1. Background
The postoperative period is an essential part of the patient’s surgical experience. Postoperative pain affects recovery from surgery. Pain management is a vital constituent in the postoperative care of surgical patients. There are various methods to relieve postoperative pain following lower limb orthopedic surgery, including the epidural infusion of local anesthetics and opioids, pericapsular nerve blocks, intravenous (IV) patient-controlled analgesia, and paravertebral nerve blocks. Each method has its advantages and disadvantages (1-5).
Epidural analgesia provides magnificent analgesia, negates the stress response involved in the surgery, reduces postoperative morbidity, and expedites postoperative functional recovery. Opioids are frequently used in epidural anesthesia either alone or in combination with local anesthetics. Local anesthetics administered with opioids increase the extent of analgesia, reduce the repeated administration of the drug, and therefore result in fewer systemic side effects (6, 7).
Buprenorphine is a semisynthetic lipophilic opioid derived from thebaine with potent agonistic activity at µ receptors and antagonistic activity at the ƙ receptor. Buprenorphine is 25 - 50 times more potent than morphine. Butorphanol is a lipophilic opioid with weak μ receptor agonist and antagonist activity and potent ƙ receptor agonism. Numerous studies compared epidural local anesthetics to dexmedetomidine, fentanyl, clonidine, and morphine in lower limb orthopedic surgery (8, 9). There is a paucity of data on comparing epidural buprenorphine and butorphanol as adjuvants to bupivacaine for postoperative analgesia in lower limb orthopedic surgery. The better adjuvant between these two still needs to be explored. Therefore, the present study focused on the efficacy of epidural buprenorphine versus butorphanol as adjuvants to bupivacaine in lower limb orthopedic surgery.
2. Objectives
This study aimed to investigate the onset of analgesia, duration of analgesia, sedation score, and side effects of butorphanol with bupivacaine versus buprenorphine with bupivacaine.
3. Methods
After obtaining the approval of the institutional ethics committee (Sri Siddhartha Medical College, Siddhartha Academy of Higher Education) and informed consent from patients, 100 patients aged 18 - 60 years posted for lower limb orthopedic surgery were selected for the study. A detailed history, thorough clinical examination, and routine investigations were carried out.
3.1. Inclusion Criteria
The inclusion criteria were American Society of anesthesiologists (ASA) grades I and II, an age range of 18 - 60 years, undergoing elective orthopedic lower limb surgery (e.g., fracture neck femur, fracture shaft femur, intertrochanteric fracture of the femur, and fracture of upper end of the tibia), and body mass index (BMI) ≤ 25 kg/m2.
3.2. Exclusion Criteria
The exclusion criteria were cardiac, respiratory, or central nervous system disorders, hepatic and renal dysfunction, bleeding diathesis, history of allergy to local anesthetics, contraindication to spinal and epidural anesthesia, complex pain syndrome, and using opioids.
The patients were advised to have an overnight fast of 8 hours for solid food. On arrival to the operating room, the IV line was secured with an 18-gauge cannula under aseptic precaution and ringer lactate solution infused at 10 - 20 mL/kg. The patients were allocated by computer-generated randomization into group A, receiving bupivacaine (anawin 0.5%, Neon Laboratories, Mumbai, India) with buprenorphine (buprigesic 0.3 mg, Neon Laboratories, Mumbai, India), and group B, receiving bupivacaine and butorphanol (butodol 2 mg, Neon Laboratories, Mumbai, India) epidurally. Under all aseptic precautions, an 18 G Tuohy needle (B Braun Prefix epidural set, Curit Pharmaceuticals, Ahmedabad, India) was introduced into L2 - L3 interspace, epidural space identified by the method of loss of resistance technique for air. Lignocaine 2% with epinephrine (1: 200000) (3 mL) was injected after securing the epidural catheter as a test dose. A 27-gauge Quincke needle (Bectan, Dickinson India Pvt Ltd., Chennai, India) was introduced at the L3 - L4 intervertebral space, and 3.4 mL of bupivacaine 0.5% heavy (anawin 0.5% hyperbaric, Neon Laboratories, Mumbai, India) was injected into subarachnoid space after confirming the backflow of cerebrospinal fluid. Intraoperative heart rate, blood pressure, oxygen saturation, and electrocardiogram were monitored throughout the procedure.
An anesthesiologist who was not part of the study was involved in the administration of the local anesthetics and opioids through the epidural catheter when the patient complained of pain [the visual analog scale (VAS) > 4]. The study drugs were prepared by a different anesthesiologist who was not part of the study. Therefore, the patients and the anesthesiologist, who administered the drugs and collected the data in the postoperative period, were blinded to the study design. Accordingly, double-blinding was achieved throughout the study.
Following the surgical procedure, the patient was shifted to the postoperative ward, and when the patient complained of pain (VAS > 4), the study drug was administered through the epidural catheter. Group A received 10 mL bupivacaine 0.125% with 0.3 mg buprenorphine. Group B received 10 mL bupivacaine 0.125% with 2 mg butorphanol. The patients were taught to read the VAS the night before the surgery.
Pain monitoring was assessed using the VAS, with 0, 1 - 3, 4 - 7, and 8 - 10 scores indicative of no, mild, moderate, and severe pain, respectively. Sedation was assessed by Ramsay sedation scores of 1, 2, 3, 4, 5, and 6, indicative of anxious and agitated, cooperative/oriented/tranquil, asleep and responding to verbal command, asleep but brisk response to light stimulus, sluggish response to a painful stimulus, and asleep without response to a painful stimulus, respectively. The pain was monitored after 15 minutes, 30 minutes, 1 hour, 2 hours, 4 hours, 8 hours, 10 hours, 12 hours, 16 hours, 20 hours, and 24 hours in the postoperative recovery room. The patient’s sleep was not disturbed if the patient did not complain of pain. The IV diclofenac sodium 75 mg mixed in 100 mL normal saline was started if the patient complained of pain despite receiving epidural opioids. This procedure was used as rescue analgesia. The onset of analgesia (VAS < 4, time from the injection of study medication to the first reduction in pain intensity to almost complete relief of pain) and duration of analgesia (time from epidural injection to the time of request for additional analgesia and VAS > 4) was assessed. The injection of diclofenac sodium aqueous mixed with 100 mL of normal saline was started after 24 hours of the study as analgesia.
The patients were monitored for any side effects, such as respiratory depression, nausea, vomiting, and pruritus. The study subjects were monitored for hypotension (i.e., a decrease in systolic blood pressure > 20% of the baseline value or systolic blood pressure < 90 mmHg), bradycardia (i.e., a pulse rate < 60 beats per minute treated with IV atropine 0.6 mg), and respiratory depression (i.e., a respiratory rate less than 8 breaths per minute or saturation <95% treated with O2 supplementation and respiratory support if needed).
3.3. Sample Size Calculation
Calculate the sample size using the following formula:
Outcome variable = Mean duration of analgesia (6).
Z-value for 5% level of significance:
- Power (80%) = 0.84
- Standard deviation (σ) = 87.84
- Effect size (d) = 50
The minimum sample size required was 48 subjects in each group (total n = 96). A sample of 50 patients in each group was included in the study (total n = 100).
3.4. Statistical Analysis
The data were copied into Microsoft excel sheets. Statistical analysis was carried out using SPSS software (version 22). Quantitative measurements were presented as mean ± standard deviation and categorical measurements in numbers and percentages. The independent sample t-test was used to test for differences between the two groups. The chi-square test was used to determine relationships between the categorical data (i.e., age, gender, BMI, and ASA grading). The significance level was assessed at 5%.
4. Results
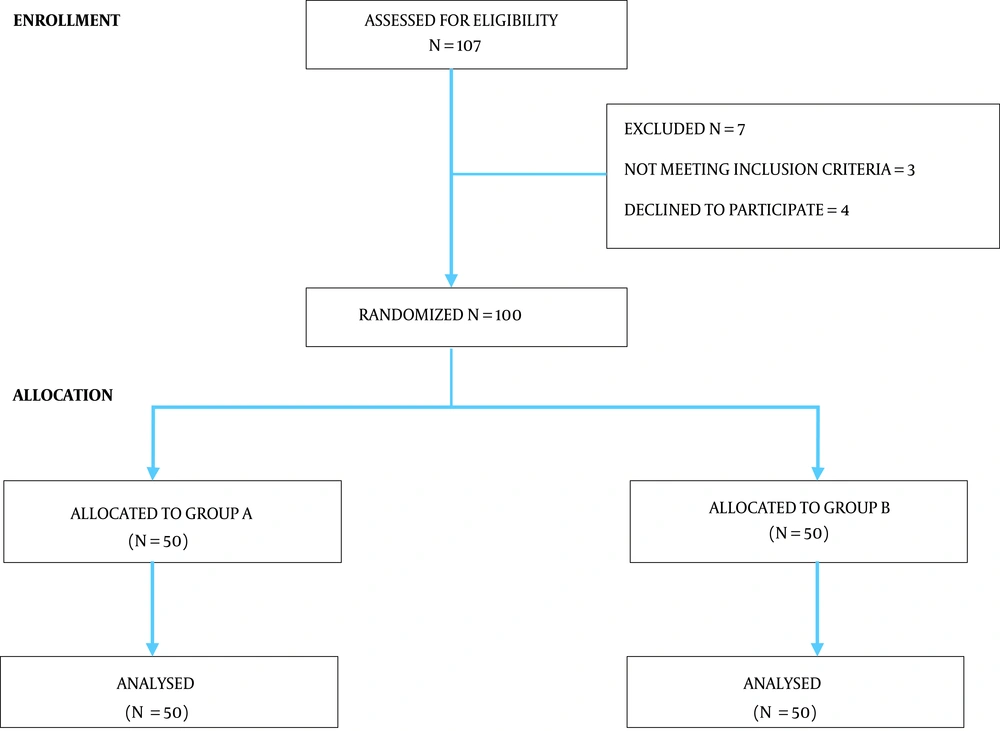
A total of 107 patients were enrolled in the study. Three patients were excluded for not meeting the inclusion criteria, and four patients declined to participate (Figure 1). The mean age, BMI, gender, and duration of surgery of subjects in groups A and B did not significantly differ (Table 1). The onset of analgesia in group A was significantly less (7.7 ± 1.6 vs. 12.6 ± 1.7 minutes, P < 0.001) than in group B. The difference in the duration of analgesia between group A and group B after the first dose of the corresponding drugs was significant (590 ± 40 vs. 480 ± 54 minutes, P = 0.009) (Table 2).
a Two-sample t-test.
b Chi-square test.
| Analgesia | Mean ± SD | P-Value a |
|---|---|---|
| Onset of analgesia (min) | < 0.001 | |
| Group A | 7.7 ± 1.6 | |
| Group B | 12.6 ± 1.7 | |
| Duration of analgesia after the first dose (min) | 0.009 | |
| Group A | 590 ± 40 | |
| Group B | 480 ± 54 |
a Two-sample t-test
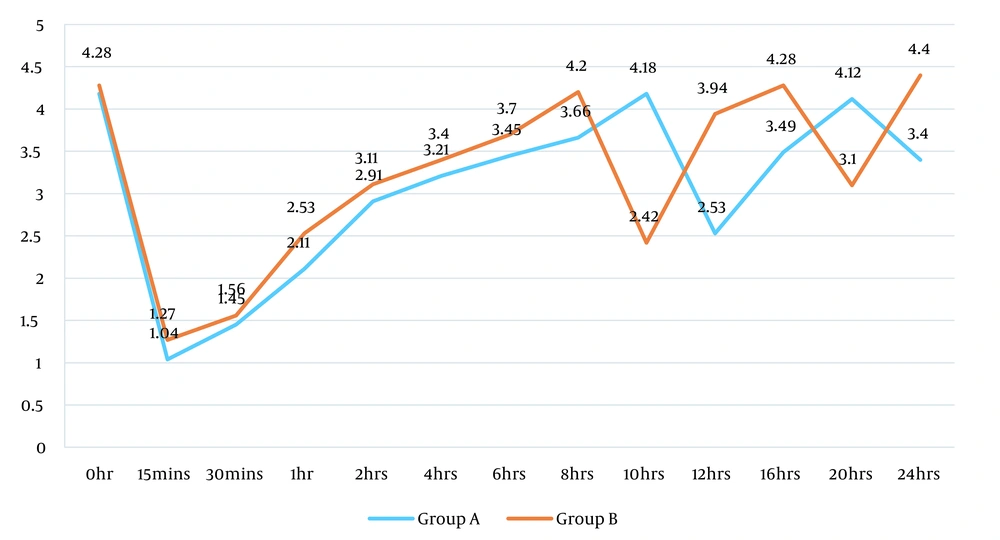
The accepted pain level on VAS to determine the wash-out effect of the drugs was 4. Regarding the VAS scores between groups A and B, the patients in group A crossed this accepted pain score at 10 hours, compared to group B which crossed at 8 hours. This is reflective evidence that indicates the longer duration of analgesia in group A than in group B, which was significant (Figure 2). The sedation scores in groups A and B were observed to be significant after 2 hours and remained better up to 24 hours after drug administration. However, there was no significant difference in the sedation scores between the groups (Figure 2, Appendix 1).
Among the clinical parameters, the pulse rate was observed to be significantly higher in group B than in group A (P < 0.001) (Appendices 2 and 3). However, although oxygen saturation and respiratory rates were significant at some time points, most of the time points were not significant (Appendices 4 - 7). Mean arterial pressure was significantly higher in group B than in group A (P < 0.001) (Table 3). Among side effects, nausea was often reported first in both groups, followed by vomiting and pruritus (Appendix 8).
| Mean Arterial Pressure | Groups | t-Value | P-Value a | |
|---|---|---|---|---|
| Group A | Group B | |||
| 0 hr | 92.8 ± 7.4 | 98.9 ± 14.6 | -2.650 | 0.009 |
| 15 mins | 89.7 ± 8.7 | 92.8 ± 15.1 | -1.268 | 0.208 |
| 30 mins | 79.6 ± 3.5 | 89.9 ± 14.0 | -5.031 | 0.000 |
| 1 hr | 84.0 ± 3.6 | 89.0 ± 12.6 | -2.698 | 0.008 |
| 2 hrs | 81.9 ± 4.0 | 88.6 ± 12.9 | -3.511 | 0.001 |
| 4 hrs | 82.6 ± 4.1 | 85.6 ± 9.0 | -2.108 | 0.038 |
| 6 hrs | 82.8 ± 3.9 | 84.6 ± 7.2 | -1.808 | 0.048 |
| 8 hrs | 83.4 ± 2.4 | 92.8 ± 15.1 | -1.981 | 0.048 |
| 10 hrs | 89.6 ± 8.6 | 89.9 ± 12.1 | -1.168 | 0.208 |
| 12 hrs | 79.4 ± 4.5 | 89.0 ± 12.6 | -5.307 | 0.000 |
| 16 hrs | 84.1 ± 5.6 | 88.5 ± 9.9 | -2.698 | 0.008 |
| 20 hrs | 81.6 ± 4.9 | 85.6 ± 10.2 | -3.511 | 0.001 |
| 24 hrs | 82.6 ± 6.3 | 83.2 ± 7.8 | -4.261 | 0.000 |
a Two sample t-test.
5. Discussion
The current study examined the effect of buprenorphine 0.3 mg and butorphanol 2 mg on postoperative pain. It was observed that the onset and duration of analgesia were better with buprenorphine than with butorphanol combination with bupivacaine. The beneficial effects of epidural analgesia on postoperative pain are well known. In this study, epidural analgesia was selected to control postoperative pain because it reduces neuroendocrine stress response, central sensitization of the nervous system, and muscle spasm. Epidural analgesia involves the comprehensive analgesia of all structures covering the operated site. However, local infiltration techniques might miss painful anatomical tissue structures (10, 11).
Some studies have explored that epidural opioid analgesia is more effective than systemic and IV patient-controlled analgesia in decreasing postoperative pain (12). Epidural local anesthetic drug administration alone has never been widely used due to significant failure rates due to regression of sensory block and incidence of motor block and hypotension when used for postoperative analgesia. Epidural opioids are routinely used for the management of postoperative pain. They have an advantage over local anesthetics in the sense that they provide quality analgesia without causing sympathetic and motor blockade. However, there is evidence that epidural opioids do not suppress the catabolic response to surgery as profoundly as local anesthetics (13). A combination of local anesthetic with an opioid is the most commonly used technique based on the observation that their combination limits the regression of local anesthetic alone and improves the dynamics of pain relief.
Naik et al. compared the effects of bupivacaine 0.125% to butorphanol 3 mcg/kg (8 mL) and bupivacaine 0.125% with buprenorphine 2 mcg/kg (8 bmL) and concluded that the onset and duration of analgesia were better with buprenorphine than butorphanol (6). Jose et al. discussed the effects of epidural bupivacaine with buprenorphine and epidural bupivacaine with butorphanol, wherein buprenorphine showed a higher mean value of visual analgesia at the first hour (39 vs. 22, P < 0.001) suggesting a faster onset of action and better analgesia with buprenorphine than butorphanol (14). The current study demonstrated similar results. Agarwal et al. also demonstrated a better quality of analgesia in patients receiving a combination of epidural bupivacaine with buprenorphine (15).
Gayatri and Lakshmi compared the effectiveness of epidural buprenorphine and butorphanol as postoperative analgesics in laparoscopic surgeries. They found that epidural buprenorphine significantly increased the quality of analgesia and reduced pain. The duration of analgesia was also longer in the buprenorphine group than in the butorphanol group (566.17 ± 73.14 vs. 325 ± 47.42, P < 0.001); nevertheless, side effects were more in the buprenorphine group (16). Another study conducted by Kumar and Kaladhar demonstrated that the onset of analgesia was faster in the butorphanol group than in the buprenorphine group; however, analgesia duration was longer in the buprenorphine group (17). Various studies have demonstrated that buprenorphine is effective as an analgesic for postoperative pain (18-20).
Wolff et al. identified that the extent of analgesia was 620 minutes with epidural buprenorphine; nevertheless, the extent was 580 minutes with epidural morphine, which is consistent with the present study’s findings (21). Gupta et al. compared butorphanol and tramadol in their study. Sedation scores were significantly higher in the butorphanol group, which is in line with the present study’s findings (22).
The sedation score was significantly higher in the butorphanol group than in the buprenorphine group in the current study. Respiratory depression was not noticed in both the study groups. Nausea, vomiting, and headache were more frequent in the buprenorphine group. However, pruritus was observed to be more frequent in the butorphanol group. No other complication was observed in either of the groups. A study performed by Ackerman et al. demonstrated that epidural butorphanol and buprenorphine showed a low incidence of pruritus (23).
5.1. Limitations
The limitation of this study was its modest sample size. The next limitation was regarding the equipotent drugs administered in the study. The doses of the drugs were selected depending on the previous studies. An optimal dose of both opioids needs to be determined.
5.2. Conclusions
It was concluded that buprenorphine added to bupivacaine provides earlier onset and longer postoperative epidural analgesia than epidural butorphanol.