1. Introduction
Laryngospasm is a potentially life-threatening condition characterized by an involuntary laryngeal muscle spasm obstructing the glottis that manifests as severe dyspnea and stridor. This obstruction can last seconds to minutes and may cause hypoxemia, loss of consciousness, bradycardia, and death (1). Laryngospasm may have different etiologies. It can be an adverse event during anesthesia. Gastroesophageal reflux disease (GERD), emotional stress, tobacco smoke exposure, and upper respiratory tract infections (URI) can also cause laryngospasm (2). So far, there have been no reported cases of laryngospasm due to Coronavirus disease 19 (COVID-19). We report a case of laryngospasm as a complication of COVID-19 in a middle-aged lady.
2. Case Presentation
A 56-year-old lady presented to the emergency department (ED) with severe respiratory distress, which suddenly started minutes before ED admission. The patient was a pediatric otolaryngologist. Her symptoms started three days before her presentation to ED, with a low-grade fever and myalgia, followed by a sore throat and anosmia the next day. On the third day, hoarseness and coughing were added to her symptoms. She experienced sudden and severe dyspnea, and stridor started minutes before her ED visit. At ED presenting time, her respiratory rate and SpO2 were 35/min and 76%, with a pulse rate and blood pressure of 128 beats per minute (bpm) and 125/85 mmHg, respectively. She was agitated with evident air hunger, asking for a tracheostomy to maintain her airway patency. Supplementary oxygen started immediately, and 0.5 mg of intramuscular epinephrine was administrated with 200 mg of intravenous hydrocortisone. Five minutes after epinephrine and oxygen administration, an improvement was observed in her SpO2 and respiratory distress, but the stridor did not respond to therapy. Due to her clinical improvement, she did not undergo oro-tracheal intubation, but close monitoring and double airway setup were stood by the patient all ED time.
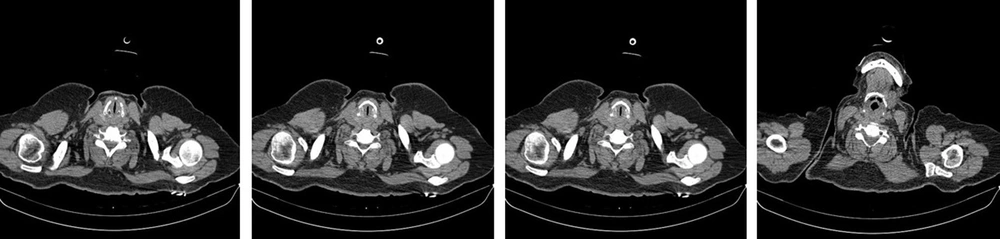
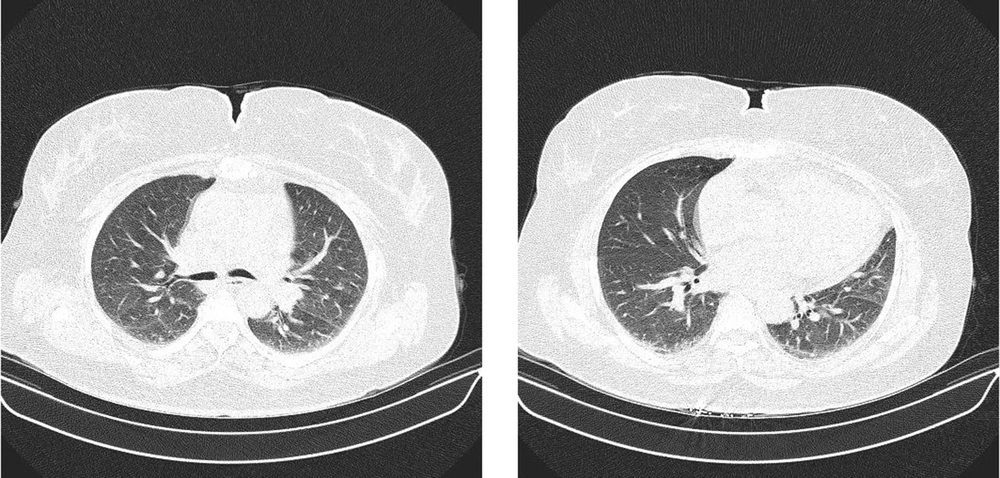
Urgent computed tomography (CT) results revealed stenosis in the glottis with a normal lung field. No radiologic manifestation of COVID-19 infection was reported in pulmonary CT (Figures 1 and 2). Her medical history was positive for tonsillectomy, lumbar discopathy, and discectomy, both of which were performed years ago. She had a history of COVID-19 infection 14 months before and completed the COVID-19 vaccination history. Her medical history was otherwise unremarkable. She was not a smoker and did not consume alcohol or recreational drugs. On the first day of her symptoms, she took acetaminophen and azithromycin orally and had no severe symptoms until her ED presentation. The patient was then admitted to the intensive care unit (ICU) and received continuous oxygen therapy. Corticosteroids started for her as a maintenance dose of 250 mg methylprednisolone twice a day, which she tapered in the following days. A positive result was obtained for the nasopharyngeal and oropharyngeal swabs of SARS CoV2 RTPCR. Table 1 shows laboratory test results on hospital stay days. The patient had an uneventful hospital stay in three days and was discharged home with a corticosteroid prescription. She had no complications or new complaints in the follow-up and fully recovered.
| Variables | ED Admission | ICU 1st Day | ICU 3rd Day |
|---|---|---|---|
| WBC | 7200 | 6000 | 6300 |
| Lymph | 880 | 830 | 870 |
| Hb | 13.4 | 12.7 | 12.8 |
| Plt | 246000 | 191000 | 197000 |
| PT | 13.5 | 13.5 | 13.5 |
| INR | 1.1 | 1.1 | 1.1 |
| PTT | 27 | 29 | 28 |
| LDH | 516 | 522 | 505 |
| CRP | 53 | 62 | 60 |
| Blood sugar | 106 | 98 | 110 |
| Urea | 20 | 22 | 21 |
| Creatinine | 0.8 | 0.8 | 0.7 |
| Na | 143 | 142 | 139 |
| K | 4.2 | 4 | 4.1 |
| Ca | 10.3 | ||
| Cholesterol | 230 | ||
| TG | 30 | ||
| LDL | 146 | ||
| HDL | 37 | ||
| IL-6 | 2 | ||
| TSH | 1 | ||
| T4 | 11 | ||
| T3 | 0.7 | ||
| RTPCR | positive |
3. Discussion
Closure of the glottic opening by vocal cord constriction is a protective reflex to avoid aspiration. Laryngospasm is an exaggerated form of this reflex that can cause life-threatening complications. Laryngospasm mainly occurs as an anesthetic adverse event in light planes of anesthesia. It is the most common cause of upper respiratory tract obstruction during the extubation of patients. Although laryngospasm is not an uncommon anesthesiologic event, it is rare outside the operation room and may have various etiologies. In the literature, paroxysmal laryngospasm is described as a rare cause of laryngospasm. Bai et al. studied paroxysmal laryngospasm in 12 patients and found a history of GERD in seven patients. In patients with GERD, laryngeal irritation due to pepsin and acid can end in exaggerated laryngeal reflexes manifested as laryngospasm (3). Our patient did not have a history of GERD.
The second most frequent trigger was cough in the study of Bai et al. Although our patient had had non-productive coughs since the third day of her symptoms, she denied that her laryngospasm started with coughing as a trigger. Moreover, she did not have emotional stress that could trigger paroxysmal laryngospasm. Hypocalcemia can cause laryngospasm, and a case of hypocalcemic laryngospasm was described by Van Veelen et al. (4). However, our patient had no electrolyte disturbance, including hypocalcemia. URIs can trigger laryngospasm. Influenza has been described as a trigger by Minagi et al. (5). We did not find any report about laryngospasm triggered by COVID-19, and we believe that our patient is the first case of laryngospasm induced by COVID-19 infection. Corona spread in December 2019 and has affected the world since then. Therefore, in addition to the common manifestations of this disease, identifying its rare manifestations can also help to understand this pandemic as much as possible (6-9).