1. Background
Osteoarthritis (OA) is the most common form of joint disease and is one of the 10 main causes of disability worldwide. Knee is the most commonly involved joint by osteoarthritis. With increasing aging of population as well as obesity, knee OA has become a major public health problem and important financial burden for the global economy. OA is the commonest joint disease worldwide with around 300 million people and mainly occurs in later life. It tends to be slowly progressive and can cause significant pain and disability. The burden of OA is physical, psychological and socioeconomic. It can be associated with significant disability, such as a reduction in mobility and activities of daily living. Psychological sequelae include distress, devalued self-worth and loneliness. Given the high frequency of OA in the population, its economic burden is large (1-3).
Pain mitigation is still a primary goal in treating patients with knee OA. There are various therapeutic methods for treatment of knee OA including nonpharmacological methods such as, exercise therapy and oral medications. If these methods fail to prove effectiveness, intraarticular injections (corticosteroid, visco-supplements, and blood-derived products) are other nonsurgical resorts to be considered (3).
For many years, corticosteroid injection has been applied for treatment of arthritis including knee osteoarthritis (4). It is recommended by American College of Rheumatology guideline for treatment of knee osteoarthritis (5).
There is good evidence supporting effects of intraarticular steroid injections on OA pain. Although its benefits may be limited to few weeks, some patients have noted pain reduction up to several months. Despite significant pain reduction, its use is not free of side effects. Short-term complications of corticosteroids include skin atrophy and depigmentation at the site of injection, post-injection flare up and thus increased pain and elevation of blood glucose in diabetic patients. Several human and animal studies have indicated accelerated arthritis process which can lead to degradation and loss of articular cartilage after intraarticular corticosteroid injections, especially recurrent ones. On the other hand, risk of septic arthritis should never be underestimated. Considering these concerns, it is generally recommended that intraarticular steroid injections should be limited to 3 to 4 times per year (4-6).
Among other injection methods, prolotherapy has been shown to be effective in promotion of tissue healing at the site of injection including joint cartilage, tendons and ligaments around the joint. It effects through different mechanisms such as elevating the level of growth factors or boosting the effectiveness of growth hormones. There are different injectable solutions such as sodium morrhuate and phenol for prolotherapy (7), but dextrose is the most commonly used one which creates a mild inflammatory state in response to cellular stress, leading to release of cytokines and hence enhanced activity of growth factors, thereby inducing proliferation of tissue specific healing cells (8). A significant advantage of dextrose is being cheap and easily available. In addition to knee osteoarthritis, dextrose prolotherapy has been used for treatment of different pathologies such as rotator cuff tendinitis (9) and lateral epicondylitis (10).
There are 3 main methods of prolotherapy (11). The most popular one consists of intraarticular injection of treatment agent. Myofascial prolotherapy is injection of soft tissue (ligaments and tendons) around the joints and under the subcutaneous fascia. The neurofascial prolotherapy approach involves an injection in the area of penetration points of peripheral sensory nerves reaching the subcutaneous tissue. According to Hilton's law, nerves innervating the skin over a joint also innervate the joint and the muscles affecting that joint (12). Bennett found that sensory nerves are vulnerable to neuropraxia or axonal damage at the point of skin penetration which is called chronic constriction injury (13). This chronic injury leads to inflammation and discharge of some degenerative peptides such as substance P and nitric oxide. Theses degenerative neuropeptides can move in an antegrade manner along the nerve to the spinal cord and then retrogradely back to the joint and have degenerative effects. Neurofascial prolotherapy affects through the restoration of function in these small sensory nerves (14).
2. Objectives
Considering the need to find nonsurgical, safe, simple, and inexpensive treatments for patients with knee osteoarthritis as well as gap of information about the efficacy of prolotherapy-especially neurofacial method- this study was designed to evaluate the effects of intraarticular along with neurofascial prolotherapy and to compare its effects with corticosteroid injection, on pain and function of patients with knee OA.
3. Methods
This study was performed on patients suffering from knee OA as a double-blind randomized clinical trial. A total of 50 patients with knee OA were randomly assigned into two groups by generating random numbers with MATLAB 2014b software, where odd and even numbers were attributed to corticosteroid injection and dextrose injection, respectively. The sample size in each group was estimated to be 50.
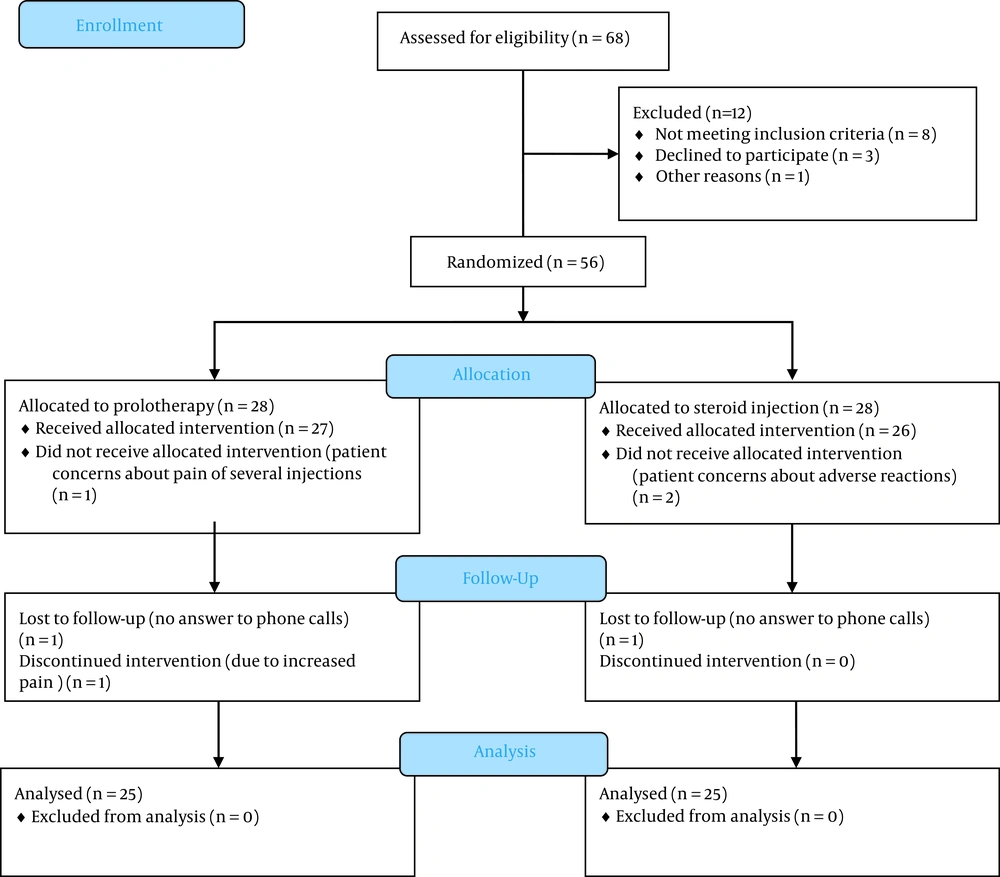
Subjects were chosen from patients referred to physical medicine and rehabilitation clinic of Mahdieh Hospital affiliated with Shahid Beheshti University of Medical Sciences from October 2018 to January 2019. The flow diagram of the study is presented in Figure 1.
The proposal of this study was investigated in the ethics committee for which ethics code was received. This study has also been registered in the Iranian clinical trials center with the code of IRCT20170311033000N4 and informed Consent was obtained from patients.
The study was approved by the ethics committee of IR.SBMU.MSP.REC.1397.555 and written informed consent was obtained from participants.
The patients were assessed at baseline, one and three months after the procedure by a trained assessor (unaware of the injection process) using Visual Analog Scale of pain (VAS) and a validated Persian translation of Western Ontario and McMaster Universities Arthritis (WOMAC) questionnaire.
Western Ontario and McMaster Universities Arthritis questionnaire includes 5 questions about pain, two questions on joint stiffness and 17 about functional limitations. Each item is scored on a scale of 0 to 4 and the total score ranges from 0 to 96. Validity and reliability of the Farsi translation of WOMAC questionnaire were evaluated and confirmed by Bina et al. in 2015 (15).
3.1. Inclusion Criteria
Knee OA patients age between 45 - 75 years with radiologic grading of 2 and 3 according to Kellgren Lawrence (KL) criteria who had no response to treatments over the past three months.
3.2. Exclusion Criteria
History of any intra-articular injection, knee physiotherapy or knee surgery over the past three months, systemic diseases (rheumatoid arthritis), BMI over 35 and allergy or hypersensitivity to the studied drugs.
According to exclusion criteria 6 patients were excluded, 4 because of obesity (BMI over than 35), 1 had arthritis rheumatoid (RA) and 1 had triamcinolone injection last week and finally, data of 50 patients were analyzed. The first group (25 patients) underwent treatment with one session of dextrose prolotherapy as one intra-articular injection in the form of a combination of 8 cc dextrose 20% + 2 cc lidocaine 1% and periarticular intradermal injections of dextrose 12% at four points around the knee (two points above the patella in the medial and lateral parts, one pint in the knee medial joint line and one point in the lateral part of the knee anterior to the head of fibula) with injection of 2.5 cc at each point (a combination of 3 cc dextrose 20% and 2 cc lidocaine 1% in a 5 cc syringe, where only 2.5 cc of it would be injected). Figure 2 shows the points of intradermal injection.
The above- mentioned areas are approximate points of fascial penetration of sensory nerves to enter the subcutaneous tissue (14). To make sure that the nerve has been effectively injected, the injections were accomplished in a circular pattern around the needle entrance site with about 5 points of infiltration of 0.5 cc of solution. The second group (25 patients) received one session of intra- articular injection of triamcinolone (40 mg) with 1 cc of lidocaine 1%. Injections were performed using G22 needle under sterilized conditions. For joint injection lateral mid-patellar approach with knee in the extension was chosen. Exercise therapy including isometric strengthening of quadriceps femoris, thigh adductors and abductors plus stretching of hamstring muscles was prescribed for both groups.
3.3. Data Analysis
For data analysis, STATA 14 software was used. Continuous demographic variables were described by mean and standard deviation, while qualitative variables were described as number and percentage. Repeated measures analysis of variance was employed for analyzing longitudinal data. The repeated measures ANOVA has two major parts of intragroup and intergroup changes; in this study both sources of changes were considered. For the qualitative variables, Chi-do Pearson analysis was used. The significance level in this study was considered below 0.05.
4. Results
50 patients with Knee OA were studied in this double blinded randomized clinical trial. In total, 33 men (66%) and 17 women (33%) were present in this study. There were 18 men (72%) and 7 women (28%) in the prolotherapy group, 15 men (60%) and 10 women (40%) in the corticosteroid group. that these differences were not statistically significant (P-Value = 0.370) (Table 1).
| Demographic Variables | Prolotherapy Group (n = 25) | Corticosteroid Group (n = 25) | P-Value |
|---|---|---|---|
| Age | 56.24 ± 6.11 | 57.08 ± 6.80 | 0.096 |
| Sex | 0.370 | ||
| Male | 18 (72) | 15 (60) | |
| Female | 7 (28) | 10 (40) | |
| BMI | 27.3 ± 2.97 | 27.33 ± 1.95 | 0.396 |
| Duration of pain | 4.28 ± 2.45 | 5.78 ± 1.36 | 0.194 |
| Stage | 0.777 | ||
| 2 | 13 (52) | 14 (56) | |
| 3 | 12 (48) | 11 (44) | |
| Turn | 0.370 | ||
| Left | 18 (72) | 15 (60) | |
| Right | 7 (30) | 10 (40) | |
| History of physiotherapy | 0.156 | ||
| Yes | 14 (56) | 9 (36) | |
| No | 11 (44) | 16 (64) |
a Values are expressed as No. (%) or mean ± SD.
The average age of the patients in the study is 56.67 years, which is 56.24 years in the prolotherapy group and 57.07 years in the corticosteroid group, which is not statistically significant (P-value = 0.096) (Table 1).
Table 2 presents before treatment values of study outcomes. No significant difference was found before treatment.
| Variables | PRT (n = 25) | CS (n = 25) | P-Value |
|---|---|---|---|
| VAS | 7.72 ± 1.06 | 7.92 ± 1.07 | 0.511 |
| WOMAC | |||
| Pain | 9.76 ± 1.39 | 9.24 ± 1.64 | 0.11 |
| Function | 30.28 ± 5.27 | 30.2 ± 5.2 | 0.95 |
| Stiffness | 2.96 ± 0.78 | 2.64 ± 1.15 | 0.25 |
| Total | 43.0 ± 6.33 | 41.8 ± 7.85 | 0.55 |
Abbreviations: PT, prolotherapy; CS, corticosteroid; VAS, Visual Analogue Scale; WOMAC, The Western Ontario and McMaster Universities Osteoarthritis Index.
Table 3 shows the changes in VAS pain scale. In one and three months postintervention, both prolotherapy and corticosteroid group showed significant improvement in pain (P < 0.001).
| Time | Test of Within-Group Effects (Mean Change from Baseline) | Test of Between-Group Effects (Mean Change from Group) | |||||
|---|---|---|---|---|---|---|---|
| PT | P-Value | CS | P-Value | MD | 95% CI | P-Value a | |
| T1 | -5.2 (-5.7, -4.7) | < 0.001 | -6.23 (-6.4, -5.5) | < 0.001 | 1.03 | (0.39 ,1.67) | 0.002 |
| T3 | -4.6 (-5.1, -4.1) | < 0.001 | -1.69 (-2.9, -1.3) | < 0.001 | -1.58 | (-2.2, -0.94) | 0.001 |
| F (%) b | 59.5 | 21.33 | |||||
Abbreviations: MD, mean difference; 95% CI, 95% confidence interval; PT, prolotherapy; CS, corticosteroid; T1, 1 month after intervention; T3, 3 months after intervention.
aAdjusted generalized estimating equations model after controlling the baseline outcome, sex, age, BMI.
b (Baseline - 3th month)/baseline) × 100.
Comparing prolotherapy and corticosteroid groups, the mean pain reduction based on VAS scale within the first month was significantly different in favor of steroid (P = 0.002). In other words, one month after treatment, corticosteroid group experienced greater improvement compared to prolotherapy group. Within three months post treatment, this difference was statistically significant in favor of prolotherapy (P = 0.001). In other words, the prolotherapy group experienced greater improvement. Table 4 lists changes in WOMAC scale.
Based on WOMAC pain subscale, at one and three months follow up, in both prolotherapy and steroid group significant decrease in pain was observed (P < 0.001) (Table 4).
| Variables | Test of Within-Group Effects (Mean Change from Baseline) | Test of Between-Group Effects (Mean Change from Group) | |||||
|---|---|---|---|---|---|---|---|
| PRT | P-Value | CS | P-Value | MD | 95% CI | P-Value a | |
| Pain | |||||||
| T1 | -5.08(-5.7, -4.4) | < 0.001 | -6.0(-6.6, -5.4) | < 0.001 | 0.92 | (0.06, 1.7) | 0.048 |
| T3 | -4.92(-6.1, -4.2) | < 0.001 | -1.96(-2.5, -1.3) | < 0.001 | -2.95 | (-3.6, -2.0) | < 0.001 |
| F (%) b | 49.8 | 23.30 | |||||
| Stiffness | |||||||
| T1 | -1.68(-2.0, -1.3) | < 0.001 | -1.53(-1.8, -1.2) | < 0.001 | -0.14 | (-0.6, 0.3) | 0.560 |
| T3 | -1.16(-1.5, -0.8) | < 0.001 | -0.38 (-0.7, -0.9) | 0.016 | -0.77 | (-1.2, -0.3) | 0.001 |
| F (%) b | 40.0 | 36.4 | |||||
| Fun | |||||||
| T1 | -12.3(-14.5, -10.1) | < 0.001 | -14.07(-15, -12,5) | < 0.001 | 1.75 | (1.04, 4.56) | 0.219 |
| T3 | -11.76(-13.9, -9.5) | < 0.001 | -5.84(-7.2, -4.5) | < 0.001 | -6.91 | (-6.5, -2.2) | < 0.001 |
| F (%) b | 38.5 | 19.2 | |||||
| Total | |||||||
| T1 | -19.08(-22.0, -16.1) | < 0.001 | -22.1(-26.2, -22.7) | < 0.001 | 2.02 | (-1.5, 5.6) | 0.262 |
| T3 | -17.84(-20.7, -14.9) | < 0.001 | -8.1(39.2,45.0) | < 0.001 | -9.64 | (-12.0, -6.2) | < 0.001 |
| F (%) b | 41.3 | 19.9 | |||||
Abbreviations: PRT, prolotherapy; CS, corticosteroid; Fun, functional limitation, MD, mean difference; 95% CI, 95% confidence interval; T1, 1 month after intervention; T3, 3 months after intervention.
aAdjusted generalized estimating equations model after controlling the baseline outcome, sex, age, BMI.
b [(Baseline - 3th month)/baseline) × 100.
Comparing prolotherapy and corticosteroid groups, the mean pain decrease based on WOMAC scale was significantly different (P = 0.048) in first month. In other words, one month after treatment, corticosteroid group experienced greater improvement. Within three months, this difference was statistically significant (P < 0.001) in favor of prolotherapy. In other words, in three months follow up, prolotherapy group experienced greater pain reduction (Table 4).
In both prolotherapy and steroid group, joint stiffness score of WOMAC scale showed a significant improvement at one and three months after intervention (P < 0.001) (Table 4).
Comparing steroid and prolotherapy group; at one month follow up; the mean decrease of joint stiffness score, was not significantly different (P = 0.560). Within three months post treatment, this difference was statistically significant (P = 0.001). In other words, three months post intervention, prolotherapy group experienced greater improvement in joint stiffness (Table 4).
In both prolotherapy and steroid group, function score of WOMAC scale at one and three months post intervention showed significant improvement (P < 0.001) (Table 4).
Comparing two groups; within the first month, mean changes in function score of WOMAC scale was not significantly different (P = 0.219). In three months, post treatment, this difference was statistically significant (P = 0.001). In other words, prolotherapy group experienced greater functional improvement in three months post intervention (Table 4).
In both prolotherapy and steroid group, the mean difference of total WOMAC score at one and three months follow up showed significant improvement (P < 0.001) (Table 4).
The mean changes of total WOMAC score among the prolotherapy and corticosteroid groups within the first month was not significantly different (P = 0.262). In three months, post treatment, this difference was statistically significant (P < 0.001). In other words, prolotherapy group experienced greater improvement in total WOMAC, compared to corticosteroid group (Table 4).
5. Discussion
This study dealt with investigating the effect of dextrose prolotherapy as a combination of intraarticular and extraarticular intradermal injection- on pain and function of patients with knee OA. We also compared the results with intra-articular injection of triamcinolone.
Based on the findings, both interventions caused significant improvement in patients’ pain and function within the short run (one month) and in the midterm (three months). Comparing two interventions, in short term follow up, the results regarding pain favored intra-articular injection of corticosteroid; at one month postintervention, the observed pain reduction (assessed by VAS and pain component of WOMAC questionnaire) was significantly better in steroid group. No significant difference was observed between the two groups at this time regarding the total score of WOMAC as well as its function or stiffness components. In third month postintervention, the results favored prolotherapy. According to the findings, in midterm follow up, therapeutic effects of prolotherapy were more persistent and superior over corticosteroid. Considering the mechanism of action of these two compounds, the findings were expectable. Steroids have temporary anti-inflammatory effects that appear quickly and go away after a while (usually some months), but prolotherapy causes tissue repair by inducing inflammation, so the effects appear later (within a week or two) but they are more stable and sometimes last for months. On the other hand, the main pathogenesis in osteoarthritis is not inflammatory but destruction of joint tissues, and therefore therapies which focus on repair have better effects on it.
In current study, in addition to intra-articular dextrose injection, neurofacial (perineural) injections were also applied. There is a hypothesis that nerve friction at the site of skin penetration, may cause chronic construction injury (CCI) and subsequently cause neuropathic pain. Perineural subcutaneous injection (PSI) of dextrose at low concentrations at the CCI site, the point of dermal penetration of nerves to enter the subcutaneous tissue, has analgesic effects on neuropathic pain, therefore the muscles can regain their normal function (16). According to this hypothesis, it can be stated that use of perineural dextrose injection along with intra-articular application (the method used in current study), can play a complementary role and increase the therapeutic effects. Looking at literature, in the only study that compared a combination of extra and intraarticular injections with intra-articular prolotherapy, better results were observed with the combined technique (17). Regarding this reinforcement effect and also to eliminate the confounding factor of number of injections (especially limitations in number of intra-articular steroid injections), in current study, a single session of combined technique was applied. The results were compared with a single intra- articular injection of corticosteroid. Considering the concerns for complications of intradermal steroid injection (skin atrophy and depigmentation), in control group just extra-articular injection of triamcinolone was not applied.
Rezasoltani et al. (18) in 2017 compared the effects of extra-articular and intra-articular dextrose prolotherapy in reducing pain and improving function of patients with knee osteoarthritis. In periarticular group, injections were performed subcutaneously at 4 points around the knee at the exit of nerves from knee capsule. Based on the findings of this study, periarticular prolotherapy has effects comparable and even superior to intra-articular injection of dextrose. Findings of their trial are a confirm to the current study´s. Difference point is the number of injections. In most prolotherapy techniques repeated injections are recommended. Rezasoltani et al., also applied three weekly injections. As explained above, the authors of current study decided to do just one session of injection and by combining the extra and intraarticular technique compensate for this. In a study by Soliman et al. in 2016 (17), intraarticular dextrose injection was compared to a combination of intra and extraarticular myofascial dextrose prolotherapy technique used by Lyftogt (19). Myofacial injection was performed at the insertion site of ligaments and tendons. In both subgroups, injections were repeated in first, second and third months. In both groups, there was a significant improvement in VAS and WOMAC in both long and short term. In short term, the improvement was significantly better in group of combination therapy. In long-term follow up (12 months), sonographic examination showed a significant decrease in ligament and tendon thickness and a significant increase in cartilage thickness. Radiological findings of the patients improved significantly only in combination therapy group. This study showed that prolotherapy leads to a lasting improvement in pain, function and radiographic characters of OA patients. Combination of two injection techniques resulted in a better and faster response. In our study, although only one injection was used, the combination technique resulted in a better response both in short and medium term.
In another study by authors of current study performed with a similar technique on patients with moderate and severe knee osteoarthritis, similar results were obtained. This finding suggests that prolotherapy can have good effects even in patients with severe osteoarthritis (20). Singh et al. (21) in 2019 compared the effect of intra-articular dextrose prolotherapy and corticosteroid in patients with knee osteoarthritis. For all patients, injections were performed monthly up to three months (three injections). This study generally concluded that intra-articular injection of corticosteroid is preferred over prolotherapy. These were in contrast to the findings of our study. In our trial, in short-term assessment, corticosteroid offered better analgesic effects compared to prolotherapy. However, in three months assessment, prolotherapy was more effective both on pain and function of patients. This difference can be attributed to different prolotherapy techniques used in two trials (intra-articular compared to intra-articular and perineural) as well as the lower volume of dextrose injected in Singh’s study (5 mL compared to 8 ml in ours). Also, the method of this study is against the most of similar trials. In this study, three consecutive intra- articular corticosteroid injections were used with one month intervals, which is in contrast to the recommended limitations on use of intra-articular steroids; considering the complications of repeated steroid injections, recommendation has been given to limit this intervention to at most three injections per year (11, 22).
Rabago et al. (23) in 2011 conducted a study with two arms (prolotherapy and control). Patients in prolotherapy group, received a combination of both intra-articular and extraarticular neurofascial injections. The patients received five injections per month. The control group underwent saline injection as well as exercise training. They also evaluated the cartilage volume which showed improvement. Based on these findings, it can be stated that prolotherapy resulted in safe and considerable improvement in pain and quality of life of these patients over 52 weeks. By influencing the volume of cartilage, prolotherapy can have a corrective effect on the course and symptoms of osteoarthritis.
Based on the findings of present study and similar research, it seems that a combination of injections (intra and extra-articular) could be an effective treatment for patients with knee arthritis. In addition to pain reduction, it can also improve the mechanical stability of knee as well as the cartilage damage (24).
5.1. Limitations
The main limitations of this study were low number of cases and short-term follow-up for only 3 months. Another point is that both outcome measure tools (VAS and WOMAC) are subjective. Application of an objective method could significantly improve the strength of findings. Also, considering the need to several needle insertions for periarticular prolotherapy, the experienced level of pain is a bit more than routine injection methods and can lead to lower patient compliance.
The strength of study is application of combined method of prolotherapy and decreasing the session of injections.
5.2. Conclusions
Based on the findings of the present study, combined method of intra-articular and neurofascial dextrose prolotherapy leads to improved pain and function in patients with knee osteoarthritis both in the short and midterm. Although prolotherapy was shown to be less effective within the short term, its effects were more persistent and in midterm investigations (three months) it caused better improvement compared to corticosteroid. Also, in future studies, it is suggested that a multi-arm clinical trial be developed and different prolotherapy methods for knee osteoarthritis sufferers be investigated together (combined prolotherapy, neurofacial prolotherapy, intra-articular prolotherapy). Also, in future studies, the effect of increasing the number of prolotherapy injections (one time compared to several times) and the effect of different concentrations of dextrose on the control of patients' symptoms can be investigated.