1. Background
Foot pain imposes a significant burden on individuals (1). Treatment strategies for regional foot pain focus on pain relief and better walking with normal plantar pressure (2). Minimally invasive therapies can meet the requirements to alleviate pain and improve walking in individuals with persistent foot and ankle pain (3, 4). Nonetheless, there is a dearth of research on the outcomes of nerve blocks in pain relief and walking improvement in patients with foot pain (4, 5).
There is a call for diagnostic procedures which can upgrade the consequences of pain therapy. Thermography uses infrared radiation to map the temperatures of the skin, and this method demonstrates potential as a diagnostic tool (6). However, the thermography of the plantar foot for better therapy of painful feet has not been analyzed. The authors of the present study were interested in whether the thermography of the plantar foot could give indications for better use of nerve blocks in individuals with foot pain.
2. Objectives
The present study aimed to define the protracted consequence of tibial nerve blocks with steroids for individuals with persistent foot pain, detect patient features coupled with long-term benefits, and investigate the link between the thermography of the plantar foot and the beneficial effect of tibial nerve block with steroids.
3. Methods
3.1. Ethical Statement
Ethical approval by the Medical Research Ethics Committees United, Nieuwegein, Utrecht, Netherlands, was granted for this study (W21.077). The current study retrospectively evaluated all patients who underwent a block of the tibial nerve in the Department of Pain Therapy of Pain Clinic De Bilt, Utrecht, Netherlands, within November 2019 to April 2020.
3.2. Subjects
All patients with chronic (> 6 weeks) intractable foot pain who had a treatment of the tibial nerve with corticosteroid injection within November 2019 and April 2020 were included. Previous conservative treatments included the restriction of excessive exercise or walking, arch support, shoe modifications, and oral analgesics. The inclusion criteria were foot pain and age over 18 years. The exclusion criteria were local infection or skin disorders at the injection site, allergy to bupivacaine or triamcinolone, and uncontrolled diabetes mellitus. The procedure for patients with painful feet comprised a clinical report, physical examination of the feet, and thermographic images before and half an hour after the tibial nerve block.
3.3. Variables and Desired Outcomes
The desired outcomes were the relief of foot pain and improvement in walking distance. Clinical variables and variables acquired from the thermography of the plantar foot were used to detect patient features coupled with long-term benefits.
3.4. Tibial Nerve Block
A tibial nerve block was put into effect by a skilled anaesthesiologist (H. Koning) in an accustomed way with a 21-gauge, 40-mm needle. The skin was cleaned with an antiseptic solution. The injection site was the median between the medial malleolus and the Achilles tendon and at the plane of the upper border of the medial malleolus. The needle was set toward the tibia, posterior to the artery, and deep to the retinaculum. A loss of resistance could be felt as the needle proceeded through the flexor retinaculum. A blend of 4 mL bupivacaine 0.5% (Bupivacaine Aurobindo, Baarn, the Netherlands) and 40 mg triamcinolone acetonide (Kenacort Bristol-Myers Squibb, Roma, Italy) was injected. A missed block was assigned in case the patient felt pain in the domain of the tibial nerve 30 minutes after the block. In the missed tibial nerve block patients, the procedure was repeated. The outpatients were supervised for 30 minutes.
3.5. Thermography
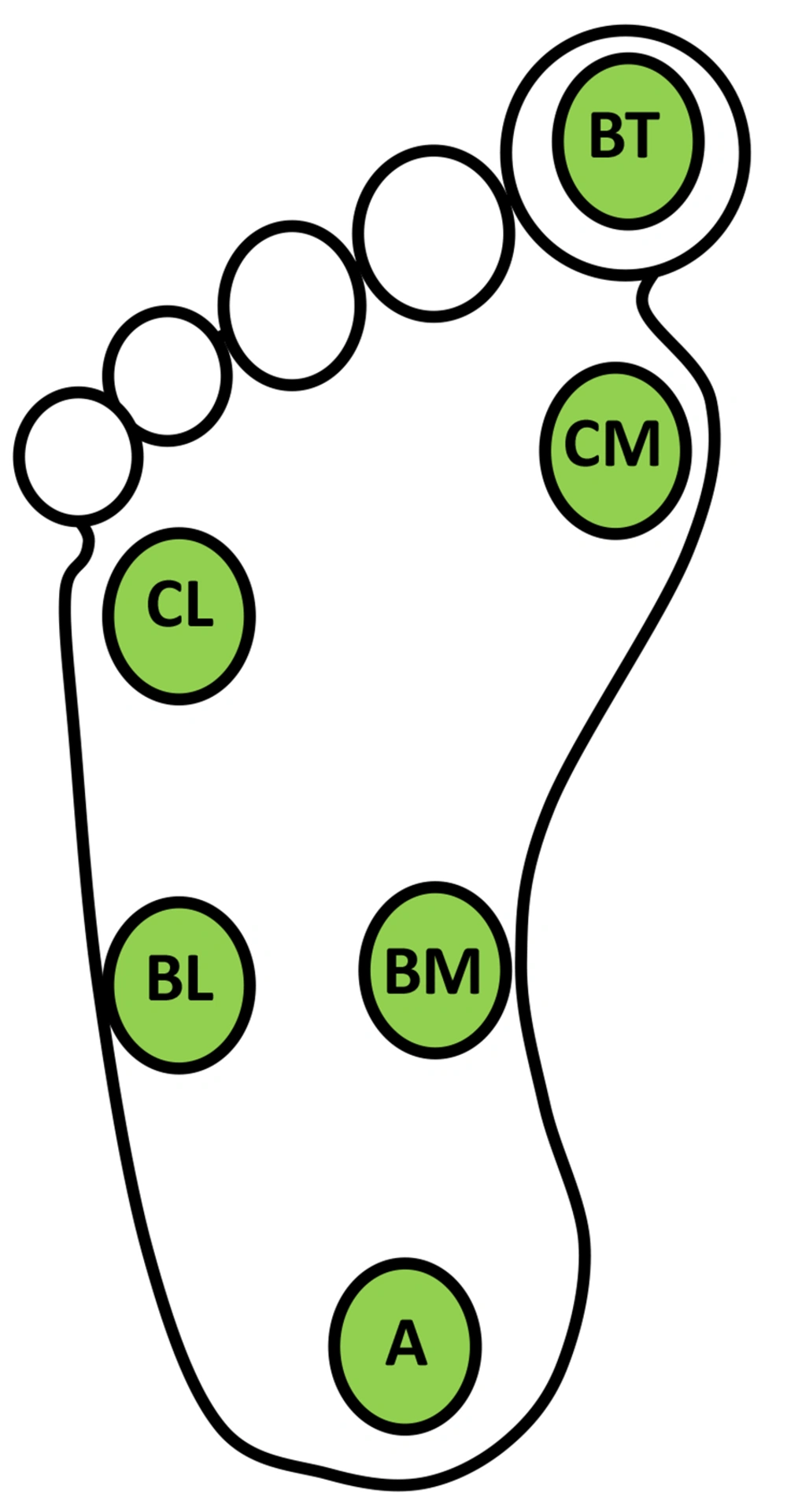
The thermography of the plantar foot was performed right before and 20 minutes after the block. The participants should not use topical products on their legs on the day of thermography. After removing any tight clothing, each participant was acclimatized to a temperature of 21°C for more than 15 minutes. With a FLIR (Oregon, USA) C3 thermal camera, the thermal images of the plantar foot were taken from 1.5 m and perpendicular to the participant’s feet. Then, these images were analyzed with Thermofy software 2021 (https://www.mirian.azurewebsites.net). The plantar foot was allocated into seven regions of interest (ROIs) and included the heel (A), the midfoot (BM-BL), the forefoot (CM-CL), and the big toe (BT) (Figure 1). In each ROI, the temperature was quantified using Thermofy software 2021. To calculate the mean temperature of the foot, the temperatures of the six ROIs were added up and divided by 6. The temperature of the ROI was noted as the gap between the mean temperature and the temperature of the ROI. For data analysis, each foot was scored separately.
3.6. Data Assessment
Patient information was retrieved from the electronic patient record. The included data were patient features (i.e., age and gender), information about the feet (i.e., left and/or right foot, traumatic injury, walking distance, and pain), comorbidity, self-announced benefit by therapy at 7 weeks on a four-point Likert scale (0%, less than 25%, 25 - 50%, and 50% or more), improvement of walking distance, period of benefit, and, if applicable, setback. Additional treatments for foot pain were carried on at 7 weeks after treatment if necessary. With a beneficial tibial nerve block, the term helpfulness from the initial procedure was noted.
The patients were evaluated, either during a repeat consultation or by questionnaire, if there was no consultation within 18 months. The subjects were contacted by an independent observer in September 2021 using an established questionnaire, including the current pain condition, consequences of therapy, relapse of the primary pain, and need for additional therapy.
3.7. Statistics
Analysis was carried out with Minitab software (version 18; Minitab Inc., State College, PA, USA), and an alpha level of P < 0.05 was brought into play for statistical signification. The student’s t-test was used for continuous variables, and the chi-square test for dichotomous variables. The term of benefit induced by tibial nerve block was examined with survival survey procedures (Kaplan-Meier plot). Stepwise regression was brought into action to distinguish variables for the regression model for a prosperous tibial nerve block. A discriminant analysis for partition in two sets assessed the interrelationship of significant variables with the beneficial effect of tibial nerve block.
4. Results
Within November 2019 to April 2020, 45 patients underwent a tibial nerve block for chronic foot pain. The age of the subjects ranged from 28 to 73 years, and 31% of the subjects were male. The symptoms existed for 2 - 51 years, with maximum visual analogue scale scores ranging from 18 to 100 mm. Moreover, 63% of the subjects had limited walking distance, and 13% of the subjects were diabetic and diagnosed with polyneuropathy. Tarsal tunnel syndrome was not diagnosed beforehand. Furthermore, 9 and 36 cases had one-sided and double-sided complaints of their feet, respectively. Table 1 shows the hallmarks of individuals with foot pain.
| Prevalence (%) | Q1 | Median | Q3 | |
|---|---|---|---|---|
| Age (y) | 51 | 63 | 73 | |
| Gender (male) | 31 | |||
| Diabetic (yes/no) | 13 | |||
| Limited walking distance (m) | 63 | |||
| Thermographic measurements before the procedure (°C) | ||||
| Mean temperature | 23.3 | 24.9 | 26.3 | |
| Difference temperature at ROI A and mean temperature | -1.0 | -0.4 | 0.2 | |
| Difference temperature at ROI BM and mean temperature | 1.6 | 2.1 | 2.6 | |
| Difference temperature at ROI BL and mean temperature | -0.5 | 0.4 | 0.9 | |
| Difference temperature at ROI CM and mean temperature | -0.7 | -0.2 | 0.3 | |
| Difference temperature at ROI CL and mean temperature | -1.3 | -0.9 | - 0.6 | |
| Difference temperature at ROI GT and mean temperature | -1.8 | -1.3 | - 0.4 |
Abbreviation: ROI, region of interest.
a A, BM, BL, CM, CL, GT: Specific measure points at the plantar feet (see methods).
In this study, 53% of the subjects had pain relief 7 weeks after the block. Additionally, 49% of the subjects had a reduction in their pain (46% good, 11% moderate, and 43% slight) following the treatment. Improved walking distance was revealed by 22% of the patients, and the progress was rated 3 times the actual walking distance (median: 3; Q1: 1.6; Q3: 4.8). Side effects of the tibial nerve block announced at 7 weeks after the treatment were the increase of pain and the occurrence of cramps of the legs in 5% (n = 2) and 5% (n = 2) of the outpatients, respectively.
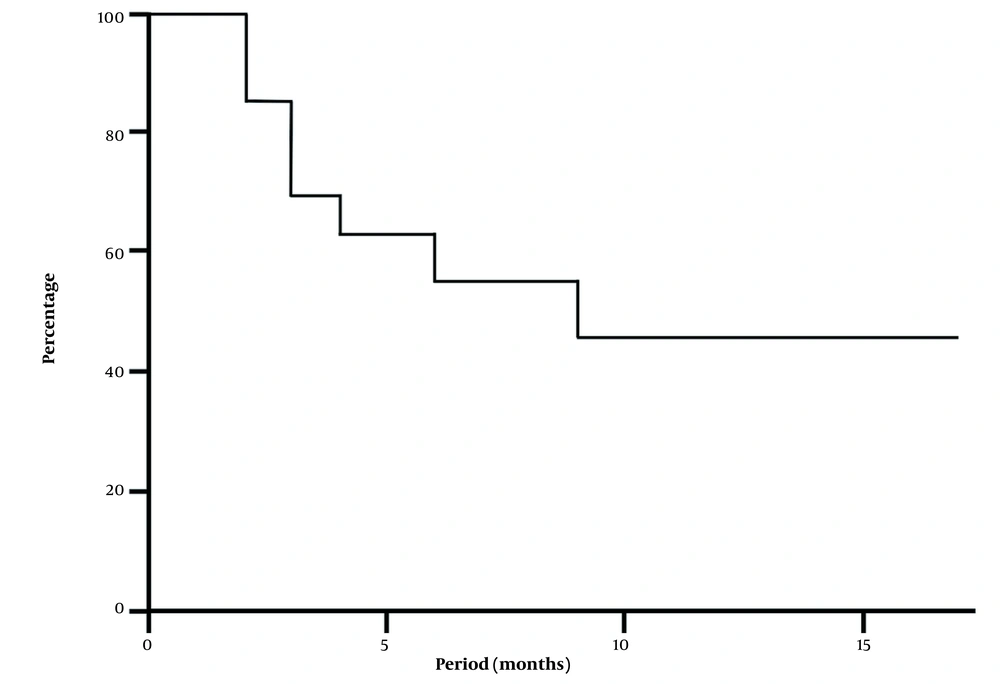
Figure 2 shows a Kaplan-Meier plot reproducing the likelihood of maintained pain relief after a helpful tibial nerve block with steroids in painful feet (n = 38 in 20 patients). The after-treatment estimation differed from 2 to 20 months, and the median value was 9 months. At 1.5 years, 45% of the made-better-feet still had benefits.
The outpatients with a helpful tibial nerve block for painful feet at 7 weeks were set side by side with patients without an effect (Table 2). The presence of unlimited walking distance, a lower mean temperature of the foot, and less minus dA before the intervention were statistically significant coupled with a beneficial effect of a tibial block. Additionally, a lower mean temperature of the foot, less negative dA, a greater dBM, and a greater negative dBT, all set side by side with the mean temperature of the foot 20 minutes after the block, were statistically significant, connected to a positive result of therapy.
| Helpful Tibial Nerve Block (n = 37) | Failed Tibial Nerve Block (n = 39) | P-Value | |||
|---|---|---|---|---|---|
| Prevalence (%) | Mean, SEM | Prevalence (%) | Mean, SEM | ||
| Age (y) | 61, 2.0 | 60, 2.4 | 0.977 | ||
| Gender (male) | 37 | 31% | 0.931 | ||
| Diabetic (yes/no) | 11 | 15% | 0.526 | ||
| Limited walking distance (m) | 52 | 76% | 0.035 b | ||
| Thermographic measurements before the procedure (°C) | |||||
| Mean temperature | 24.4, 0.31 | 25.4, 0.34 | 0.040 b | ||
| Difference temperature at ROI A and mean temperature | -0.2, 0.12 | -0.7, 0.20 | 0.043 b | ||
| Difference temperature at ROI BM and mean temperature | 2.1, 0.14 | 2.1, 0.15 | 0.978 | ||
| Difference temperature at ROI BL and mean temperature | 0.4, 0.15 | 0.1, 0.15 | 0.173 | ||
| Difference temperature at ROI CM and mean temperature | -0.3, 0.12 | 0.1, 0.19 | 0.102 | ||
| Difference temperature at ROI CL and mean temperature | -0.9, 0.10 | -1.0, 0.12 | 0.487 | ||
| Difference temperature at ROI GT and mean temperature | -1.2, 0.17 | 0.2, 1.43 | 0.076 | ||
| Thermographic measurements after the procedure (°C) | |||||
| Mean temperature | 24.7, 0.41 | 26.0, 0.40 | 0.027 b | ||
| Difference temperature at ROI A and mean temperature | -0.2, 0.16 | -0.7, 0.23 | 0.040 b | ||
| Difference temperature at ROI BM and mean temperature | 2.1, 0.16 | 1.5, 0.23 | 0.036 b | ||
| Difference temperature at ROI BL and mean temperature | 0.3, 0.18 | 0.1 0.19 | 0.371 | ||
| Difference temperature at ROI CM and mean temperature | -0.2, 0.13 | 0.1, 0.16 | 0.093 | ||
| Difference temperature at ROI CL and mean temperature | -0.8, 0.12 | -0.7, 0.18 | 0.478 | ||
| Difference temperature at ROI GT and mean temperature | -1.2, 0.24 | -0.3, 0.23 | 0.008 b | ||
Abbreviation: SEM, standard error of the mean; ROI, region of interest.
a A, BM, BL, CM, CL, GT: Specific measure points at the plantar feet (see methods).
b Significant.
4.1. Thermographic Image of a Successful Tibial Nerve Block
Multivariate statistical analysis of the findings of the thermal imaging before and after the tibial nerve block showed dBT as a predictor of a positive tibial nerve block (proportion correct = 0.633). The discriminant analysis computed the interrelationship of dBT with the consequence of the tibial nerve block. If dBT was smaller than -0.9°C, 60% of the patients had a prosperous tibial nerve block, compared to 29% if the dBT was -0.9°C or higher. The used criteria have a sensitivity of 59% and a specificity of 65% in prognosticating a worthwhile tibial nerve block with steroids in painful feet. The positive and negative predictive values were 75% and 53%, respectively.
The prospect of a tibial nerve block in individuals with foot pain was specified for the existence of a dBT smaller than -0.9°C shown on thermography before and after the block (Table 3). A dBT smaller than -0.9°C both on thermography before and after the tibial nerve block can predict a beneficial tibial nerve block. A single thermograph of the plantar foot 20 minutes after the block can best estimate the probability of a beneficial tibial nerve block in sufferers of painful feet.
| Difference in Temperature Between the Big Toe and the Average Temperature of the Foot Less Than -0.9°C Before the Procedure (%) | Total (%) | ||
|---|---|---|---|
| No | Yes | ||
| Difference of temperature between the big toe and the average temperature of the foot less than -0.9°C following the procedure (%) | |||
| No | 30 (n = 23) | 13 (n = 8) | 28 (n = 32) |
| Yes | 44 (n = 9) | 67 (n = 33) | 62 (n = 42) |
| Total (%) | 36% (n = 33) | 58 (n = 43) | |
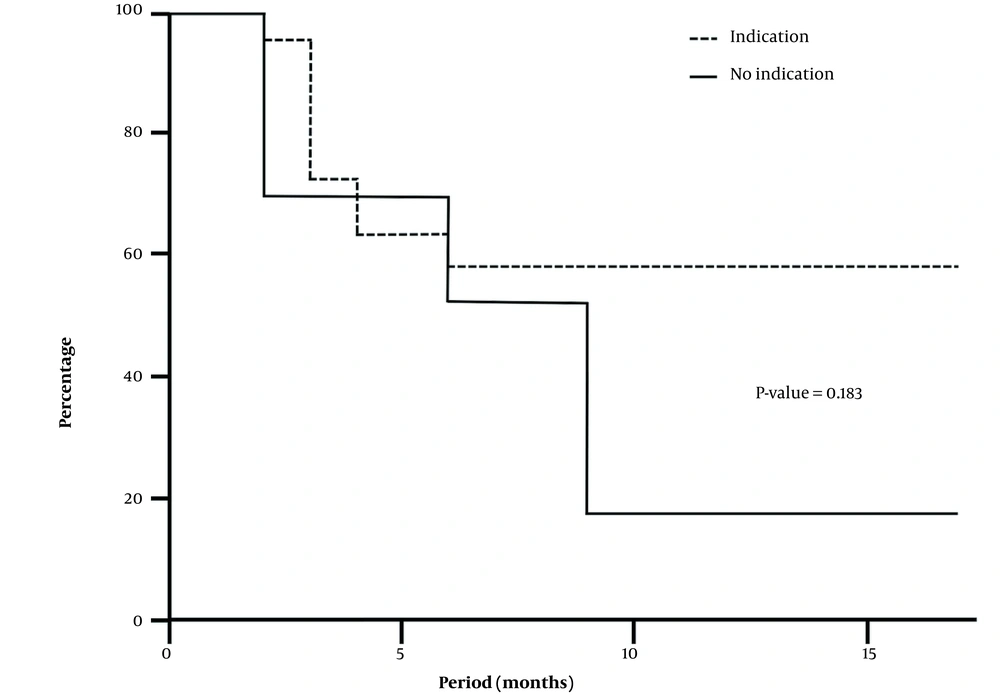
Figure 3 depicts the Kaplan-Meier survival curves of the 38 subjects with a beneficial tibial nerve block differentiating for the existence of a dBT smaller than -0.9°C on thermography before the tibial nerve block. Pain relief persisted in almost 60% of the cases with a dBT smaller than -0.9°C for over 1 year, compared to nearly 20% of the subjects without such discrepancy.
Kaplan-Meier curves for the probability of sustained pain relief after successful tibial nerve block with steroids in feet with (indication) and without (no indication) a difference between the temperature of the big toe and the average temperature of the foot of less than -0.9°C on thermography before posterior tibial nerve block
5. Discussion
Sufferers of chronic foot pain were characterized as female subjects (69%) aged over 50 years and restricted walking distance (63%). Of these subjects, 53% responded with pain relief following a tibial nerve block with steroids, and 22% responded with an advanced walking range. Adverse events were uncommon, with a 5% chance of aggravation of pain and a 5% chance of muscle cramps after the block. At 18 months, 45% of the successfully treated feet still had benefits. The thermography of the plantar foot can predict a beneficial tibial nerve block with steroids on painful feet. A gap between the big toe’s temperature and the foot’s mean temperature smaller than -0.9°C before and after the block can predict successful treatment.
Foot pain is common, with a widespread presence of up to 30%, and senior individuals, females, and stout individuals are in danger of lower leg pain (2, 7). Other treats for foot pain are the stance and misuse of the foot, such as planus (low-arched), cavus (high-arched), over-pronated, or over-supinated feet (2). The origins of foot pain are not entirely identified; however, musculoskeletal conditions are indicated as the main reason for chronic foot and/or ankle pain, with peripheral neuropathy as the second cause (2, 8, 9).
Although the administration of perineural steroids has been put forward as a treatment for neuropathic pain, there is hardly any evidence of perineural steroids for patients with foot pain (5). A study of 120 patients treated with perineural steroids for neuropathic pain of the foot reported less pain at 1 - 3 months (10). Another study of injection therapy with anesthetics and corticosteroids of the tibial nerve for foot pain stated relief in 67% of patients without serious adverse events (3). The present study showed a success rate of 53% and minor adverse effects of 10%. Unlike earlier studies, the current study also investigated the long-term benefits of the tibial nerve block and demonstrated that 45% of the successful blocks lasted more than 18 months. Therefore, tibial nerve block with steroids provides a safe, minimally invasive treatment option in nearly 50% of the sufferers of chronic foot pain, which can last long term. In addition, some patients can notice a greater walking distance.
Currently, foot pain is largely managed conservatively with foot orthotics, medications, and intra-articular injections (3). Intra-articular corticosteroid injections are worthwhile in the short term (3). Custom foot orthoses reduced foot pain and improved foot function, particularly for a long time, compared to corticosteroid injection (11, 12). Tricyclic antidepressants, selective serotonin-norepinephrine reuptake inhibitors, and calcium-channel anticonvulsants can be prescribed for neuropathic pain with a low chance for a 50% reduction of pain (13). Given the outcome of conservative therapy, the tibial nerve block should be considered, especially when custom foot orthoses have been proven inadequate for pain relief or walking distance improvement.
Thermography has great potential for improving the diagnosis of neuropathy (6, 14). Dysfunction of a nerve or a local musculoskeletal disorder could be linked with varying temperature patterns, such as local hypothermia or hyperthermia of an extremity (14-16). The measurement of skin temperature with infrared thermography has been claimed as an objective method to appraise the sequel of regional blocks, such as epidural anesthesia, infraclavicular brachial plexus block, and lumbar sympathetic block (17-19). The authors of the present study were interested in whether the use of thermography of the plantar foot before and after a tibial nerve block could provide clues about the likelihood of future outcomes. A gap between the big toe’s temperature and the foot’s mean temperature of less than -0.9°C both on thermography before and after the tibial nerve block can predict the beneficial effect of the treatment. It seems that the tibial nerve block makes this distinction even more clear. In the present study, the thermography of the plantar foot predicted the outcomes of tibial nerve block but not explicitly enough to make it usable in clinical practice.
This study has some limitations. The proposed statements are restricted by the backward-looking design and the limited total number of individuals in this study. A controlled study with a placebo injection with more patients and with special attention to plantar pressure is more appropriate to appraise the consequences of tibial nerve block in persistent foot pain and the manner of walking. This study used a classic anatomical landmark guided block technique for tibial nerve block with a volume of local anesthetic of more than 3 mL for a better success rate (20). An ultrasound-guided block technique can achieve more successful nerve blocks (21). Therefore, further prospective studies comparing both block techniques for (long-term) effects and thermographic prediction are suggested to better determine the consequences of tibial nerve block with steroids in individuals with chronic foot pain. A prospective study should also include enduring better walking as an objective.
5.1. Conclusions
In patients with chronic foot pain in the present study, 53% responded with less pain on a tibial nerve block with steroids, and 22% responded with greater walking distance. Moreover, 49% of the treated feet had a reduction in pain. Adverse events were uncommon and minor. Therefore, a block of the tibial nerve with steroids provided a safe treatment for 53% of the patients with foot pain, and when it is successful, it can last long term. The tibial nerve block should be considered when custom foot orthoses have been inadequate for pain relief or restricted walking distance. The thermographic imaging of the plantar foot can predict only to a small extent the beneficial effect of the tibial nerve block with steroids on foot pain.