mass index (BMI), level of procedure, Visual Analog Scale (VAS;1-100), neck pain disability index -Thai Version (NDI-TH), and complications were reviewed. The NDI-TH has been translated to Thai and validated, exhibiting high inner consistency (intraclass correlation coefficient score 0.986) (16). It contains 10 sections: seven related to everyday behaviors, two related to pain, and one related to concentration. All items are scored from 0 to 5. A score of 0 denotes the maximum level of function, while a score of 5 indicates the bottom level of function. The maximum score is 50, and a greater score relates to an increased level of disability. The NDI-TH scores were recorded before intervention and at the first week, first month, third month, sixth month, ninth month, and the first year after the intervention. The follow-up was performed either face-to-face or by phone, and patients were not permitted to use over-the-counter analgesic medication. The primary outcome was the number of patients who experienced successful treatment, expressed as at least 80% pain relief from baseline (17) and the NDI score of less than 15 (18) for at least three months (15). The secondary outcomes comprised the duration of pain relief defined as the time of pain relief until VAS had been restored to at least 50% from baseline (19) and side effects including numbness, ataxia, dysesthesia, hypersensitivity, itching, and muscular weakness (dropped head syndrome) in the groups. A research assistant, uninvolved in the intervention or postoperative follow-up, retrospectively collected all data from medical records.
3.4. Statistical Analysis
The sample size was calculated based on the study of Lord et al. (8). The probability of unsuccessful treatment with RFA was 0.417, while the probability of unsuccessful treatment from control was 0.916. Therefore, 13 patients per group were required to reach a significance level of 0.05, and the power of the study was established at 80%. Statistical analysis was performed using SPSS, Version 26.0 (IBM Corp., released 2011, Armonk, NY, USA). Descriptive values for continuous data were presented as mean and Standard Deviation (SD) for adequately normal distribution. For nominal data, absolute and relative frequencies were exhibited for each category. The chi-square test and independent t-test were employed to compare the differences between groups in categorical and continuous data, respectively. The duration of pain relief was shown as a median and 95% confidence interval and compared using the Mann-Whitney test. Kaplan-Meier survival curves were executed for both treatment groups, and significant differences between groups were determined using the log-rank test. A P-value < 0.05 was considered statistically significant.
4. Results
The medical records of 83 patients with chronic neck pain were reviewed. Of them, 26 patients were excluded because the pain had been managed with oral pain medication; 12 patients were excluded due to negative diagnostic cervical medial branch block; two patients were excluded due to neck pain with radicular pain symptoms, and three patients in the CRF group and one patient in the CPRF group had incomplete documentation of data due to lost follow-up. The final analysis included 21 patients in the CRF group and 18 in the CPRF group, as presented in Figure 3.
No differences were shown regarding baseline characteristics in terms of age, sex,
BMI, VNRS, NDI, and level of facet referral pattern, as presented in Table 1.
| Features | CRF (N = 21) | CPRF (N = 18) | P-Value |
|---|---|---|---|
| Gender (man) | 12 (57.1) | 10 (55.6) | 0.921 |
| Age, y | 52.95 ± 10.48 | 52.28 ± 11.78 | 0.851 |
| Body weight (kg) | 68.1 ± 9.94 | 70.11 ± 12.78 | 0.583 |
| Height (cm) | 167.76 ± 8.28 | 168.33 ± 6.71 | 0.816 |
| BMI (Kg/m2) | 24.09 ± 2.04 | 24.62 ± 3.42 | 0.553 |
| VAS | 78.1 ± 10.3 | 78.33 ± 9.24 | 0.940 |
| NDI | 24.76 ± 2.81 | 23.83 ± 2.79 | 0.309 |
| Level | 0.829 | ||
| C2-3 | 4 (19) | 4 (22.2) | |
| C2-4 | 3 (14.3) | 2 (11.1) | |
| C2-6 | 2 (9.5) | 3 (16.7) | |
| C2-7 | 1 (4.8) | 0 (0) | |
| C3-6 | 2 (9.5) | 0 (0) | |
| C3-7 | 2 (9.5) | 1 (5.6) | |
| C4-6 | 2 (9.5) | 1 (5.6) | |
| C4-7 | 3 (14.3) | 3 (16.7) | |
| C5-6 | 2 (9.5) | 3 (16.7) | |
| C5-7 | 0 (0) | 1 (5.6) |
Abbreviations: CRF, radiofrequency ablation (RFA) group; CPRF, combined RFA and pulsed radiofrequency (PRF) group; BMI, body mass index; VAS, Visual Analog Scale; NDI, neck pain disability index.
a Data are presented as numbers (%) of patients or mean ± SD.
The average VNRS and NDI scores were significantly reduced from baseline at all follow-ups in both groups (P < 0.001). However, no significant difference was shown among the groups (P > 0.05).
4.1. Primary Outcomes
Fourteen (66.7%) and 12 (66.7%) patients in the CRF and CPRF groups had successful treatment at three and six-month follow-ups, respectively. Only one (5.6%) patient in the CPRF group had successful treatment at the nine-month follow-up. However, no significant difference was found between the group comparisons throughout the whole follow-up period (P = 0.274), as shown in Table 2.
| Follow-up Periods | CRF (N = 21) | CPRF (N = 18) | P-Value |
|---|---|---|---|
| 1 week | 15 (71.4) | 15 (83.3) | 0.379 |
| 1 month | 14 (66.7) | 12 (66.7) | 1 |
| 3 months | 14 (66.7) | 12 (66.7) | 1 |
| 6 months | 14 (66.7) | 12 (66.7) | 1 |
| 9 months | 0 (0) | 1 (5.6) | 0.274 |
| 12 months | 0 (0) | 0 (0) | N/A |
Abbreviations: CRF, radiofrequency ablation (RFA) group; CPRF, combined RFA and pulsed radiofrequency (PRF) group.
a Data are presented as numbers (%) of patients.
4.2. Secondary Outcomes
The median time to the reoccurrence of at least 50% of the preprocedural pain was 303.8 days in the CRF group and 270 days in the CPRF group, as shown in Table 3. The Kaplan-Meier survival curves showed that 16 patients in the CRF group and 14 in the CPRF group had a successful outcome at six months of follow-up. However, an insignificant difference was demonstrated between the two groups using the log-rank test (P = 0.395), as shown in Figure 4.
| Groups | Time (d) | 95% CI |
|---|---|---|
| CRF | 303.8 | 268.7 - 338.8 |
| CPRF | 270.0 | 164.2 - 375.8 |
| Overall | 300.0 | 266.9 - 333.1 |
Abbreviations: CRF, radiofrequency ablation (RFA) group; CPRF, combined RFA and pulsed radiofrequency (PRF) group.
a Data are presented as median and 95% confidence interval (CI)
The study found more significant side effects in the CRF group, including numbness, dysesthesia, and hypersensitivity syndrome (P < 0.05). However, no significant difference was indicated between the groups concerning ataxia side effects (14 (66.7%) vs. nine (50%) in the CRF vs. CPRF groups, respectively, P = 0.291). One patient in CRF group reported mild weakness of the cervical extensor muscles from RFA at bilateral C3-7 medial branches, while no patients in the CPRF group experienced extensor muscle weakness (P = 0.348). Itching was not reported in either groups, and no cases of serious or permanent complications were recorded, as presented in Table 4.
Abbreviations: RF, radiofrequency; CRF, radiofrequency ablation (RFA) group; CPRF, combined RFA, and pulsed radiofrequency (PRF) group.
a Data are presented as numbers (%) of patients.
b P < 0.05
5. Discussion
This is the first report to compare outcomes for combined RFA and PRF (CPRF group) vs RFA alone (CRF group) to alleviate cervical facet joint pain. The study found a 66.7% success rate for initial radiofrequency treatment in both groups at three and six months, which is similar to a previous study (17). Additionally, the median time of pain relief was 303.8 days and 270 days in the CRF and CPRF groups, respectively, which is similar to prior studies reporting median durations of benefit from radiofrequency treatment ranging from 161 to 421 days (8, 9, 20, 21). Similar outcomes in successful treatment and duration of pain relief in both groups may have stemmed from extended effects of thermocoagulation in RFA, producing cell apoptosis surrounding the tip of the electrode at 80°C (22-24) and prolonging the upregulation of inflammatory cytokines in the CRF group. However, the analgesic effects gradually wore off in the PRF, resulting in the CPRF group showing slightly less duration of pain relief (25).
Post-radiofrequency (RF) side effects, including ataxia, cutaneous numbness, and dysesthesia, have been reported at 19% to 97% (9, 26, 27); the wide range in incidence rates might have stemmed from differences in either the cervical levels treated or RF techniques. Our study showed a lower incidence of RF side effects compared with a study performed at the C2-3 segment, which RF ablation of the upper cervical level being associated with a higher incidence of neuritis (9). However, our study found a higher incidence of RF side effects than Lord et al. (26), which might be due to different approaches or difference surveillance methods; we applied a single 20-gauge RF cannula per medial branch per level in a slightly posterior oblique position while study by Lord et al. placed 22-gauge electrodes via 2 different trajectories , creating 2 to 3 lesions at each location (8, 26). However, recent consensus practical guidelines recommend using a posterior or slight posterior oblique approach in all cervical medial branch RF (15).
Interestingly, the CPRF group exhibited significantly lower post-radiofrequency side effects, including numbness, dysesthesia, and hypersensitivity syndrome, than CRF group. These results stemmed from PRF determined by exposing nerves to high electrical fields without neurodestructive effects and reducing the risk of RFA caused by heat dispersed in the surrounding tissue. This occurred during an inactive period of 480 msec after exposure to the radiofrequency electrical field, delivering an active phase of 20 msec at a repetition rate of 2 Hz (28). Moreover, PRF initiated the C-fos gene (immediate early gene), which may have reduced pain transmission to the superficial lamina of the spinal dorsal horn (29, 30), decreasing glial cell activation (31), decreasing the release of excitatory pain neurotransmitters at the presynaptic area (32), and inducing descending inhibitory pain pathways (33). Therefore, fewer incidences of post-radiofrequency complications due to the neuromodulation effect (34) were similar to those in a prior study reporting a lower incidence of post-procedural complications after combining RFA with PRF in trigeminal neuralgia (35).
One patient in the CRF group reported mild weakness of the cervical extensor muscle from bilateral C3 to 7 medial branch lesioning, which might have stemmed from the neurodestruction of medial branches on multiple cervical levels (19, 36). However, these complications were unreported in the CPRF group, where the neuromodulation effect from PRF might have reduced neurodestructive effects.
5.1. Limitations
The present study confronted some limitations. First, this constitutes a retrospective study in which intraoperative and immediate postoperative complications such as vagovagal and dizziness were unrecorded. However, transient effects were observed (7-9). Moreover, serious complications were found, including the intrathecal, intravascular injection, or direct nerve injury. Second, the duration of post-radiofrequency complications such as numbness or dysesthesia was also unrecorded. However, a similar study reported that the numbness typically continued for one to three weeks and was often substituted by itching and dysesthesia, followed by the return of usual cutaneous sensation (7, 9). Third, the study did not demonstrate a double block during the diagnostic period. However, recent guidelines endorse a single block before cervical radiofrequency ablation is sufficient, and double blocks will cause a significant quantity of false negative responses (15). Fourth, patients with previous spine surgery were enrolled in the study, which might have affected the outcome. However, a recent study showed no difference in success rates between previous surgical and nonsurgical patients (15, 37). Fifth, oral medication and physiotherapy before and after intervention were not demonstrated, which might have affected the result. However, strong opioids or outside medication was not permitted, and only two physicians (WM and SM) prescribed oral pain medications. Finally, it is a retrospective study from a single center. Therefore, a prospective study using a larger sample size should be performed.
5.2. Conclusions
Combined RFA and PRF can be used for cervical facet joint pain, providing a success rate and duration of pain relief as RFA alone but with significantly fewer postoperative complications.