1. Background
Ultrasound has modernized regional anesthesia by its ability to construct cross-sectional images of the area of interest to assist in the placement of peripheral nerve blocks for postoperative pain relief. Two-dimensional (2D) imaging is the standard technique where nerves and local anesthetic injectates are visualized in one plane (i.e., transverse or longitudinal). A constraint of the 2D view is that multiple probe adjustments are necessary to maintain the needle trajectory toward the nerve target and to envision the distribution of the local anesthetic spread. This limitation can be addressed using three-dimensional (3D) ultrasound, which has traditionally been utilized as an optional imaging modality to the conventional 2D ultrasound-guided technique.
The utility of 3D imaging is primarily dependent on the type of ultrasound software and specialized probes. The use of 3D technology requires more computer processing power and expensive software features than 2D imaging, which are not typically available on standalone ultrasound machines (1). Recently, handheld ultrasound devices have become popular among clinicians due to their affordability and compatibility with tablets and smartphones. Their performance and image quality have demonstrated similar accuracy compared to cart-based ultrasound machines (2). Interestingly, several handheld ultrasound devices have the capability to construct 3D images using a traditional 2D ultrasound transducer. However, the literature description of handheld ultrasound 3D imaging of nerve blocks is limited.
2. Objectives
The current study aimed to construct 3D images of common peripheral nerve and fascial plane blocks using a handheld ultrasound device with a 2D ultrasound probe.
3. Methods
3.1. General Conditions
This study was performed under an exempt status granted by the Institutional Review Board of Rhode Island Hospital, the United States (IRB#1910048). The Institutional Review Board determined that the study qualified for exemption under 45 CFR 46.101(b). The 3D ultrasound imaging was part of the investigator’s routine evaluation.
3.2. Subject Population
A total of 10 patients who were scheduled to receive ultrasound-guided peripheral nerve blocks for outpatient surgery and classified as the American Society of Anesthesiologists physical status I or II with a body mass index of ≤ 30 kg/m2 were included in the study. Patients who presented with anatomical variations during the initial ultrasound scanning were excluded.
3.3. Nerve Block and Ultrasound Characteristics
Following the placement of standard monitors, the patients were premedicated with intravenous midazolam (2 - 5 mg) or fentanyl (25 - 50 mcg) as needed. All nerve blocks were performed by resident trainees prior to surgery in the preoperative holding area supervised by the primary investigator (V.R.). Before the placement of each nerve block with a local anesthetic, an ultrasound scan was performed to assess the anatomical structures using a portable handheld ultrasound transducer (Butterfly Network, Inc., Guilford, CT, USA) paired with a software-equipped tablet. This handheld ultrasound system includes several clinical built-in imaging options, including 3D reconstruction, without the need to switch transducers. Following the initial evaluation and localization of the target area, the position of the transducer was marked on the skin to record its location.
Each individual nerve block was performed using a conventional cart-based ultrasound system (Fujifilm SonoSite, Inc., Bothell, WA, USA). The block techniques and the dose of local anesthetic have been previously described in the literature (3-5). Immediately following block needle withdrawal, the portable handheld transducer was repositioned on the skin using the previously marked lines as a guide to obtaining the same transverse view of the target area and local anesthetic spread. After confirming the presence of no aberrant nearby fluid flow, the transducer in brightness mode was held steadily while a sweep of the local anesthetic spread was captured in a series of 2D images using the preset automatic volume calculation setting. After a few seconds (up to 10 seconds), the construction of the 3D image captured from the 2D images was complete.
4. Results
This study successfully constructed the 3D images of 10 peripheral nerve blocks. Table 1 shows patients’ demographic information, including the type of surgeries and the characteristics of the regional block performed. The median age of the study group was 44 years (interquartile range: 32 - 47 years). The average time to complete each 3D scan was less than 5 seconds per attempt, with fascial plane blocks requiring twice the amount of time to complete. The average time from needle withdrawal to portable handheld transducer placement was 3 minutes. All the nerve blocks provided effective postoperative analgesia without complications. The 3D images were successfully captured in all patients.
| Age (y) | Gender | Body Mass Index (kg/m2) | Type of Surgery | Side | Type of Block | Time to Obtain a Three-Dimensional Image (s) | Type of Injectate |
|---|---|---|---|---|---|---|---|
| 22 | Male | 28 | Clavicle open reduction internal fixation | R | Interscalene | < 5 | 30 mL 0.5% bupivacaine |
| 20 | Male | 26 | Elbow open reduction internal fixation | R | Supraclavicular | < 5 | 30 mL 0.5% bupivacaine |
| 46 | Female | 25 | Middle finger open reduction internal fixation | R | Infraclavicular | < 10 | 30 mL 0.5% bupivacaine |
| 45 | Female | 27 | Wrist open reduction internal fixation | L | Axillary | < 5 | 30 mL 0.5% bupivacaine |
| 52 | Female | 29 | Mastectomy | R | Pectoral nerve II | < 10 | 40 mL 0.25% ropivacaine |
| 47 | Male | 24 | Colostomy revision | R | Transversus abdominis plane | < 10 | 40 mL 0.25% ropivacaine |
| 32 | Male | 28 | Patella tendon reconstruction | R | Femoral | < 5 | 20 mL 0.5% bupivacaine |
| 58 | Male | 28 | Total knee arthroplasty | L | Adductor | < 5 | 20 mL 0.5% bupivacaine |
| 44 | Male | 27 | Leg flap reconstruction | L | Subgluteal sciatic | < 5 | 20 mL 0.5% bupivacaine |
| 34 | Male | 22 | Ankle open reduction internal fixation | R | Popliteal sciatic | < 5 | 30 mL 0.5% bupivacaine |
Patients’ Demographics and Regional Block Characteristics
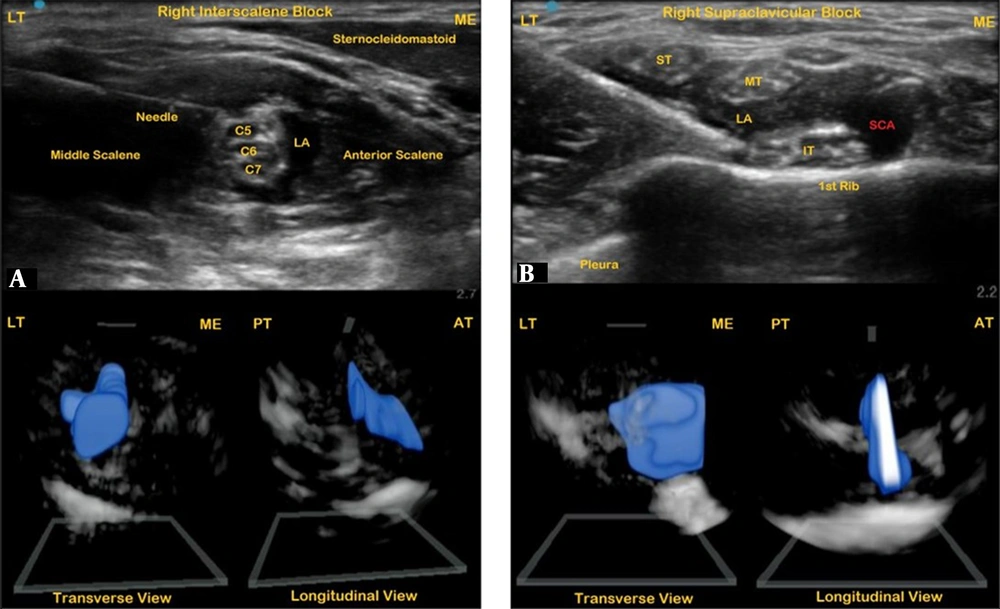
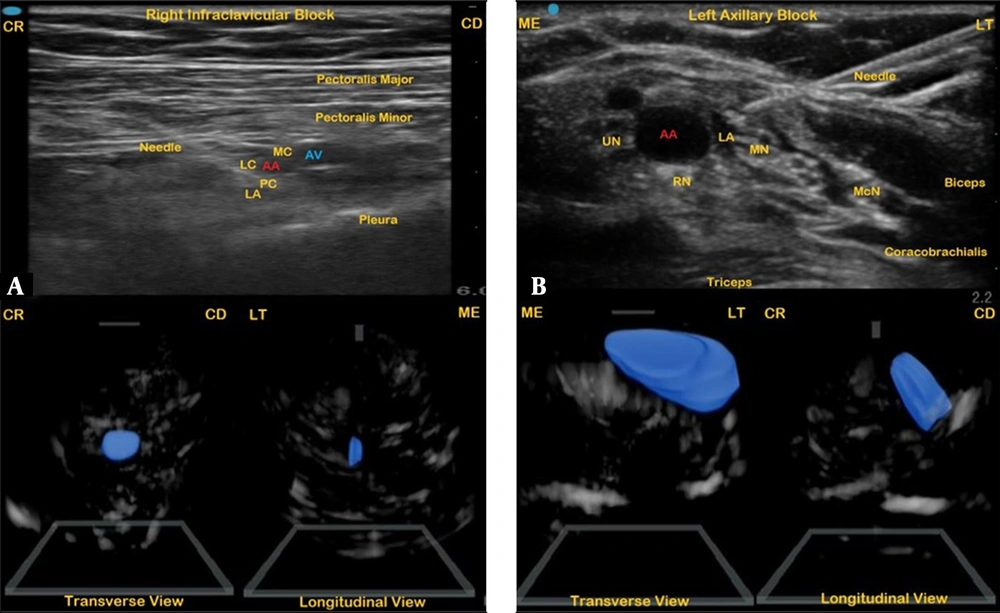
For each nerve block, the 2D ultrasound image and the reconstructed 3D image of the local anesthetic spread at the target site were visualized in both transverse and longitudinal views. The 3D image of the interscalene block revealed a circumferential spread of local anesthetic around the C5, C6, and C7 nerve roots that extended anteriorly toward the clavicle (Figure 1A). Although there was no such anterior or posterior extension, the supraclavicular block’s 3D image showed a uniform transverse spread of the injectate within the plexus sheath, engulfing the superior, middle, and inferior trunks (Figure 1B). For the infraclavicular block, the local anesthetic injectate covering the posterior and lateral cords of the brachial plexus was captured that displayed a 3D elliptical image (Figure 2A).
An ultrasound image of a right interscalene block (A) with a corresponding three-dimensional (3D) image of the local anesthetic injectate in transverse and longitudinal views; an ultrasound image of a right supraclavicular block (B) with a corresponding 3D image of the local anesthetic injectate in transverse and longitudinal views. LT, lateral; ME, medial; AT, anterior; PT, posterior; LA, local anesthetic; ST, superior trunk; MT, middle trunk; IT, inferior trunk; SCA, subclavian artery.
An ultrasound image of a right infraclavicular nerve block (A) with a corresponding three-dimensional (3D) image of the local anesthetic injectate in transverse and longitudinal views; an ultrasound image of a left axillary block (B) with a corresponding 3D image of the local anesthetic injectate in transverse and longitudinal views. CR, cranial; CD, caudal; ME, medial; LT, lateral; LA, local anesthetic; MC, medial cord; LC, lateral cord; PC, posterior cord; UN, ulnar nerve; RN, radial nerve; MN, median nerve; McN, musculocutaneous nerve; AA, axillary artery; AV, axillary vein.
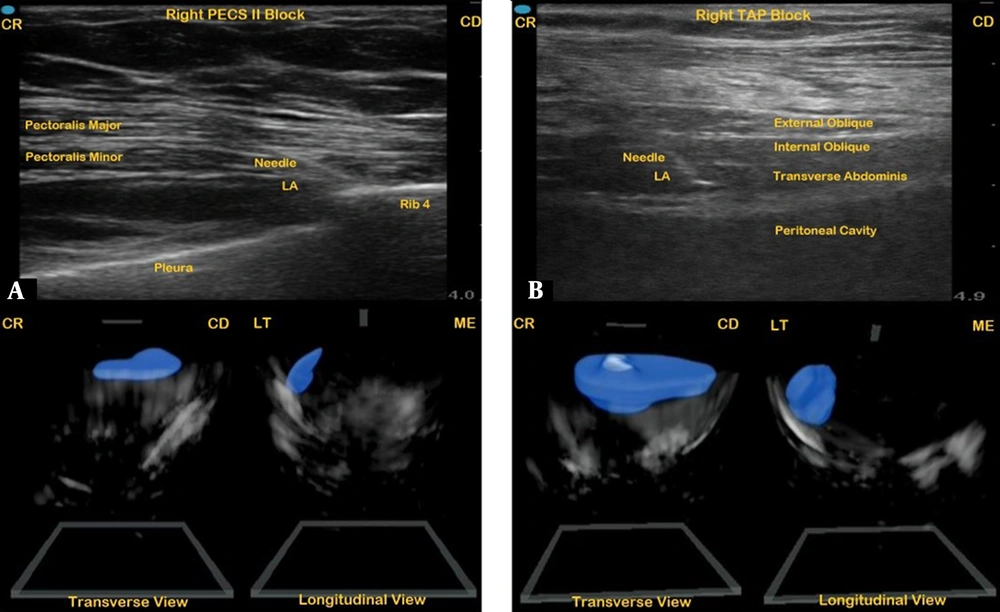
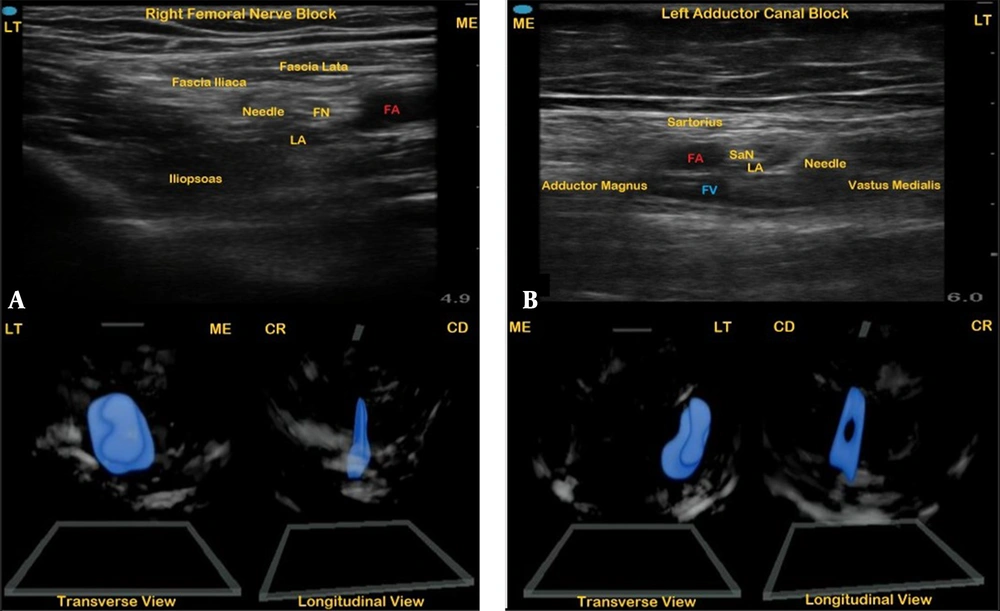
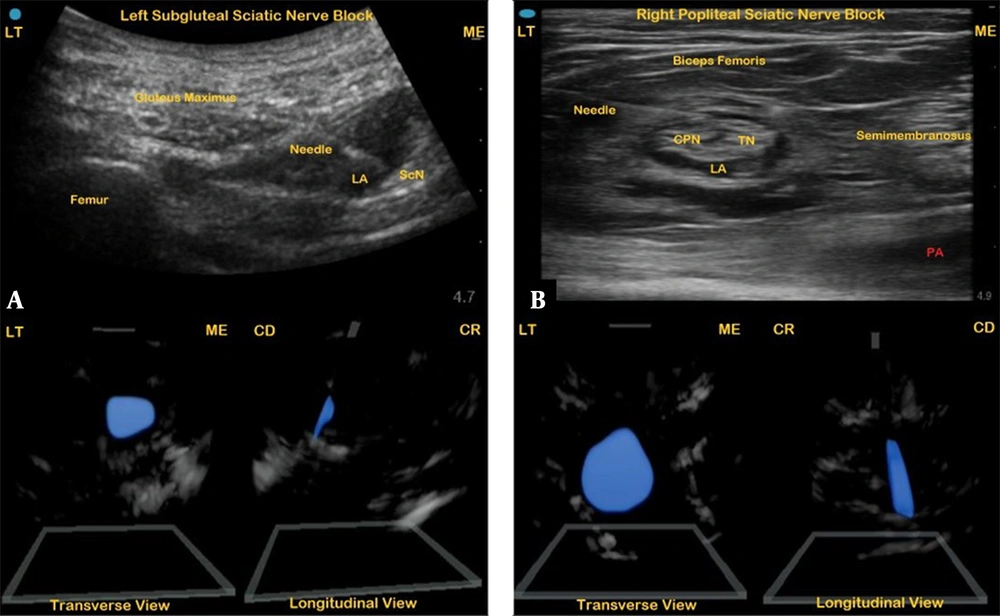
The 3D picture of the axillary block displayed the local anesthetic injectate laterally enclosing the median and the musculocutaneous nerve (Figure 2B). The local anesthetic injectate of the facial plane blocks, pectoral nerve (Pecs) block (Figure 3A), and transversus abdominis plane block (Figure 3B) yielded flat 3D images within the fascial compartments that extended caudally in both cases. For the lower extremity nerve blocks, the femoral nerve block injectate showed a circumferential spread encircling the femoral nerve producing a spheroid 3D image underneath the fascia iliaca (Figure 4A). A lateral crescent-shaped 3D image of local anesthetic spread was visualized following the placement of the adductor canal block (Figure 4B). The 3D reconstructed image of the local anesthetic spread following the placement of the sciatic nerve block at the subgluteal (Figure 5A) and popliteal (Figure 5B) levels revealed oblique images that displace and encircle the nerve, respectively.
An ultrasound image of a right type II pectoral nerve block (A) with a corresponding three-dimensional (3D) image of the local anesthetic injectate in transverse and longitudinal views; an ultrasound image of a right transversus abdominis plane block (3B) with corresponding 3D image of the local anesthetic injectate in transverse and longitudinal views. CR, cranial; CD, caudal; ME, medial; LT, lateral; LA, local anesthetic.
An ultrasound image of a right femoral nerve block (A) with a corresponding three-dimensional (3D) image of the local anesthetic injectate in transverse and longitudinal views; an ultrasound image of a left adductor canal block (B) with a corresponding 3D image of the local anesthetic injectate in transverse and longitudinal views. LT, lateral; ME, medial; CR, cranial; CD, caudal; LA, local anesthetic; FN, femoral nerve; SaN, saphenous nerve; FA, femoral artery; FV, femoral vein.
An ultrasound image of a left subgluteal sciatic nerve block (A) with a corresponding three-dimensional (3D) image of the local anesthetic injectate in transverse and longitudinal views; an ultrasound image of a right popliteal sciatic nerve block (B) with a corresponding 3D image of the local anesthetic injectate in transverse and longitudinal views. LT, lateral; ME, medial; CR, cranial; CD, caudal; LA, local anesthetic; ScN, sciatic nerve; CPN, common peroneal nerve; TN, tibial nerve; PA, popliteal artery.
5. Discussion
This study demonstrated that 3D image construction from the conventional B-mode ultrasound images of local anesthetic spread following the placement of different peripheral nerve blocks is achievable using a handheld point-of-care ultrasound (PoCUS) system. The retrospective 3D image results in a more dynamic picture allowing for better visualization of local anesthetic spread, assisting clinicians in real-time decisions with more confidence. Moreover, capturing these images at the bedside allows for a quick assessment due to the fast startup times of the app-based smartphone technology associated with the handheld ultrasound device.
Previous studies have reported 3D imaging of selective nerve blocks using either retrospective or prospective real-time 3D construction approaches (6-9). Prospective imaging involves obtaining 3D images directly and waiting for the rendering process to be complete, which can be time-consuming. However, a traditional 2D ultrasound transducer captures multiple 2D plane images while remaining stationary and retrospectively constructs a multiplanar image during the scanning process providing a quick real-time 3D image (9). The present study showed that the retrospective construction process is fast and easy to use regardless of which nerve block was investigated.
The preset tools on the handheld ultrasound system allow for a single probe that is capable of performing many different types of scans over a wide frequency range. Its technology is based on a 2D capacitive micromachined ultrasonic transducer (CMUT) that incorporates thousands of microsensors that combine the capabilities of curved, linear, and phased-array transducers into a single probe (10). The CMUT transducer and its associated software have shown high reproducibility and accuracy in estimating volume (11). The volume factory setting, together with the flat transducer, provides the ability to perform a 3D sweep providing an expanded view of 120 degrees; however, the probe remains stationary. Following the capture of the multiplanar images, a deep neural network based on an artificial intelligence algorithm incorporated every 2D ultrasound image as an input, and the contours of fluid contained in the images are highlighted. Finally, by combining the segmentation results on each image, a 3D model of the fluid is displayed on the screen (12).
The present study observed the 3D images of local anesthetic spread relevant to previous reports. For example, Cash et al. demonstrated a 3D image of the vertical and horizontal alignment of the brachial plexus at the interscalene and supraclavicular levels (13). Therefore, an even anterior and then lateral spread of the injected solution can be anticipated, as demonstrated in the present work, with the connective tissues surrounding roots and trunks interconnected and the brachial plexus situated inside the bordering tissue plane of relevant anatomical structures.
With regard to infraclavicular and axillary blocks, the current study’s 3D images are similar to previous descriptions of incomplete local anesthetic spread with confined deposits of injectate around the axillary artery (6, 14). Fascial plane blocks achieve analgesia by the local anesthetic spread between two fascial layers. The present study successfully visualized the local anesthetic distribution of these blocks using 3D imaging. In the truncal region, the local anesthetic following the placement of a type II Pecs block spreads to the posterior axillary line and over the third and seventh ribs without extending into the cranial axilla region (15). In the abdomen, a transversus abdominis plane block allows for caudal and/or anterolateral spread of the injectate (16). At the femoral region, the present study’s 3D image of the local anesthetic injectate demonstrated an even distribution of local anesthetic around the femoral nerve encased within the fascia iliaca. A crescentic 3D image of the injectate following the placement of the adductor canal block might suggest, as previously reported, that the local anesthetic spread around the saphenous nerve is achieved when the injection is placed after piercing the vastoadductor membrane that roofs the adductor canal rather than in the subsartorial fat compartment above the vastoadductor membrane where only an inconsistent medial or superficial spread over the saphenous nerve and femoral artery can be visualized (17).
The current study’s 3D images of sciatic nerve block injectates at the subgluteal and popliteal levels correspond to the notion that the local anesthetic injectate might displace and encircle the nerve at those levels, respectively. A previous study reported a potential perineural space that is formed by the surrounding muscle epimysium, which widens as it descends caudally, resulting in an encircling spread of local anesthetic around the sciatic nerve (7, 18). The utility of the handheld ultrasound imaging system allowed the researchers to visualize the 2D ultrasound image and the reconstructed 3D image to evaluate the local anesthetic spread in these blocks.
Handheld ultrasound systems are not as available as 2D conventional standalone ultrasounds, although the trend might change. Compared to standalone ultrasound systems (> $50,000), handheld ultrasound devices are less expensive (< $5,000) and ideal for clinicians or hospitals that are financially limited (2). Moreover, professional organizations have endorsed the perioperative use of PoCUS and provide educational resources, such as webinars, podcasts, teaching modules, and hands-on workshops (19). This is particularly promising as the support reinforces the teaching and core competencies that need to develop and maintain proficiency in clinical practice.
Several important limitations of the present study should be mentioned. Firstly, this study was performed at a single center and on a relatively small number of patients, which might affect the generalizability of the results. Secondly, although there are 20 preset clinical functions associated with the software of the handheld ultrasound, there is no specific preset function specifically designed for 3D imaging of peripheral nerve blocks. Thirdly, this study did not evaluate the postoperative analgesic efficacy of the nerve blocks following hospital discharge. It has been demonstrated on countless occasions that regional anesthesia offers superior analgesia over opioid-based analgesia. Nonetheless, future studies are needed to explore the reproducibility of the present study’s clinical findings and utility.
5.1. Conclusions
The present study has shown that a 3D image of a nerve block injectate can be obtained using a portable handheld ultrasound system that captures multiple 2D images of fluid deposits. The 3D images provide clinicians with valuable information on the anatomical boundaries of the injectate that can further direct needle direction and placement of local anesthetic to achieve visual confidence of anesthetic spread. Future larger studies investigating the integration of 3D imaging performed at the bedside are desired to support the evidence to be a component of PoCUS assessment for the professional development of future clinicians.