1. Background
Percutaneous transforaminal endoscopic discectomy (PTED) is a modern and effective method for the removal of symptomatic lumbar spine hernias that improves refractory pain syndromes (1). This surgical procedure has become a desirable procedure for lumbar disc herniation (LDH) due to its safety, minimal invasion of surrounding tissues, reduction of bleeding during surgery, short hospital stay, and faster return of the patient to daily activities (2). Providing patient analgesia during PTED surgery is performed through various methods of general anesthesia, sedation, local anesthesia (LA), and epidural anesthesia (EA). To prevent damage to the nervous system, it is best for the patient to be alert during this procedure to report pain due to possible nerve damage (3, 4).
Recently, the use of LA has been considered; however, in clinics, it does not provide the desired analgesia and causes prolonged surgery, increased radiation exposure, and patient and surgeon dissatisfaction. The EA is a good option for patient analgesia during surgery due to the patient’s awakening, providing optimal analgesia, and the possibility of patient neurological monitoring (5). However, studies describing the short-term and long-term safety of using epidural blocks in PTED are rare. Zheng et al. conducted a systematic review to compare the safety of EA and LA. A meta-analysis, including six studies, revealed EA as a safe method in PTED (6).
Due to the posterior interlaminar approach and easier identification of anatomic orientation, some studies have also used interlaminar epidural injections for patient analgesia (7). Nevertheless, in this study, by selecting S1 transforaminal epidural blocks for patients’ Pain, due to the simplicity of the technique and the possibility of few side effects, the surgeon can perform the block, and the exposure time and the length of the surgery are also reduced (6).
2. Objectives
This study investigated the efficiency of the S1 epidural block during surgery.
3. Methods
3.1. General Information
This retrospective study was performed on patients who underwent PTED with the S1 epidural block from May 2020 to May 2021. This study was registered in the Research Council of Shahid Beheshti University of Medical Sciences, Tehran, Iran (ethics code: IR. SBMU RETECH.1400.752). The study protocol was in accordance with the Declaration of Helsinki. All the included patients were informed about the purpose of the study, and written consent was obtained from the parents.
This study evaluated 60 patients with LDH from May 2020 to May 2021 who underwent PTED with the S1 epidural block. All hernia patients had L4 - L5 level and unilateral clinical signs, and supportive treatments were not effective after 6 - 12 weeks. The patients subjectively scored their satisfaction out of 10 at intervals before surgery, during surgery, and 48 hours after surgery.
3.2. Criteria for Inclusion and Exclusion
3.2.1. Inclusion Criteria
(1) Patients with a definitive diagnosis of LDH who did not recover after 6 - 12 weeks of supportive and medical treatment and underwent PTED at L4 - L5 level, with the S1 epidural block;
(2) Patients with an age range of 18 - 65 years and American Society of Anesthesiologists grades 1 and 2.
3.2.2. Exclusion Criteria
(1) History of receiving anticoagulants or coagulopathy;
(2) Systemic or local infection at the surgical site;
(3) History of allergies to the drugs used in the study;
(4) History of severe cardiovascular, liver, kidney, and hematology diseases;
(5) Mental disorders;
(6) Lumbar disc herniation in more than one level;
(7) History of lumbar surgery;
(8) Spondylosis or anatomical disorder in the lumbar region.
3.3. Surgical Procedure
Before the operation, an intravenous Line G 18 is inserted for the patient, and the patient is monitored for heart rate, blood pressure, blood oxygen, and electrocardiogram. The patient is placed in the prone position, and a pillow is placed under the abdomen to reduce lumbar lordosis. After prep and drop, the desired sacral surface for the block was identified in the fluoroscopic anterior-posterior view. Line up the superior S1 end plate by tilting the beam cephalad. Squaring off the superior S1 end plate by tilting the fluoroscope cephalad provides an initial starting point for optimizing visualization. The dorsal S1 foramen is better visualized with a slight ipsilateral oblique view. The surgeon places the spinal needle 25 coaxially into the fluoroscopic beam. The needle enters the S1 foramen after hitting the inferior aspect of the S1 pedicle and walk-off superior. Then, 1 - 2 cc of contrast agent is injected to see the S1 epidurogram, and 12 cc of 1% lidocaine is injected to achieve the aim of sensory-motor separation. After analgesia, all the patients underwent transforaminal endoscopy by a surgeon. All the patients were awake during surgery and received no adjuvant intravenous sedation (Figure 1).
3.4. Clinical Evaluation
All the patients were followed up using a questionnaire before, during, and 48 hours after surgery. Pain, cooperation during surgery, and patient and surgeon satisfaction as primary results, and mean arterial pressure and patient heart rate as secondary results were asked in this questionnaire.
The visual analog scale (VAS) was used to measure the degree of back or leg pain in patients. The VAS is characterized by a score range of 0 - 10. Higher scores indicate more severe pain. In this way, a 10 cm line was drawn on the paper; the beginning and end of the line were marked with 0 and 10, and then the patient was asked to show the amount of pain on it (8). According to the patient’s pain in different degrees, the VAS score was classified as follows:
0: Painless;
1 to 3: Slight pain;
4 to 6: Moderate tolerable pain;
7 to 10: Unbearable severe pain.
Patient and surgeon subjective satisfaction was recorded by a numerical scale. Accordingly, the numbers 8 - 10, 4 - 7, and less than 4 showed high satisfaction, average satisfaction, and dissatisfaction of the patient or surgeon, respectively. The surgeon graded the cooperation of patients during surgery. In assessing patient cooperation during surgery, the absence of inappropriate or unwanted movements of the patient during surgery indicates good cooperation, and the presence of these movements occasionally shows moderate cooperation. If the patient’s movements disrupt surgery, it shows poor patient cooperation. The time between the onset of EA and the start of surgery (i.e., surgical onset time), the volume of intraoperative bleeding, and the duration of surgery were also recorded.
3.5. Statistical Assessment
All quantitative variables are expressed as mean ± standard deviation, and qualitative variables are expressed as numbers (percentages). Additionally, a paired t-test was used to compare quantitative variables between the two different times. Statistical tests were performed in two domains at a significant level of 5%, and SPSS software (version 26) was used for data analysis.
4. Results
4.1. Patient Demographics
Of the 60 patients evaluated in this study, 61.7% and 38.3% were female and male, respectively. The patients’ mean age and weight values were 42.98 ± 10.79 years and 74.27 ± 9.83 kg, respectively (Table 1).
| Gender | No. (%) |
|---|---|
| Female | 31 (61.7) |
| Male | 23 (35.3) |
4.2. Clinical Results
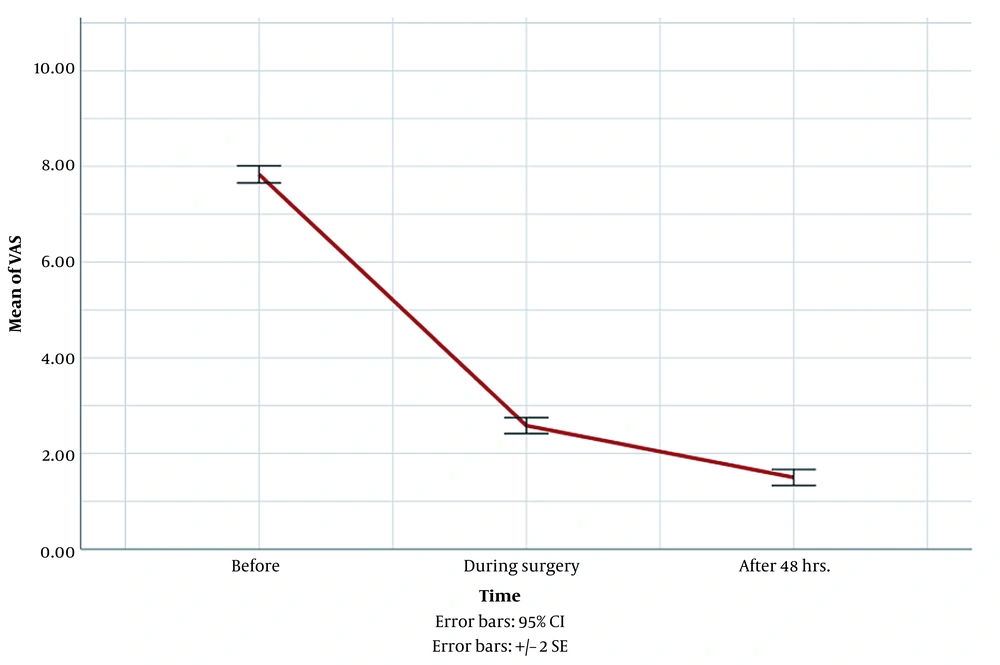
The symptoms of all preoperative patients did not improve with conservative treatment after 6 - 12 weeks. The mean preoperative pain score in these patients was 7.83 ± 0.69, which decreased to 2.58 ± 0.65 during surgery and 1.50 ± 0.65 48 hours after surgery. Moreover, 48 hours after surgery, the postoperative pain score decreased by an average of 7.33 ± 0.04 units, compared to preoperative time, which was statistically significant (P < 0.001) (Figure 2 and Table 2).
| Characteristics | Values |
|---|---|
| Level | |
| L4 - L5 | 60 (100) |
| VAS score | |
| Before surgery | 7.83 ± 0.69 |
| During surgery | 2.58 ± 0.65 |
| 48 hours after surgery | 1.50 ± 0.65 |
Abbreviation: VAS, visual analog scale.
a Values are expressed as No. (%) or mean ± standard deviation.
The mean scores of cooperation, patient satisfaction, and surgeon satisfaction were equal to 1.80 ± 0.40, 8.88 ± 0.69, and 8.98 ± 0.89, respectively (Table 3).
| Variables | Mean ± Standard Deviation |
|---|---|
| Patient cooperation | 1.80 ± 0.40 |
| Patient satisfaction | 8.88 ± 0.69 |
| Surgeon satisfaction | 8.98 ± 0.89 |
In addition, patients’ mean arterial pressure and heart rate at three different times of needle entry into the skin, obturator entry, and endoscope entry had limited changes (Table 4).
| Variables | Values |
|---|---|
| Number of patients | 60 |
| Mean arterial pressure | |
| Needle entry time into the skin | 74.63 ± 11.48 |
| Obturator arrival time | 75.60 ± 11.82 |
| Endoscope arrival time | 75.87 ± 11.87 |
| Heart rate | |
| Needle entry time into the skin | 70.00 ± 7.32 |
| Obturator arrival time | 71.45 ± 6.96 |
| Endoscope arrival time | 71.23 ± 7.29 |
a Values are expressed as No. or mean ± standard deviation.
The mean duration of operation in these patients was 58.58 ± 16.95 minutes, and the mean onset time was 3.12 ± 10.08 minutes. Moreover, the mean bleeding was 124.17 ± 25.20 cc (Table 5).
| Variables | Mean ± Standard Deviation |
|---|---|
| Total operation time | 58.58 ± 16.95 |
| Blood loss | 124.17 ± 25.20 |
| Surgical onset time | 10.08 ± 3.12 |
4.3. Complications
There were no immediate or delayed postoperative complications in these cases.
5. Discussion
This retrospective study evaluated 60 patients with L4 - L5 disc herniation candidates for PTED. In this survey, all the included patients underwent the S1 transforaminal EA. Low back pain is observed in 80% of the general population and is one of the most common complaints with a great impact on society and the economy (9). Disc herniation is a common cause of low back pain and sciatica. Annually, 5 cases per 1,000 individuals develop LDH (10, 11). Lumbar disc herniation can be treated with various methods, such as education, personal care, physiotherapy, medication, interventional pain procedures, and surgery (12, 13). There are several surgical procedures for the treatment of LDH, including open discectomy and minimally invasive procedures.
Open surgery is associated with extensive tissue damage and postoperative pain that will increase the patient’s recovery time and have adverse economic and social effects (14, 15). Currently, open microdiscectomy is still the gold standard treatment for LDH, although without class I evidence. Long-term complications of lumbar microdiscectomy include recurrence, epidural fibrosis, and spinal instability, which can be challenging even for an experienced spine surgeon (10, 16). Due to these microdiscectomy limitations, microendoscopic discectomy was introduced. Advances in the use and design of optics and surgical instruments have led to the use of completely endoscopic surgical procedures, such as endoscopic lumbar discectomy through the skin (3, 17).
Recently, some reports have suggested that PTED could be an alternative treatment for LDH with clinical results comparable to conventional open lumbar discectomy. The advantages of this method include no bone removal, reduction of complications, minor wounds, reduction of bleeding, reduction of fluid requirements, no need for catheterization, reduction of hospitalization period, very low complication rate, rapid recovery, return to work, and reduction of costs. The safety and effectiveness of this treatment have been confirmed by several randomized studies (18-20). On the other hand, because this procedure is performed under LA or EA, the patient is conscious during surgery, and damage to the spinal cord is prevented (13, 21).
Managing patient pain during surgery is very important for patient and surgeon satisfaction and reduction of costs (8). Patient analgesia using LA does not have the side effects of general anesthesia; however, according to previous studies, it has not provided good pain control in patients, especially when implanting working channel and foraminal expansion, which is practically difficult to continue surgery due to the patient pain and, in some cases, requires the use of general anesthesia to continue surgery (22-24). In previous studies, EA has provided acceptable analgesia compared to LA. During this method, the patient is awake and does not feel pain due to sensory-motor separation but can move his/her toes; therefore, the general anesthesia method is preferable in preventing nerve damage and the possibility of monitoring the patient by the surgeon (24, 25). The disadvantages of EA include increasing the time of exposure to radiation, an increase in surgery time, and a long learning curve (22).
Almost all studies showed better pain management in patients who underwent EA. Zhen et al. conducted a meta-analysis, including 1660 patients (26). It was revealed that the intraoperative VAS score in patients with EA was significantly lower than in patients who received LA (26). Similarly, Sun et al. showed that the intraoperative and postoperative lumbar and leg VAS scores in the EA group were significantly lower than LA (27). Another meta-analysis comprising six studies and 529 patients confirmed the same results (6). Consequently, intraoperative and postoperative pain control is significantly better in EA. In this study, the mean VAS score decreased significantly after 48 hours.
In 2022, Zhang et al. included 160 PTED candidates and divided them into two groups, one receiving transforaminal EA and the other LA (28). They showed that the satisfaction rate and lumbar and leg VAS scores were significantly lower in the transforaminal EA group (28). A systematic review conducted by Zhen et al. also confirmed that the satisfaction rate is statistically higher among patients who received EA (26). Likewise, in a comparative study, the satisfaction scores between these two groups differed significantly, and the EA group had a higher satisfaction rate (23). The mean subjective satisfaction score of the present survey was 8.88, indicative of high patient satisfaction.
By evaluating 160 patients, it was revealed that patients under transforaminal EA had lower mean arterial pressure and heart rate (28). Moreover, there was a discrepancy in results regarding complications. The findings of Sun et al.’s and Zhen et al.’s meta-analyses showed no difference in adverse events between the two groups (26, 27). The findings of Zhang et al. also showed that the complication rate did not vary between patients who received transforaminal EA and LA (28). However, in a randomized control trial, it was concluded that complications, such as nausea, vomiting, dizziness, and drowsiness, were lower in the EA group (1). The same result was repeated in Zheng et al.’s systematic review (6). Nevertheless, by assessing 132 PTED candidates, postoperative dysuria and decrement of lower limb strength were observed in the EA group (23). Therefore, there is no consistent finding about the comparison of adverse events in the two groups.
Wang et al. conducted a randomized control trial and concluded that immune function had better function in patients with EA (1). Furthermore, the inflammatory indices were higher in LA patients (1). Among the evaluated variables, postoperative Oswestry Disability Index, surgical duration, and X-ray exposure did not differ between the two groups (26, 28).
In this study, with the S1 epidural block, in addition to using the benefits of epidural block in controlling patient analgesia, due to the simplicity of the S1 transforaminal epidural technique and short learning curve, it is possible for the surgeon to provide patient analgesia. Due to sensory-motor separation, when the patient is on analgesic, the surgeon can evaluate the patient during surgery and prevent unwanted complications of nerve damage.
5.1. Study Limitations
This study was conducted as a single-center survey. A multi-center study with a larger number of patients is required to obtain more precise results. A longer period of follow-up helps determine the exact mortality rate and other possible delayed complications.
5.2. Conclusions
The PTED with S1 EA is a safe and effective treatment for LDH. The S1 epidural block technique is simple and can be performed by a surgeon. It also causes good analgesia during the operation and cooperates well with the surgeon due to patient consciousness.