1. Background
The International Association for the Study of Pain has defined pain as an unpleasant feeling and mental experience associated with potential or real tissue damage (1). Pain is one of the most common symptoms and signs of diseases that informs an individual of a dysfunction in a part of the body (2, 3). Following all surgical procedures, patients experience pain unavoidable in various degrees (4).
On the other hand, cesarean section is one of the most significant and common surgical procedures in obstetrics and gynecology to save the lives of mothers and children in difficult deliveries (5, 6). In cesarean section, there is acute pain due to complex physiologic reactions against histological damage, visceral stretch, and uterine contractions (7). In poor control and insufficient management of pain, some adverse effects may occur on different body systems, such as the inability to discharge secretions of the respiratory system, increased blood pressure and heart rate, and prolonged bed rest, thereby increasing the risk of deep vein thrombosis, delayed breastfeeding, and inappropriate neonatal nutrition (7).
To relieve post-cesarean pain, opioids and nonsteroidal anti-inflammatory drugs (NSAIDs) are widely used (8). For a long time, opioid drugs have been the main choice for postoperative pain relief (9). Pethidine (meperidine) is the most frequently used opioid during delivery. Meperidine binds to the opioid receptors of the central nervous system, thus inhibiting the ascending pain pathway and reducing pain perception (10). However, opioids are used less due to adverse effects, including respiratory depression, nausea, vomiting, slow gastrointestinal function, and reduced consciousness, delaying rehabilitation and movement. Nowadays, various methods are suggested to decrease opioid use, one of which is to use non-opioid drugs along with or as a substitute for narcotic drugs (11).
Paracetamol (an analgesic and antipyretic medication) is administered intravenously before, during, and after surgery (11). The use of this drug before surgical incision (preemptive) has shown favorable effects on postoperative pain in different studies (11, 12). Besides the early return of bowel function and quicker improvement, non-opioid analgesics do not affect breastfeeding and have no respiratory weakness, drug abuse potential, and low narcotic effects (13).
Paracetamol is a non-opioid antipyretic and analgesic drug (14) that acts by inhibiting the production of prostaglandins. It is one of the most highly consumed drugs worldwide (14). The onset of its analgesic effect ranges from 5 to 10 minutes, and its maximum effect is 1 hour, lasting from 4 - 6 hours (15).
2. Objectives
Given the significance of post-cesarean pain control, as well as the side effects of opioid analgesics, this study was conducted to determine the preoperative analgesic effect of intravenous paracetamol on post-cesarean pain control.
3. Methods
The proposal of the present study was approved by the Research Council of Rafsanjan University of Medical Sciences (No. 841), as well as by the Ethics Committee of Rafsanjan University of Medical Sciences (code: IR.RUMS.REC.1395.115). In addition, it was registered on the Iranian Registry of Clinical Trials website (code: IRCT20150519022320N17).
In this randomized, double-blind clinical trial, 240 pregnant women aged 18 - 40 years were enrolled; they were referred to Niknafas Maternity Hospital in Rafsanjan, Iran, for elective cesarean section. The sample size was determined based on the study by Jabalameli et al. (16). The trial design was parallel, and the allocation ratio was 1: 1. Exclusion criteria were patients with a history of cardiovascular diseases, hypertension, diabetes, hepatic/renal failure, psychiatric disorders, specific drug dependency, and drug abuse, as well as those prohibited from paracetamol or meperidine consumption. Exclusion criteria were confirmed through a questionnaire before surgery. In addition, patients undergoing general anesthesia, receiving meperidine during surgery, or having complicated surgery were excluded from the study and replaced by new patients.
The study was performed during 2017 - 2018. Patients’ medical histories were recorded. The study and pain severity measurement method and consumption of drugs and their side effects were explained to the patients. Then, a questionnaire, including demographic information and research variables, was completed for each patient; in addition, informed written consent was obtained from all participants.
The patients who agreed to participate in the study were randomly assigned to paracetamol (n = 120) and control (n = 120) groups. We used the simple randomized pairing method. Patients with general entry conditions were divided into 2 groups by throwing coins. The operating room nurse determined the group of each patient, and the patients’ group was recorded in their own record sheet. The surgeon, researchers, and patients were unaware of the groups.
All patients kept Nil Per Os (NPO) for 8 hours, during which the hydration therapy was prepared according to the 1, 2, and 4 rules using Ringer’s solution (Shahid Ghazi Pharmaceutical Co., Tabriz, Iran). The paracetamol group received 10 mg/kg paracetamol intravenously (Exir Pharmaceutical Co., Borujerd, Iran) dissolved in 100 mL of normal saline (Shahid Ghazi, pharmaceutical Co., Tabriz, Iran) 15 minutes before surgery. The control group received 100 mL of normal saline intravenously 15 minutes before surgery. The patients were blinded to the type of groups. The drug was administered before surgery by a nurse who was not part of the research team, and the patient was immediately transferred to the operating room. All patients received 10 mL/kg Ringer’s solution intravenously before spinal anesthesia and 10 mg metoclopramide (Daru Pakhsh Co., Tehran, Iran). Spinal anesthesia was performed in a sitting position by spinal needle No. 25 (Dr J, China) and 2.5 mL of Marcaine 0.5% (Mylan, France), totally 12.5 mg. After performing spinal anesthesia and reaching the appropriate anesthetic level (T4), cesarean section was carried out. If the mean arterial pressure (MAP) dropped more than 20% of the base level, the patient received 5 mg of ephedrine (STEROP, Brussels, Belgium). When the baby was delivered, 1 mg of midazolam (Tehran Shimi Co., Tehran, Iran) was administered intravenously to all patients. A trained anesthetic technician recorded vital signs at baseline (after placement on the bed and performing anesthesia) and then every 15 minutes until the end of surgery and 1 hour after surgery, as well as nausea, vomiting, and chills during and after surgery. All patients underwent spinal anesthesia by a single anesthesiologist, and a single surgeon performed the operations. The surgeon and the anesthesiologist were not part of the research team.
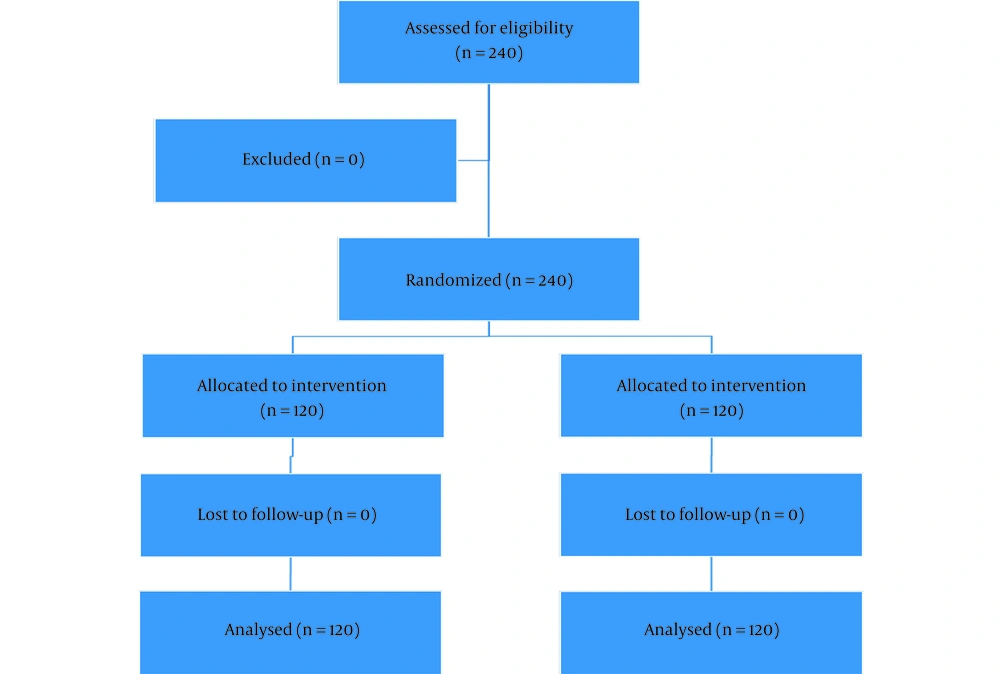
After surgery, a recovery nurse taught the patient how to use the visual analogue scale (VAS). Zero showed no pain, and 10 indicated the worst level of pain (17). VAS was recorded by trained nurses 1, 2, 4, 6, 12, and 24 hours after surgery. These nurses were blinded to the patient groups. The pain score was determined by a VAS scoring ruler (Figure 1). If VAS was > 5, the patient was visited by a physician, and if prescribed, meperidine (25 mg) was administered by the nurse. Also, the mean dose of meperidine intake was recorded in the first 24 hours. The obtained data were analyzed using SPSS version 18 (SPSS Inc., Chicago, Ill, USA) and parametric and non-parametric statistical tests (t test, chi-square, and Mann-Whitney). The t test was used to compare demographic parameters, and the chi-square test was used to compare qualitative parameters, such as chills and nausea. The Mann-Whitney test was used for the following variables: Scores of pain, meperidine consumption, pulse rate, and systolic and diastolic blood pressures. P values less than 0.05 were considered statistically significant. A summary of the steps taken is given in the flowchart below (Figure 2).
4. Results
In the present study, 240 pregnant women referred for elective cesarean section were included and divided into 2 equal groups (n = 120). The average age of the participants was 31 years, and the average height, weight, and body mass index (BMI) were 159 cm, 79 kg, and 31 kg/m2, respectively.
All study participants received their own therapeutic interventions and completed the study. No participants were excluded from the study after the randomization. Therefore, the data of all participants were used in all analyzes. The Mann-Whitney test was performed for the following variables: scores of pain, meperidine consumption, pulse rate, and systolic and diastolic blood pressures.
The results of the independent t test showed no significant difference between the 2 groups in weight, height, age, and BMI (Table 1).
| Variables | Paracetamol | Control | Total | P Value |
|---|---|---|---|---|
| Age (y) | 31.55 ± 7.13 | 30.64 ± 6.72 | 31.10 ± 6.96 | 0.310 |
| Weight (kg) | 80.06 ± 12.61 | 79.57 ± 14.90 | 79.82 ± 13.77 | 0.787 |
| Height (m) | 158.73 ± 9.83 | 160.43 ± 5.87 | 159.60 ± 8.08 | 0.118 |
| BMI | 31.58 ± 5.06 | 30.81 ± 5.74 | 31.19 ± 5.42 | 0.290 |
Comparison of Age, Weight, Height, and Body Mass Index Between the Paracetamol and Control Groups a
The findings of the chi-square test showed no significant difference between the two groups in the frequency of post-surgery chills and nausea (Table 2).
| Variables and Index | Paracetamol | Control | Total | P Value |
|---|---|---|---|---|
| Chills | 0.315 | |||
| Yes | 15 (12.6) | 18 (15.7) | 33 (14.1) | |
| No | 104 (87.4) | 97 (84.3) | 201 (85.9) | |
| Nausea | 0.198 | |||
| Yes | 24 (20) | 18 (15) | 42 (17.5) | |
| No | 96 (80) | 102 (85) | 198 (82.5) |
Frequency of Post-cesarean Chills and Nausea in Pregnant Women in the Paracetamol and Control Groups a
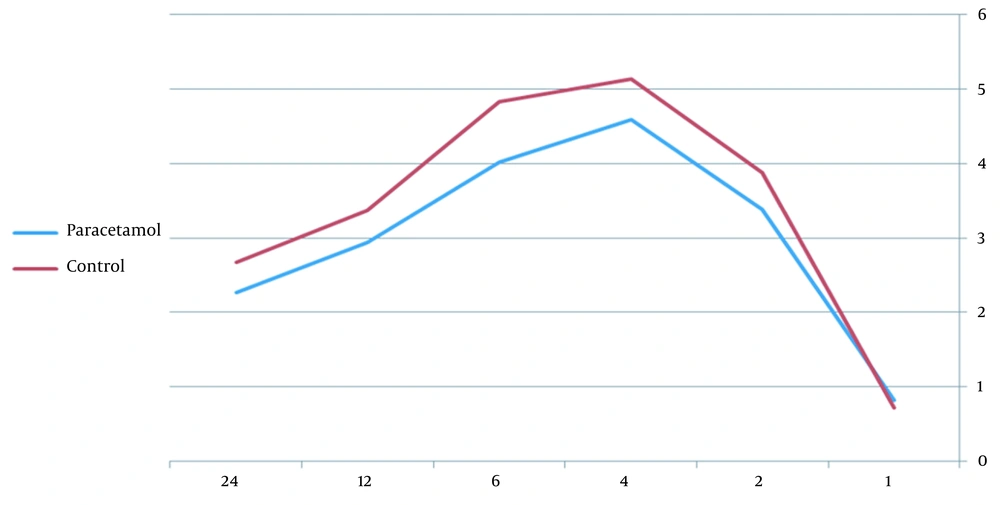
The statistical test revealed that the mean pain scores 6 and 24 hours after surgery were significantly lower in the paracetamol group than in the control group (Table 3). There was no significant difference between the 2 groups in the mean pain scores at other times. Figure 1 shows the changes in mean pain scores in both study groups over time (Table 3).
| Group | 1 Hour | 2 Hours | 4 Hours | 6 Hours | 12 Hours | 24 Hours |
|---|---|---|---|---|---|---|
| Paracetamol | 0.82 ± 1.83 | 3.38 ± 2.43 | 4.58 ± 2.58 | 4.01 ± 2.22 | 2.94 ± 1.78 | 2.26 ± 1.85 |
| Control | 0.72 ± 1.48 | 3.87 ± 2.45 | 5.13 ± 2.36 | 4.83 ± 2.35 | 3.37 ± 1.92 | 2.67 ± 1.80 |
| P value | 0.573 | 0.108 | 0.082 | 0.008 | 0.072 | 0.038 |
Mean and SD of Pain Scores at Different Hours After Surgery in the Paracetamol and Control Groups
Meperidine consumption 24 hours after surgery was lower in the paracetamol group than in the control group, but it was not statistically significant (Table 4).
| Groups | Pethidine (mg); Mean ± SD |
|---|---|
| Paracetamol | 34.78 ± 12.47 |
| Control | 40.53 ± 58.12 |
| P value | 0.245 |
Mean Consumption of Pethidine 24 Hours After Surgery in the Paracetamol and Control Groups
The Mann-Whitney test indicated no significant difference between the 2 groups in the mean pulse rate at all study times (Table 5).
| Variables | Control | Paracetamol | P Value |
|---|---|---|---|
| 15 minutes | |||
| Pulse rate | 94.31 ± 19.46 | 91.21 ± 19.87 | 0.397 |
| Systolic blood pressure (mm Hg) | 107.17 ± 19.70 | 107.67 ± 20.36 | 0.786 |
| Diastolic blood pressure (mm Hg) | 63.42 ± 12.73 | 60.67 ± 12.88 | 0.046 |
| 30 minutes | |||
| Pulse rate | 94.75 ± 17.47 | 96.62 ± 17.75 | 0.428 |
| Systolic blood pressure (mm Hg) | 104.42 ± 19.35 | 99.83 ± 20.66 | 0.273 |
| Diastolic blood pressure (mm Hg) | 57.81 ± 14.74 | 55.67 ± 14.07 | 0.255 |
| 45 minutes | |||
| Pulse rate | 96.81 ± 14.83 | 93.78 ± 14.00 | 0.094 |
| Systolic blood pressure (mm Hg) | 107.48 ± 15.36 | 103.17 ± 14.38 | 0.053 |
| Diastolic blood pressure (mm Hg) | 57.63 ± 13.31 | 54.50 ± 12.08 | 0.042 |
| 60 minutes | |||
| Pulse rate | 97.84 ± 16.63 | 95.40 ± 12.66 | 0.499 |
| Systolic blood pressure (mm Hg) | 109.39 ± 13.33 | 106.81 ± 14.18 | 0.228 |
| Diastolic blood pressure (mm Hg) | 58.20 ± 13.17 | 57.93 ± 13.09 | 0.885 |
Mean and SD of Pulse Number, Systolic Blood Pressure, and Diastolic Blood Pressure at Different Hours After the Start of Surgery in the Paracetamol and Control Groups a
Another parameter investigated in our research was the mother’s blood pressure. The results of the statistical test showed no significant difference between the study groups at different times in terms of mean systolic blood pressure (Table 5), but a significant difference was seen between the 2 groups in diastolic blood pressure at 15 and 45 minutes after starting the operation (Table 5).
There were no unwanted side effects in the 2 groups.
5. Discussion
This study was conducted on 240 pregnant women undergoing cesarean section. The results showed that since postoperative pain was a very common complication, especially in cesarean section, preoperative administration of intravenous paracetamol could have a significant analgesic effect and reduce the required meperidine after surgery. This result was obtained by measuring postoperative pain in patients using VAS and the amount of post-cesarean meperidine used.
In the present study, paracetamol was administered as preemptive. The purpose of this method was to block pain receptors before painful stimulation. In the studies of Ong et al. and Arici et al., paracetamol was administered in the same manner (11, 12).
Most studies have emphasized the analgesic effects of paracetamol. Kiliçaslan et al. compared the patients’ post-cesarean pain scores in 2 groups (n = 25), one receiving intravenous paracetamol plus tramadol and one receiving tramadol alone. They concluded that the pain score was lower in the paracetamol group than in the control group (18). Inal conducted a study on 50 patients under cesarean surgery and compared the analgesic effects of paracetamol and meperidine. They found that paracetamol led to a reduction in pain scores in patients (19). Faiz et al. compared intravenous paracetamol and ketamine injection in controlling pain after an abdominal hysterectomy. The pain score (VAS) was significantly lower in the paracetamol group than in the control group; the highest difference was seen 6 hours after surgery (20). This result is in agreement with the results of the present study. In another study, Ali and Khan compared the analgesic impact of tramadol plus paracetamol and tramadol alone on 60 patients undergoing laparoscopic surgery, obtaining the same results as presented above (21). Cattabriga et al. investigated the analgesic effect of paracetamol on postoperative pain in patients undergoing cardiac surgery, reporting that intravenous paracetamol could induce appropriate analgesic effects in patients (22). In all studies mentioned above, the frequency of administration and the total dose of narcotic analgesics were reduced when paracetamol was administered. In our study, although the difference between the 2 groups was not statistically significant for meperidine intake, meperidine administration was clinically lower in the paracetamol group.
Vuilleumier et al. conducted a study in Switzerland in 1998, comparing the postoperative analgesic effect of paracetamol and morphine. They found that paracetamol could be used as a substitute for morphine to induce postoperative analgesia in moderate pain. They reported that morphine had a better short-term analgesic effect, but finally, paracetamol had a longer analgesic effect (23). Nikoda and Maiachkin conducted a study in Russia in 2002, examining the postoperative analgesic effects of paracetamol on 30 patients. They showed that paracetamol reduced the severity of postoperative pain (24). In another study, Emir et al. compared the analgesic effect of tramadol plus paracetamol and tramadol alone on spinal surgery and reported a higher efficacy of paracetamol (25). Mofidi et al. also conducted a study on 80 patients with renal pain, finding that intravenous paracetamol is a safe and effective drug with no remarkable side effects in relieving pain in renal patients. They also reported that paracetamol had a higher efficacy and fewer complications than tramadol in renal patients (26).
In the present study, paracetamol was administered preoperatively. Although the peak efficacy was 1 hour, and the duration of effect was 4 to 6 hours, the pain score was significantly reduced at 6 and 24 hours postoperatively. In the study by Arici et al., the effect of preoperative and end-of-operation injections of paracetamol was compared with the control group in abdominal hysterectomy. There was a significant difference between the pain scores of the 2 intervention groups and the control group. Although the difference in pain scores was not significant in the 2 intervention groups, it was clinically lower in the preemptive group than in the other groups; this effect remained for up to 24 hours. Morphine consumption was lower in the intervention groups than in the control group. The difference between the 2 intervention groups was statistically significant. The amount of morphine consumption in the two intervention groups was lower in the group administered paracetamol before the operation than in the group administered at the end of the operation (12). Consistent with our study, they reported that the analgesic effect of paracetamol was longer than the drug effect duration. These results may be caused by pain receptors blocked before painful stimulations. In addition, cutting off pain signals can prevent central nerves from becoming sensitive.
However, some studies have shown no significant difference between the analgesic effect of paracetamol and narcotic analgesics, such as the study by Van Aken et al. that compared the analgesic effects of paracetamol and morphine in dental surgery (27) and the study by Rawal et al. that compared the analgesic effect of oral tramadol and intravenous paracetamol in outpatient surgeries (28). The differences between the results of these 2 studies with our and other results appear to be due to differences in the extent of surgery. However, in these articles, paracetamol had no weaker effect than the other 2 drugs.
In our study, side effects, such as nausea and chills, were reported in both groups. Previous studies have mostly reported significantly fewer side effects in the paracetamol group than in the control group due to the reduced total dose of the narcotic drug (29, 30).
The pain had a descending trend in both groups during the study period, which is in agreement with the patient’s gradual improvement and reduction of neural damage. Generally, the pain level was different in both groups; pain reduction was greater in the paracetamol group than in the control group; this difference is statistically significant at 6 and 24 hours after surgery. This result is similar to some studies, such as the study of Sinatra et al. that investigated the effect and safety of single and repeated administration of 1 g of intravenous paracetamol for pain management following large orthopedic surgery (31), the study by Olonisakin et al. that investigated the saving effect of intravenous paracetamol on using morphine for postoperative pain control in women (30), and the study by Iqbal that investigated the analgesic level and quality of postoperative intravenous paracetamol and reduction of narcotic requirement (32).
However, some studies, such as the study by Uysal et al. on the comparative analysis of the efficacy of intravenous paracetamol vs. tramadol for postoperative analgesia in pediatric adenotonsillectomy (33), the study by Kiliçaslan et al. on the effect of intravenous paracetamol on postoperative analgesia and tramadol on cesarean section (18), and the study by Lee et al. on the effect of paracetamol, ketorolac, and paracetamol plus morphine on pain control after thyroidectomy, showed no significant difference between the 2 groups in terms of pain reduction; the only advantage was faster rehabilitation (34).
The present study found nausea and chills in the paracetamol and control groups, but no significant difference was observed. Sanjar Mousavi and Khalili reported dizziness, nausea, headache, vomiting, sleepiness, and immobility in both groups received paracetamol and opioid for postoperative pain relief, but no significant difference was observed between the groups (35).
The findings of the present study indicated no significant difference between the 2 groups in systolic blood pressure in different measurement stages during and after cesarean; however, diastolic blood pressure was significantly lower in the paracetamol group than in the control group 15 minutes after the start of the cesarean section. Further, diastolic blood pressure was significantly lower in the paracetamol group than in the control group 45 minutes after the start of the cesarean section. In a systematic review by Turtle et al., it was shown that in many studies, paracetamol increased blood pressure; however, in 2 studies, no effect was observed, and in 1 study, hypotension was observed. Therefore, they concluded that the effect of paracetamol on blood pressure was unclear (36). Beyzaei et al. showed that systolic blood pressure had significant changes over time in both groups; it was reduced 3 hours after surgery and then raised again; however, no significant difference was found between the 2 groups. Similarly, their results showed significant changes in diastolic blood pressure over time in both groups; however, the difference was not statistically significant between the 2 groups (37). According to the results of the present study and the above-mentioned studies, further studies are needed to further investigate the effect of paracetamol on blood pressure.
Since drugs have specific pharmacogenetic effects, the results of this study can be extended to other races and communities.
5.1. Strengths and Limitations
The strength of this study is that none of the participants were excluded from the study, and due to the study design and the absence of unwanted complications, the results of the study can be generalized to the entire population of pregnant women.
The limitation of this study is that only pregnant women referred for elective cesarean section were included in the study, and the study was not conducted on women in the labor phase who had pain before emergency cesarean section; conducting a study on these women may show different results.
5.2. Conclusions
The preemptive intravenous administration of paracetamol induced great analgesic effects on post-cesarean pain and reduced the frequency and total dose of meperidine despite a statistically insignificant difference. If future studies confirm this result, intravenous paracetamol can be used extensively as an adjuvant medication or even a substitute for opioids in cesarean.