1. Context
Cesarean section is one of the most common surgeries in obstetrics, the rate of which is increasing significantly worldwide (1-4). The rate of cesarean section has been reported at 42.35% in the world and 47.9% in Iran (5, 6). The correct management of delivery and choosing the appropriate anesthetic method to achieve analgesia and maintain the health of the mother and fetus during cesarean section are of great importance (7). The type of anesthesia used in cesarean section should cause the fewest complications for both mother and baby. For cesarean section patients, spinal anesthesia is a reliable and safer procedure than general anesthesia (8). Spinal anesthesia is often used in emergency and elective cesarean section due to the reduction of anesthesia-related mortality, rapid onset, and complete muscle relaxation (9-12). Less neonatal complications, lower prevalence of failed block, and reduction of pneumonia due to aspiration are among the advantages of spinal anesthesia (10). Bupivacaine is a long-acting amide anesthetic mainly used for spinal anesthesia (13). Ropivacaine is a long-acting amide anesthetic that is structurally very similar to bupivacaine. This drug creates an effective epidural anesthesia for cesarean delivery and is also used in spinal anesthesia (14). The ideal drug for spinal anesthesia should have fewer hemodynamic disorders, appropriate duration of anesthesia, quick return of sensation/movement, and fewer side effects (7). Since various studies have reported different side effects of the intrathecal hyperbaric bupivacaine and hyperbaric ropivacaine in cesarean section, this systematic review and meta-analysis aimed to evaluate maternal and newborn outcomes after spinal anesthesia with intrathecal hyperbaric bupivacaine and hyperbaric ropivacaine.
2. Evidence Acquisition
This meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The statistical population of this study included all women candidates for elective cesarean section under spinal anesthesia who received intrathecal bupivacaine or ropivacaine. This study was approved by the Ethics Committee of Ilam University of Medical Sciences (code: IR.MEDILAM.REC.1401.223; grant number: A-10-2341-34).
2.1. Search Strategy and Eligibility Criteria
With no language restrictions, the researchers began searching for clinical trial studies using a systematic search from 1 September 2022 to 1 November 2022. Other studies (such as case reports, abstracts, and review studies) were excluded from the search.
In this systematic search, studies between the years 1995 to 2022 were investigated using the following keywords: Intrathecal bupivacaine or ropivacaine, hypotension, nausea, vomiting, shivering, onset of sensory and motor block, Apgar score, cesarean section, spinal anesthesia, and regional anesthesia. Web of Science, Embase, PubMed, Scopus, Google Scholar, MagIran, and IranDoc databases were searched from 1 September 2022 to 1 November 2022.
Inclusion criteria were the use of intrathecal hyperbaric bupivacaine and hyperbaric ropivacaine, elective cesarean section under spinal anesthesia, onset of sensory and motor block, and assessment of hypotension, bradycardia, nausea, vomiting, shivering, and Apgar score. Exclusion criteria were emergency cesarean section, the use of local anesthesia, studies unrelated to the topic, and studies whose full text was not available.
2.2. Data Extraction
Two researchers simultaneously conducted study selection and data extraction and checked the quality of the studies. The following information was extracted from all studies: Author’s name, country, year of publication, sample size, incidence of hypotension, bradycardia, nausea, vomiting, shivering, Apgar score at 1 and 5 minutes, and onset of sensory and motor block.
2.3. Statistical Analysis
Since the included studies were clinical trials, the effect size consisted of relative risk (RR) and Hedges G (standardized mean difference (SMD)). A fixed-effects model was used for parameters where the I2 index was less than 25%, and a random-effects model was used for parameters above 50%. The Egger test and funnel plot were used to check publication bias. Data were analyzed using Stata version 17 (StataCorp LLC, College Station, Texas, USA). The significance of the year in the studies was carried out using the meta-regression method. P values less than 0.05 were considered statistically significant.
3. Results
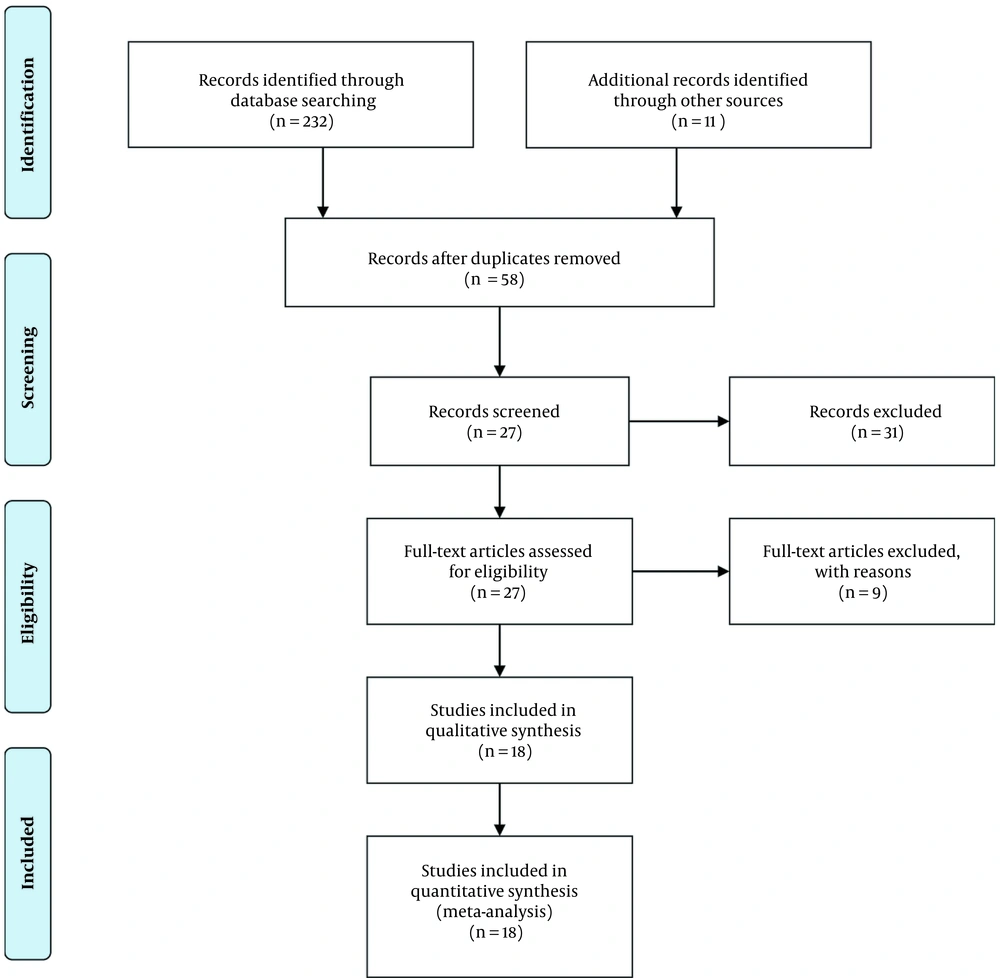
Selection of articles: 73, 65, and 116 articles were taken from Web of Science, PubMed and Scopus respectively. After removing duplicates, 58 articles remained. After reviewing the summary of the articles, 31 articles unrelated to the topic were removed. By checking the full text of the articles, due to the use of anesthetic drugs in combination with other drugs, 6 articles were removed, and 2 articles were excluded due to the lack of sample size. Finally, 18 articles with 1542 subjects (6-8, 11, 15-28) were included in the analysis (Figure 1).
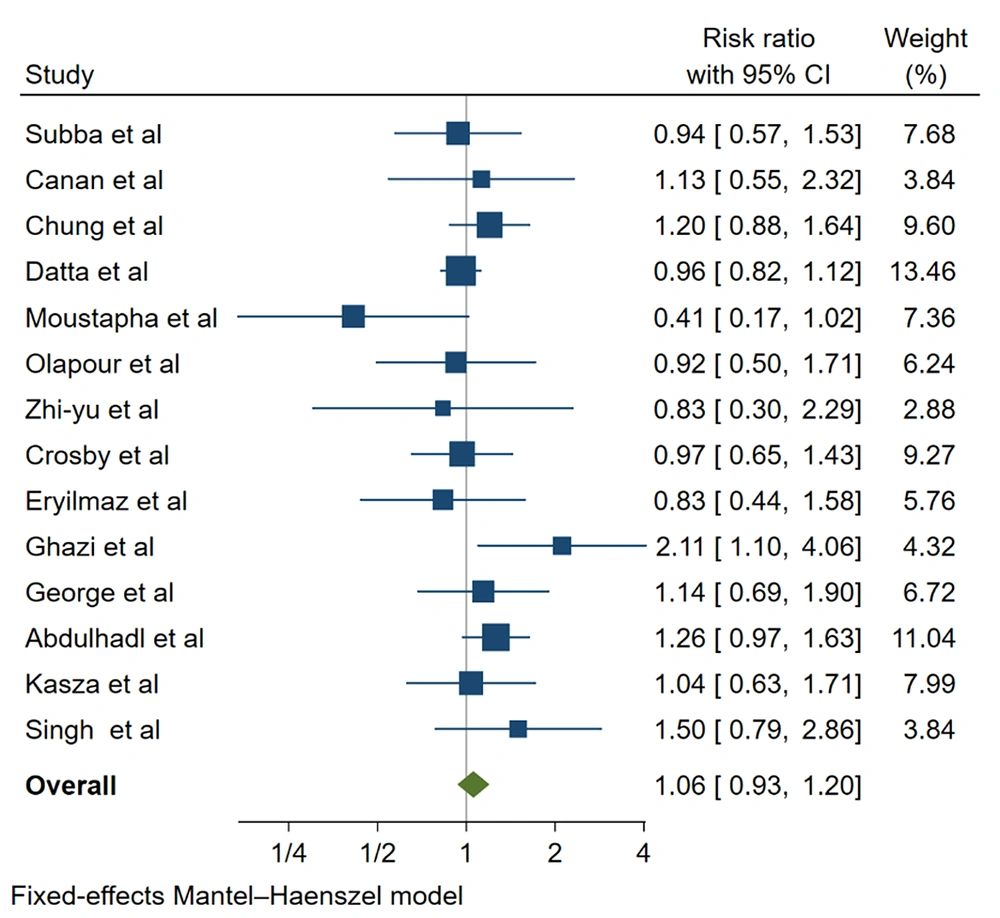
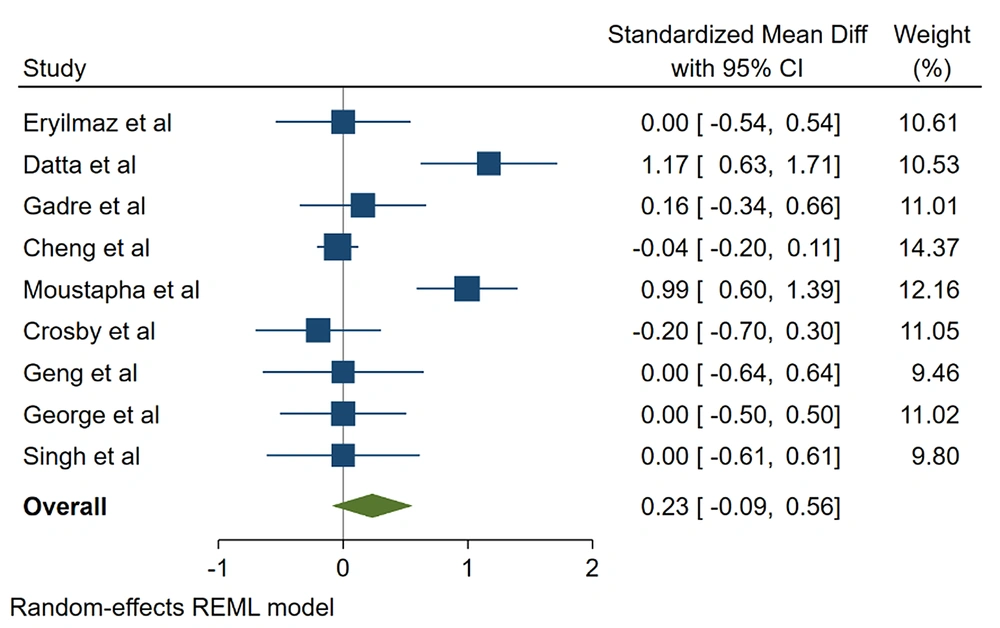
The results indicated that the 2 groups had no statistically significant differences in hypotension (RR, 1.57; 95% CI, 0.932 - 1.198; P = 0.3), bradycardia (RR, 0.785; 95% CI, 0.414 - 1.490; P = 0.4), and Apgar score of 1 (SMD, 0.233; 95% CI, -0.093 to 0.559; P = 0.16) and 5 minutes (SMD, 0.154; 95% CI, -0.135 to 0.443; P = 0.295; Figures 2 and 3, Tables 1 - 4).
| ID | Author | Year | Country | No./B | Mean/B/OM | SD/B/OM | No./R | Mean/R/OM | SD/R/OM | Mean/B/OS | SD/B/OS | Mean/R/OS | SD/R/OS | Mean/B/AS at 1 Min | SD/B/AS at 1 Min | Mean/R/AS at 1 Min | SD/R/AS at 1 Min | Mean B/AS at 5 Min | SD/B/AS at 5 Min | Mean/R/AS at 5 Min | SD/R/AS at 5 Min |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Bhattarai et al. (15) | 2019 | Nepal | 30 | 7.53 | 1.72 | 30 | 14.33 | 6.19 | 4.87 | 1.46 | 4.87 | 1.82 | ||||||||
| 2 | Günaydin and Eryilmaz (28) | 2011 | Turkey | 26 | 8.1 | 4.1 | 26 | 11.6 | 5.6 | 9 | 0.1 | 9 | 0.1 | 10 | 0.5 | 10 | 0.5 | ||||
| 3 | Canan et al. (8) | 2013 | Turkey | 20 | 20 | 8.1 | 0.8 | 8.4 | 0.5 | 9.8 | 0.3 | 9.7 | 0.4 | ||||||||
| 4 | Chung et al. (16) | 2001 | Korea | 30 | 6 | 1.9 | 30 | 6.3 | 2.2 | 2.5 | 1 | 3.2 | 1.2 | ||||||||
| 5 | Datta et al. (19) | 1995 | USA | 29 | 8.9 | 1.14 | 31 | 10.3 | 0.8 | 2.8 | 1.1 | 2.7 | 1.2 | 7.4 | 0.3 | 7.1 | 0.2 | 9 | 0.1 | 9 | 0.1 |
| 6 | Gadre et al. (11) | 2019 | India | 30 | 4.8 | 0.8 | 30 | 5.4 | 0.6 | 4.2 | 0.08 | 4.3 | 0.8 | 8.13 | 0.5 | 8.05 | 0.5 | 9.1 | 0.3 | 9.1 | 0.1 |
| 7 | Cheng et al. (6) | 2019 | China | 297 | 6.94 | 0.1 | 318 | 3.84 | 0.5 | 9.78 | 0.5 | 9.8 | 0.4 | 9.7 | 0.2 | 9.1 | 0.8 | ||||
| 8 | Diouf et al. (20) | 2020 | Senegal | 42 | 73 | 8 | 0.5 | 7.5 | 0.5 | 9.5 | 0.5 | 9.5 | 0.5 | ||||||||
| 9 | Olapour et al. (17) | 2020 | Iran | 33 | 1.63 | 0.3 | 33 | 2.86 | 0.8 | 1.28 | 0.4 | 2.32 | 0.9 | ||||||||
| 10 | Crosby et al. (23) | 1998 | Canada | 31 | 30 | 7 | 0.05 | 7.1 | 0.7 | 9 | 0.7 | 9 | 0.1 | ||||||||
| 11 | Geng et al. (21) | 2014 | China | 18 | 18 | 9 | 1 | 9 | 0.5 | 10 | 0.5 | 10 | 0.3 | ||||||||
| 12 | Ghazi et al. (7) | 2021 | Iran | 38 | 38 | 3.63 | 1.34 | 8 | 3 | ||||||||||||
| 13 | George et al. (25) | 2022 | India | 30 | 5.6 | 1.6 | 30 | 6.45 | 1.8 | 2.31 | 0.6 | 2.6 | 0.8 | 8 | 1 | 8 | 1 | 10 | 0.5 | 10 | 0.3 |
| 14 | Al-Abdulhadi et al. (26) | 2007 | Saudi Arabia | 33 | 6.4 | 0.3 | 33 | 6.6 | 0.6 | 4.81 | 2.17 | 4.79 | 1.95 | ||||||||
| 15 | Kasza et al. (27) | 2009 | Poland | 39 | 11.2 | 22.6 | 36 | 10.4 | 2.2 | 6.4 | 1.4 | 6.1 | 1.1 | ||||||||
| 16 | Singh et al. (18) | 2019 | India | 20 | 20 | 8 | 1 | 8 | 0.7 | 10 | 0.3 | 10 | 0.1 |
Characteristics of the Studies According to Mean ± SD
| ID | Author | Year | Country | No./B | No.+/B/HY | No./R | No.+/R/HY | No.+/B/BR | No.+/R/BR | No.+/B/SH | No.+/R//SH | No.+/B/VO | n+/R/VO | n+/B/NU | n+/R/NU |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Bhattarai et al. (15) | 2019 | Nepal | 30 | 15 | 30 | 16 | 1 | 1 | 3 | 1 | 0 | 1 | 0 | 1 |
| 2 | Canan et al. (8) | 2013 | Turkey | 20 | 9 | 20 | 8 | 2 | 3 | 3 | 2 | 10 | 8 | 13 | 12 |
| 3 | Chung et al. (16) | 2001 | Korea | 30 | 24 | 30 | 20 | 1 | 3 | 5 | 3 | 5 | 2 | 8 | 4 |
| 4 | Datta et al. (19) | 1995 | USA | 29 | 26 | 31 | 29 | ||||||||
| 5 | Diouf et al. (20) | 2020 | Senegal | 42 | 5 | 73 | 21 | 1 | 2 | ||||||
| 6 | Olapour et al. (17) | 2020 | Iran | 33 | 12 | 33 | 13 | 1 | 3 | ||||||
| 7 | Geng et al. (21) | 2011 | China | 20 | 5 | 20 | 6 | 3 | 3 | 3 | 3 | ||||
| 8 | Feng et al. (22) | 2021 | China | 42 | 44 | 28 | 9 | ||||||||
| 9 | Crosby et al. (23) | 1998 | Canada | 31 | 19 | 30 | 19 | 1 | 1 | 1 | 2 | 3 | 1 | 10 | 5 |
| 10 | Günaydin and Eryilmaz (28) | 2011 | Turkey | 26 | 10 | 26 | 12 | 1 | 2 | 4 | 1 | 3 | 3 | 6 | 6 |
| 11 | Ghazi et al. (7) | 2021 | Iran | 38 | 19 | 38 | 9 | 3 | 2 | 11 | 7 | 15 | 4 | 19 | 6 |
| 12 | George et al. (25) | 2022 | India | 30 | 16 | 30 | 14 | 1 | 0 | 2 | 5 | 6 | 8 | ||
| 13 | Al-Abdulhadi et al. (26) | 2007 | Saudi Arabia | 33 | 29 | 33 | 23 | 3 | 3 | 20 | 11 | ||||
| 14 | Kasza et al. (27) | 2009 | Poland | 39 | 18 | 36 | 16 | 1 | 1 | 4 | 1 | 5 | 2 | ||
| 15 | Singh et al. (18) | 2019 | India | 20 | 12 | 20 | 8 | 2 | 2 | 5 | 3 | 7 | 5 |
Characteristics of the Studies According to the Number of Parameters
| Parameters | Sample Size | Number of Study | I2% | RR (95% CI) | P Value |
|---|---|---|---|---|---|
| Hypotension | 891 | 14 | 13.81 | 1.057 (0.933,1.198) | 0.3 |
| Bradycardia | 705 | 11 | 0.00 | 0.785 (0.414,1.490) | 0.4 |
| Shivering | 435 | 7 | 0.00 | 2.24 (1.480,3.395) | 0.000 |
| Nausea | 630 | 11 | 4.25 | 1.526 (1.175,1.981) | 0.001 |
| Vomiting | 630 | 11 | 0.00 | 1.542 (1.048,2.268) | 0.02 |
Relative Risk and 95% CI in Variables: Hypotension, Bradycardia, Shivering, Nausea, and Vomiting
| Parameters | Sample Size | Number of Study | I2% | SMD (95% CI) | P Value |
|---|---|---|---|---|---|
| Apgar score at 1 min | 1155 | 9 | 80.38 | 0.233 (-0.093, 0.559) | 0.16 |
| Apgar score at 5 min | 1155 | 9 | 75.53 | 0.154 (-0.135, 0.443) | 0.295 |
| Onset sensory | 581 | 8 | 87.35 | -0.550 (-1.054, -0.045) | 0.032 |
| Onset motor | 1172 | 9 | 84.49 | -0.812 (-1.254, - 0.371) | 0.000 |
Standardized Mean Difference and 95% CI in Variables: Apgar Score at 1 and 5 Minutes, Onset Sensory Block, and Onset Motor Block
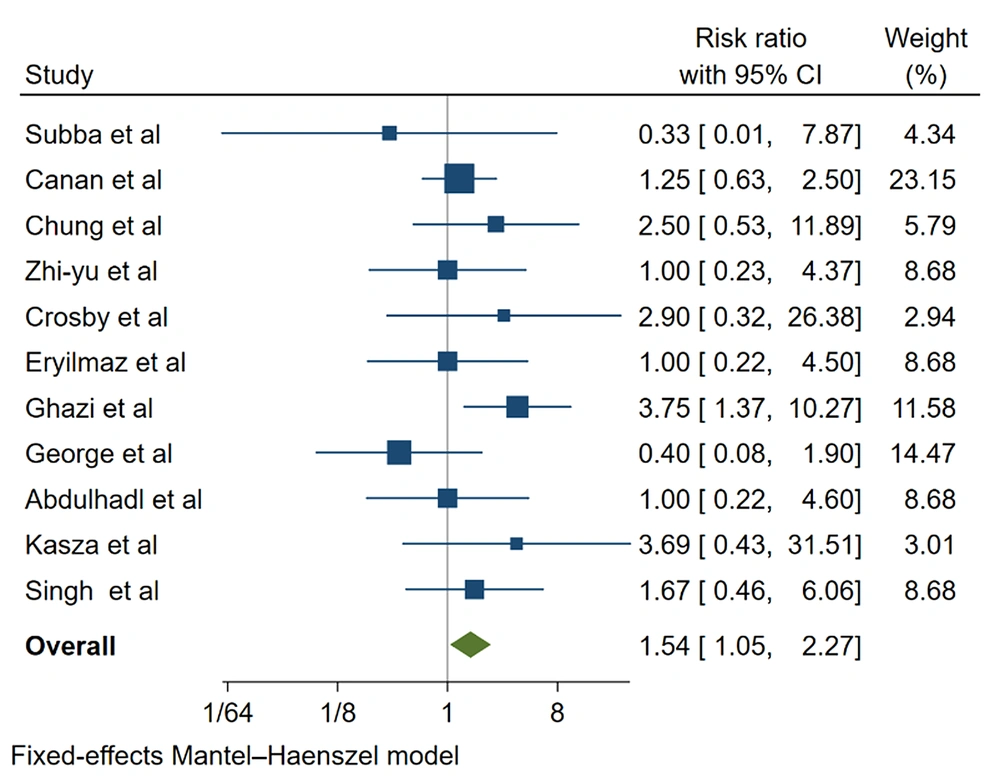
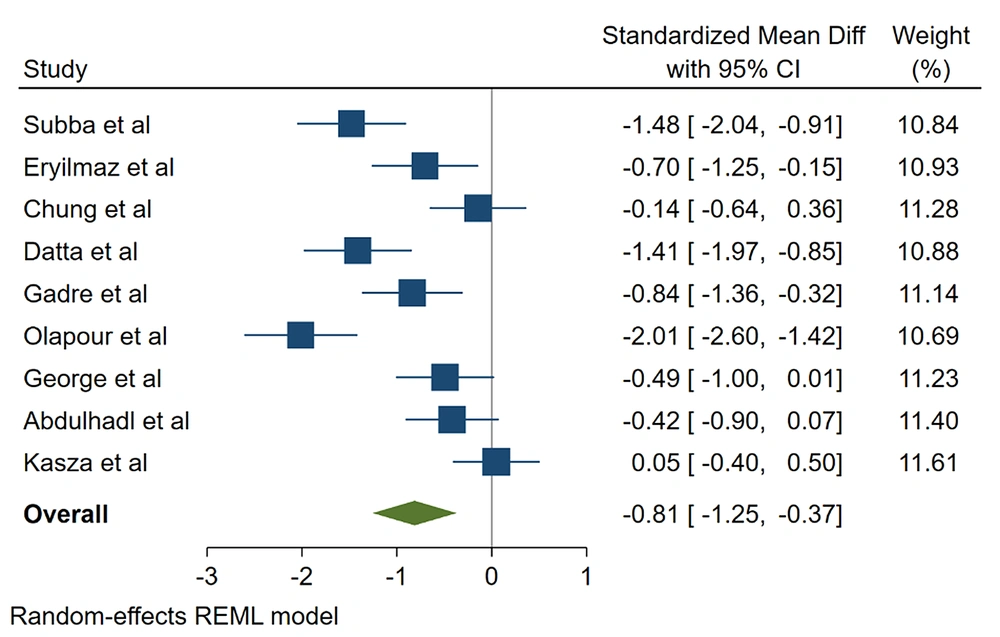
There was a statistically significant difference between the 2 groups in nausea (RR, 1.526; 95% CI, 1.175 - 1.981; P = 0.001), vomiting (RR, 1.542; 95% CI, 1.048 - 2.268; P = 0.02), shivering (RR, 2.24; 95% CI, 1.480 - 3.39; P = 0.00), onset of sensory block (SMD, -0.550; 95% CI, -1.054 to -0.045; P = 0.032), and onset of motor block (SMD, -0.812; 95% CI, -1.254 to -0.371; P = 0.000). The risk of nausea and vomiting caused by bupivacaine was 0.53% and 0.54% higher than the ropivacaine (Figures 4 and 5, Tables 1 - 4).
The incidence of shivering was 2.24 times higher in the bupivacaine group than in the ropivacaine group. The average onset time of sensory block (SMD, -0.550) and motor block (SMD, -0.812) was significantly lower in the bupivacaine group than in the ropivacaine group.
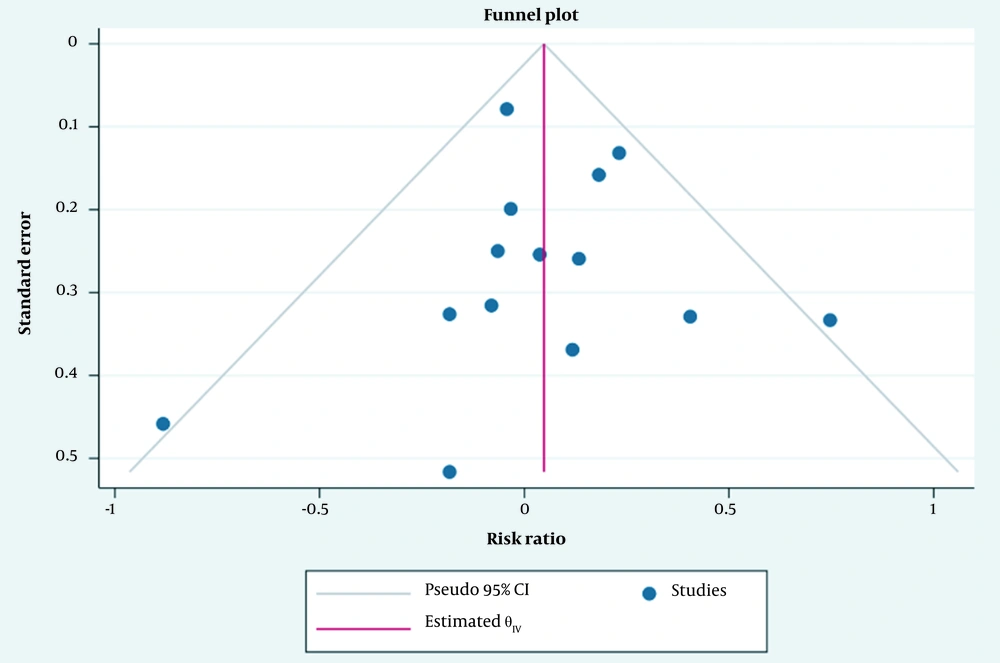
A meta-regression test was performed for all parameters, showing the non-significance of the year in the studies. On the other hand, the Egger test indicated no publication bias in the studies (Figure 6).
4. Discussion
In cesarean section, anesthesia can affect the mother and fetus (29). Anesthesia should not only provide adequate analgesia for the mother after cesarean section but also should have minimal effects on the relationship between the baby and the mother (30). The rapid onset of anesthesia, high success rate, fewer side effects, reduction of aspiration, and reduced mortality rate are among the advantages of spinal anesthesia in cesarean section (31-33). Our study showed that intrathecal bupivacaine vs. ropivacaine in cesarean section had no statistically significant difference in the incidence of hypotension, bradycardia, and Apgar score of newborns. Although the incidence of nausea, vomiting, and shivering was significantly higher in the bupivacaine group than in the ropivacaine group, the onset of sensory and motor block was faster in the bupivacaine group than in the ropivacaine group.
Bhattari et al. found that intrathecal bupivacaine vs. ropivacaine in cesarean section under spinal anesthesia had no statistically significant difference in the incidence of hypotension and bradycardia between the 2 groups (15). The incidence of nausea, vomiting, and shivering was significantly higher in the bupivacaine group than in the ropivacaine group. The onset of sensory block was faster in the bupivacaine group than in the ropivacaine group; however, the ropivacaine group had a shorter recovery (15). In another study, Ghazi et al. showed that blood pressure and the time to reach the appropriate level of anesthesia were significantly lower in the bupivacaine group than in the ropivacaine group (7). The time to decrease the level of anesthesia, the rate of nausea and vomiting, hypotension, and the use of ephedrine were significantly lower in the ropivacaine group than in the bupivacaine group (7).
In a similar study, Olapour et al. concluded that the duration of sensory and motor block was shorter in the ropivacaine group than in the bupivacaine group (17). There was no statistically significant difference in blood pressure between the 2 groups, but the heart rate was significantly higher in the bupivacaine group than in the ropivacaine group (17). Günaydin and Eryilmaz found that the onset of sensory and motor block was faster in the bupivacaine group than in the ropivacaine, and the duration of motor block was longer in the bupivacaine group than in the ropivacaine (28). No difference was observed in the hemodynamic changes of the 2 groups (28).
Canan et al. observed no statistically significant difference in hemodynamic changes, duration of anesthesia, Apgar score, pain, and onset of sensory and motor block between the 2 groups (8). The finding of Chung et al. and Singh et al. are consistent with the present study (16, 18). In the current study, the incidence of shivering, nausea, and vomiting was higher in the bupivacaine group than in the ropivacaine group, which is consistent with some previous studies (15, 16, 34, 35).
Cesarean section patients, especially those under spinal anesthesia, often complain of pain, nausea, vomiting, and shivering (36). Nausea is caused by the stimulation of chemoreceptors by opiates and hypotension (37). The shivering in cesarean section patients is caused by the acceleration of blood circulation, high metabolism in the late third trimester of pregnancy, and loss of heat during childbirth. The compensatory vasoconstriction in non-blocked areas caused by low blood pressure after anesthesia can increase the prevalence of shivering (1). Previous studies have indicated that in the management of shivering in cesarean section, ropivacaine is more suitable than bupivacaine (38), which is consistent with the present study. Both drugs had similar effects on the Apgar score of infants, which is consistent with some previous studies (9-11, 16, 39, 40). The onset time of sensory and motor block was less in the bupivacaine group than in the ropivacaine group.
Bupivacaine is a long-acting amide local anesthetic that causes cardiotoxicity. Since this side effect can cause problems for some pregnant women, ropivacaine has been developed to avoid it (11). Ropivacaine is a local anesthetic with a structure similar to bupivacaine. Ropivacaine has advantages such as separated sensory and motor block with fewer complications in the cardiovascular and central nervous systems, hemodynamic stability, less fat solubility, and faster recovery (41).
Since ropivacaine has a greater sensory block than bupivacaine, it leads to earlier motor activity and faster recovery (11). Although bupivacaine is more potent than ropivacaine for spinal anesthesia, it can be a good choice in shorter surgeries when rapid recovery is required. Fast recovery can bring more patient satisfaction (15). Gadre et al. found that ropivacaine had better clinical effects than bupivacaine in cesarean section patients, including shorter duration of motor and sensory block, high level of block, hemodynamic stability, and adequate analgesia after surgery (11).
Due to its low effects on the uterus, placenta, and hemodynamics of mothers, ropivacaine is suitable for anesthesia during cesarean section (6). Kathuria et al. reported that the use of ropivacaine in spinal anesthesia reduced complications in mothers and had better effects than traditional anesthetics (42). Several studies have suggested that in cesarean section, ropivacaine reduces motor block more significantly than bupivacaine (43). Fast recovery, early movement with fewer side effects, and safety of the fetus have made this drug desirable in cesarean section (11).
4.1. Conclusions
Although both ropivacaine and bupivacaine are effective in cesarean section, ropivacaine is more recommended due to fewer hemodynamic changes, shorter duration of sensory and motor block, fewer side effects, and faster recovery. These points can be important in patients with hemodynamic instability, such as pregnant women with heart diseases.
4.2. Limitations and Strengths
The small number of articles is one of the limitations of this study. Lack of bias in entering studies, the absence of language restrictions, and analysis of all parameters were the strengths of this study.