1. Background
Double-lumen tubes (DLT) are the most common tubes used to make anatomical and physiological isolation of the lungs owing to their efficiency and simplicity (1).
Misplacement of the DLT can result in inadequate nonventilated (operative) lung deflation, insufficient lung ventilation, and hypoxemia (2). Therefore, optimal DLT positioning is essential for efficient lung isolation during thoracic procedures with fewer intraoperative complications (3).
The correct placement of a DLT is checked using clinical methods such as auscultation of breath sounds and observation of chest wall movements and using instrumental methods such as fiberoptic bronchoscope (FOB) and lung ultrasound (LUS) (4).
Around 48% of DLTs were misplaced when blind methods were used. The use of FOB is considered the gold standard for confirmation of correct placement of the DLT and has largely replaced conventional blind intubation methods in thoracic anesthesia (5). Unfortunately, FOB has disadvantages such as cross-infection, the need for experienced personnel, and high costs (6). Searching for modalities that reduce the possible risks of cross-infection following the COVID-19 pandemic raised concerns about new tools that can effectively replace FOB. Chest auscultation alone is not reliable for assessing DLT placement as it is subjective and cannot accurately identify DLT misplacement (7, 8).
LUS is a noninvasive method that has been widely employed in airway management in the past years and can be used to assess the placement of the endotracheal tube even in an emergency (4, 9). Even in thoracic surgery, LUS has shown to be a superior approach and enhances auscultation accuracy for determining the proper placement of DLTs due to its high sensitivity and specificity (10, 11). Moreover, LUS is a compelling alternative to FOB because of its simplicity and less required training (12).
2. Objectives
We hypothesized that LUS could be the same as FOB and better than auscultation in determining DLT correct placement. This trial was conducted to assess the accuracy of LUS and auscultation about FOB to detect DLT placement during thoracic surgery in the same patient and, to detect the possibility of using LUS as an alternative to FOB.
3. Methods
This diagnostic accuracy study, conducted according to STARD guidelines, enrolled 120 cancer cases aged ≥ 18 years undergoing thoracic surgery and requiring DLT intubation at the National Cancer Institute (NCI) after obtaining written informed consent and after approval of the Institutional Review Board (IRB: 202101-2P-02002) and registration at clinical trials.gov (ID: NCT04740385) from February 2021 to June 2022.
Cases with expected airway difficulty or an in-situ tracheostomy tube, previous lung surgery, pleural effusion, pneumothorax, pleurodesis, or absent lung sliding sign were excluded. We performed a complete history taking, clinical examination, specifically of the airway, routine laboratory tests, and additional tests based on the patient's medical history.
In the waiting area, all patients were clinically examined using a stethoscope, auscultation, and LUS to confirm the presence of lung sliding signs. Patients with absent lung sliding signs were excluded.
Induction of general anesthesia (GA) was performed by propofol 2 mg/kg and fentanyl 2 µ/kg IV. Laryngoscopy was facilitated by rocuronium 0.6 mg/kg followed by intubation by DLT (COVIDIEN, Shiley) sized (35, 37, or 39 F) according to sex and height. GA was maintained using isoflurane 1 - 1.5% through positive pressure mechanical ventilation and rocuronium top-up doses. All the DLT inserted were left-sided, as, in our institute, we routinely use left DLT except in rare cases where right DLT insertion is mandatory.
After confirmation of intubation by capnography and confirming normal airway pressure, confirmation of DLT placement was done through auscultation in the supine position, then by LUS, and finally by FOB.
All procedures were conducted by two professional anesthesiologists with a complete agreement between them (κ = 0.99).
3.1. Auscultation
After insertion of the DLT, the tracheal cuff was initially inflated, then auscultation of the upper and lower chest zones on both sides were done. This was followed by inflation of the bronchial cuff and repeated auscultation of the same regions, first with the tracheal lumen clamped and finally with the bronchial lumen clamped. Correct intubation of the DLT was confirmed by the existence of symmetrical bilateral lung sounds prior to clamping of the tracheal lumen, then by a reduction in the whole sound of the right lung and the appearance of symmetrical upper and lower lung sounds in the left lung following tracheal lumen clamping. This was followed by a reduction in the whole sound of the left lung and the appearance of symmetrical upper and lower lung sounds in the right lung following bronchial lumen clamping.
Time to confirm tube position was calculated starting from auscultation to the end of DLT position confirmation.
3.2. Lung Ultrasound
After auscultation, an LUS examination was performed on both sides of the anterior and lateral chest wall by low frequency (5 - 10 MHz) curved probe of Sonosite M-Turbo ultrasound machine (FUGIFILM Sonosite, Inc., Bothel, WA 98021, USA). LUS was done on four quadrants bilaterally in the supine position.
LUS scanning was done in eight areas. The chest areas were divided on each side into two anterior and two lateral areas. Anterior areas were outlined from the sternum to the anterior axillary line, while the lateral areas were from the anterior to the posterior axillary line. Each anterior and lateral area was further divided into upper and lower areas from the clavicle to the second-third intercostal spaces and from the third space to the diaphragm. The correct position of the DLT was confirmed with a loss of lung sliding sign on the same clamped lumen side.
Time was calculated from the probe to the chest position until confirmation by the absence of lung pleura sliding.
3.3. Fiberoptic Bronchoscopy
Tube position was initially checked using FOB (Karl Storz, Germany, Tuttlingen, Germany) as a reference standard through the tracheal lumen and then through the bronchial lumen.
The correct DLT placement criteria were: (1) the tracheal rings are seen anteriorly and the muscular stria posteriorly, (2) the bronchial cuff is seen below the carina and just above the left bronchus, (3) the tip of the tube is positioned just above the secondary carina through the bronchial lumen.
The incorrect DLT placement criteria were: (1) absence of the tracheal rings (esophageal or bronchial intubation), (2) too shallow, defined as more than 50% of the right bronchus opening is obscured by the bronchial cuff, (3) too deep, defined as either the bronchial cuff after inflation was totally unseen or when the tip of the bronchial tube is seen under the secondary carina.
To calculate the accuracy of auscultation and LUS compared to FOB:
• True positive (TP) result was described as a situation wherein auscultation, or LUS indicated the correct DLT placement, which was verified by FOB.
• True negative (TN) result was described as a situation in which auscultation or LUS revealed incorrect DLT placement that was verified by FOB.
• False positive (FP) results were described as a situation wherein auscultation, or LUS, revealed a correct DLT placement, but FOB revealed the incorrect placement.
• False negative (FN) results were characterized as a situation wherein auscultation or LUS revealed incorrect DLT placement, which was verified to be accurate following FOB.
The primary outcome was the accuracy of LUS. Secondary outcomes included procedural time and agreement between LUS and FOB findings.
3.4. Sample Size Calculation
Based on the previous paper by Parab et al., 2015 (12), the expected sensitivity of the traditional auscultation method is 75% with 18% specificity. Using 90% power, 5% significance level, and 95% confidence interval, at least 114 patients are required. We added six cases to overcome dropout. Therefore, 120 cases were recruited. The sample size calculation was done based on the Arifin sample size calculator 2017.
3.5. Statistical Analysis
Statistical analysis was done by SPSS v26 (IBM Inc., Chicago, IL, USA). Quantitative variables were expressed as average and standard deviation (SD). Qualitative variables were expressed as frequency and percentage. Times were compared by repeated measure ANOVA. Sensitivity, specificity, and accuracy were measured to validate the DLT placement compared to the FOB findings. Kappa test indicated agreement with FOB results. A two-tailed P value was considered significant.
4. Results
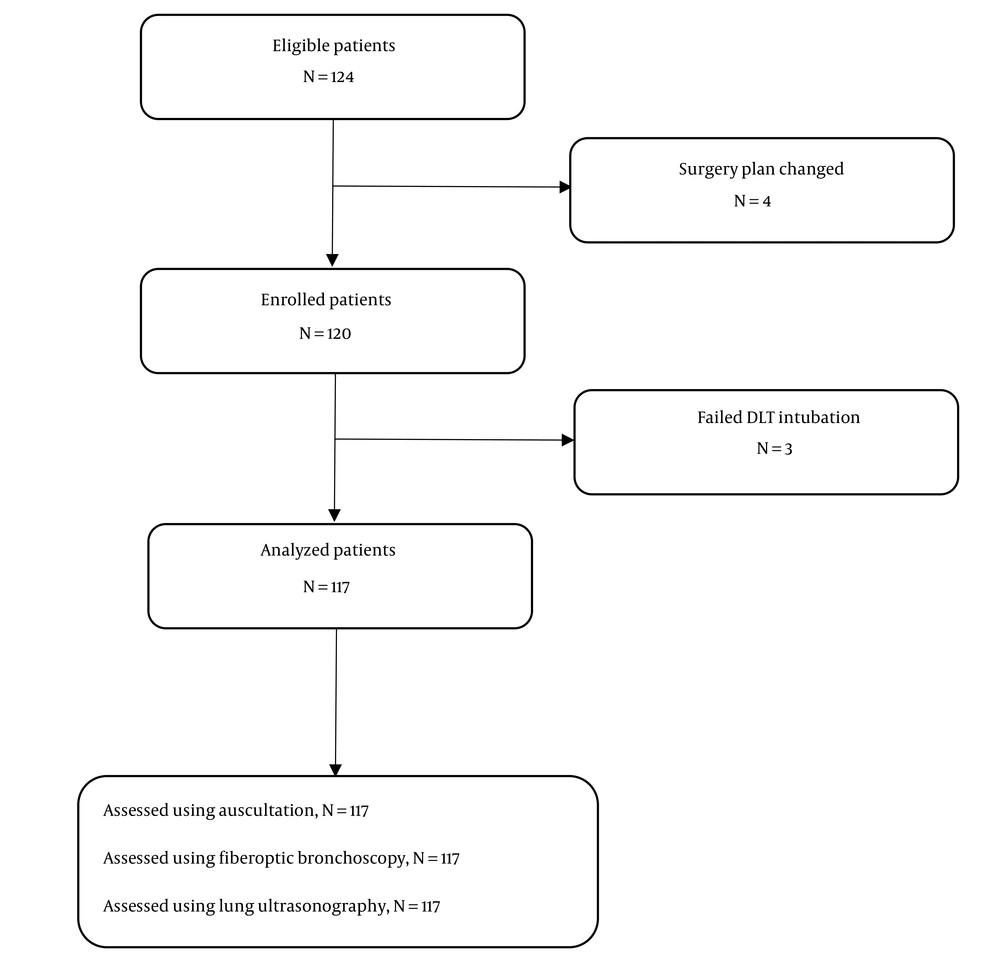
In our study, 139 cases were assessed for eligibility, and 19 cases were excluded (15 patients did not meet the eligibility criteria and the surgical plan was changed in 4 patients). One hundred twenty patients were included, and three dropped out due to failed intubation. Therefore, only 117 cases were analyzed (Figure 1).
Characteristics, type of surgery, and size of inserted DLTs of the studied cases are shown in (Table 1).
| Variables | Values |
|---|---|
| Age (y) | 41.07 ± 15.04 |
| Sex | |
| Male | 79 (67.52) |
| Female | 38 (32.48) |
| Height (m) | 1.61 ± 0.08 |
| Weight (kg) | 65.44 ± 11.27 |
| BMI (kg/m2) | 25.56 ± 4.99 |
| Type of surgery | |
| Lung resection | 75 (64.1) |
| Esophageal | 42 (35.9) |
| Size of inserted DLTs | |
| 35 F | 21 (17.95) |
| 37 F | 77 (65.81) |
| 39 F | 19 (16.24) |
Characteristics, Type of Surgery, and Size of Inserted DLTs of the Studied Cases (n = 117) a
The mean time (± SD) was 59.32± 13.53sec for auscultation, 103.29 ± 9.81sec for LUS, and 58.16± 10.94 sec for FOB (un-tabulated data). Time for LUS was significantly longer than for auscultation and FOB (P-value < 0.001) and insignificantly between auscultation and FOB.
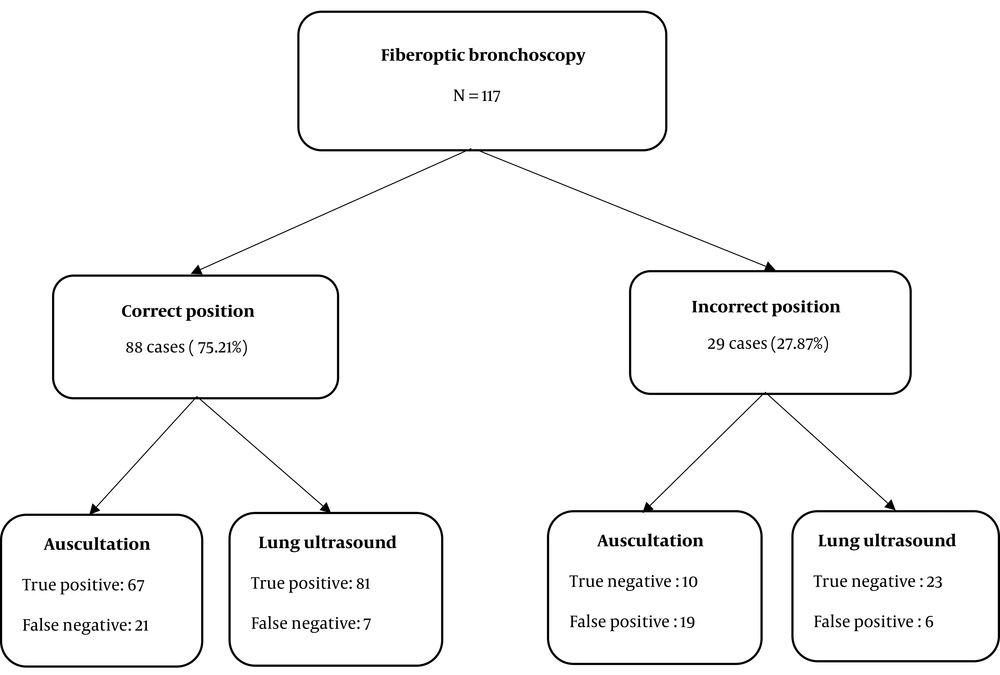
Using FOB for detection of DLT placement, 88 cases (75.21%) were correctly placed, and 29 (27.87%) cases were incorrectly placed in which 10/29 cases (34.48%) the tube was found to be too shallow and 12/29 (41.37%) cases the tube was found to be too deep while 7/29 (24.13%) cases the tube was misplaced (Figure 2, Tables 2 and 3).
| By FOB | ||
|---|---|---|
| Correct | Incorrect | |
| By auscultation | ||
| Correct | 67 | 19 |
| Incorrect | 21 | 10 |
| By LUS | ||
| Correct | 81 | 6 |
| Incorrect | 7 | 23 |
Comparison Between Auscultation and LUS in the Detection of Correct DLT Position Compared to FOB
| By Auscultation (95%CI) | By LUS (95%CI) | |
|---|---|---|
| Sensitivity | 76.1 (65.7 - 84.6) | 92.1 (84.3 - 96.7) |
| Specificity | 34.5 (17.9 - 54.3) | 79.3 (60.3 - 92.0) |
| Accuracy | 65.8 (56.5 - 74.3) | 88.9 (81.8 - 93.9) |
Sensitivity, Specificity and Accuracy
Using auscultation for the detection of DLT placement compared to FOB finding, 67 cases were true positive, 10 cases were true negative, 19 cases were false positive, and 21 cases were false negative (Figure 2 and Table 2).
Using LUS for detection of DLT placement compared to FOB finding, there were 81 cases that were true positive, 23 cases were true negative, 6 cases were false positive, and 7 cases were false negative. Auscultation had 76.14% sensitivity, 34.48% specificity, and 65.81% accuracy in detecting correct DLT placement. LUS had 92.05% sensitivity, 79.31% specificity, and 88.89% accuracy in detecting correct DLT placement (Figure 2 andTable 2).
There was substantial agreement between LUS and FOB (κ = 0.705) and poor agreement between auscultation and FOB (κ = 0.104).
5. Discussion
The correct positioning of DLTs has been considered one of the bases of anesthetic management (13, 14).
FOB is still adopted as the standard gold technique for DLT placement confirmation, although it has limitations (4). Ventilation has been measured with more recent techniques, such as LUS and electrical impedance tomography. LUS provides some benefits, such as wide accessibility, efficiency, and notably reduced exposure to respiratory secretions, consequently lowering operator risk in circumstances where infectious respiratory diseases are present (15). Thus, the benefits of using LUS as a simple, noninvasive tool for confirmation of appropriate DLT positioning recently emerged as a promising modality that can be used as an alternative to FOB with the spread of the novel COVID-19.
In the current study performing the three techniques in the same cohort might give strength in investigating the promising role of LUS as a standard of care in the confirmation of double-lumen tube positioning. In this study, auscultation was done first, followed by LUS, and confirmed by FOB.
In this trial, the accuracy of LUS was 88.89%, while the accuracy of auscultation was 65.81% for the determination of the correct DLT placement. However, the procedure time was higher in LUS compared to FOB and auscultation, and this may be attributed to examining eight areas in the US.
Auscultation is believed to have less accuracy. This reduced accuracy might be because breath sounds audibility is frequently modified by tidal volume, the consistency of the lung tissue, chest wall thickness, the intensity of noise, the stethoscope sensitivity, and individual hearing acuity (4, 13).
Near to the current study results, Parab et al. (4) reported that LUS showed significantly higher accuracy (70.5% vs. 48.9%) with increased sensitivity (94.1% vs. 73.3%), more PPV (57.1% vs. 35.5%), and higher NPV (93.8% vs. 75.0%) compared to auscultation. Additionally, the median time needed for LUS to evaluate DLT position was longer than auscultation (161.5 vs. 114 s, P < 0.001).
Also, Chung et al. (11) found that LUS had higher accuracy than auscultation for detecting DLT misplacement with experts (69.8% vs. 37.5%). Moreover, Sustic et al. (16) reported that LUS had higher accuracy when added to auscultation compared to auscultation alone (88% vs. 72%).
Previous research by de Bellis and his colleagues (17) reported that 37% of the DLTs that were inserted blindly during their study needed repositioning using FOB, whereas 32% of the intubations were initially expected to have a correct position by auscultation but had been proved to be of malposition after FOB; furthermore, 5% were found to be critically mispositioned.
In accordance with our findings, Saporito et al. (18) reported that although FOB is considered the gold standard for detecting DLT placement, LUS can be used as a sensitive, specific, and cost-effective tool in detecting proper tube positioning. On the other hand, they reported that LUS could not completely replace FOB as bronchoscopy offers direct visualization of the DLT position with extra merits that can be offered when FOB is used for tube placement as the facilitation of precise tube placement and guidance in case of right DLT insertion.
The results of the current study showed substantial agreement between LUS and FOB (κ = 0.705) and poor agreement between auscultation and FOB (κ = 0.104). Kanavitoon et al. (3) reported that, as demonstrated by surgical grading, LUS is superior to FOB for obtaining sufficient lung collapse after the correct insertion of a DLT. They concluded that LUS was non-inferior to FOB in detecting proper tube position with subsequent adequate lung collapse.
One of the limitations of the current study included that intraoperative tube displacement couldn’t be assessed using LUS and necessitated the use of FOB; however, tube displacement is not the main point addressed by this study where the study investigates the possibility of using LUS as a possible alternative to the routine use of FOB during the assessment of tube placement.
5.1. Conclusions
In the current study, the authors concluded that LUS is more accurate than auscultation for determining DLT placement. LUS is non-inferior to fiberoptic bronchoscopy in detecting DLT placement with good diagnostic accuracy. Thus, using LUS stepwise may be beneficial in certain circumstances, such as a shortage of FOB availability or in the presence of infection in favor of limiting its transmission. Consequently, with continued advances in ultrasound technology, LUS may become a promising alternative to FOB.