1. Background
The incidence of uncontrolled intraoperative hypertension is more common in hypertensive patients. Episodes of intraoperative hypertension should be promptly controlled because such elevation of blood pressure can be associated with the increased risk of morbidity and mortality in the postoperative period (1). Proper control of intraoperative blood pressure values with maintaining adequate organ blood flow and perfusion is mandatory (2). Medications used for intraoperative blood pressure control should have a rapid onset of action and can be easily titrated to the desired effect. Several agents are used for the intraoperative control of elevated blood pressure as sodium nitroprusside, esmolol, phentolamine, and nitroglycerine (1). Nitroglycerine is a direct vessel wall vasodilator with greater venodilator effect than arterial dilator effect. It is used as an anti-anginal and antihypertensive drug. This medication plays a role in reducing blood pressure through decreasing preload and cardiac output. However, it carries the risk of reflex tachycardia and hypotension which are exacerbated by volume depletion commonly present in hypertensive patients (3). Dexmedetomidine is a highly selective alpha-2 (α2) adrenergic agonist with sympatholytic, opioid sparing, and analgesic effects. Therefore, it can attenuate hemodynamic and stress response to surgery (1, 4). Dexmedetomidine exerts its action on α2 receptors which are widely distributed, such as in the nervous system (peripheral, central, and autonomic), blood vessels, and body organs. This distribution leads to its anxiolytic, sedative, sympatholytic, and vasodilator effects (5). The sympatholytic effect of dexmedetomidine results in the reduction of mean arterial pressure (MAP) and heart rate (HR) through inhibiting norepinephrine release (6).
2. Objectives
The aim of the current study was to compare nitroglycerine infusion with dexmedetomidine infusion for controlling accidental intraoperative uncontrolled hypertension.
3. Methods
The current prospective cohort comparative study was conducted in National Cancer Institute during August 2021-November 2022 after approval by the Institutional Review Board. The study was registered prospectively in clinical trials.gov (NCT04953156). Data for the nitroglycerine group (retrospective group) were retrieved from the medical records of ASA II cancer patients with controlled hypertensive conditions who underwent surgery under general anesthesia and experienced uncontrolled intraoperative hypertension which required nitroglycerin infusion during July 2020-July 2021. Data for the dexmedetomidine group were prospectively collected from ASA II cancer patients with controlled hypertension who experienced uncontrolled intraoperative elevated blood pressure during general anesthesia during August 2021-August 2022.
Study population included patients above 18 years old who underwent cancer resection surgical procedures under general anesthesia and developed accidental uncontrolled hypertension. The exclusion criteria were patients on beta blockers with HR below 55 beats/min, kidney or liver function impairment, bradycardia, any degree of heart block and severe cardiorespiratory disease, pheochromocytoma, major blood loss, and major fluid shift.
3.1. Medical Intervention
All patients received 2 mg dormicum after the insertion of intravenous line in the holding area. In the operating theatre, all patients were monitored using electrocardiogram, non- invasive blood pressure monitoring, capnography, and oxygen saturation using pulse oximeter. Anesthesia was induced by intravenous 2 mg/kg propofol, 0.6 mg/kg rocuronium, and 2 µg/kg fentanyl. Maintenance of anesthesia was achieved through controlled mechanical ventilation and inhalational anesthesia by either sevoflurane or isoflurane with 50% Fio2. Intraoperative analgesia was attained using either intravenous morphine 0.1 mg/kg, epidural analgesia, or regional wall blocks in some cases. In case of an increase in either blood pressure or heart rate above 20% from the baseline 50 µg fentanyl was administered to exclude inadequate analgesia. Upon the administration of medications for hemodynamic control (either nitroglycerine or dexmedetomidine), invasive blood pressure monitoring using Datex-Ohmeda 3030, Carestation 620 B40 monitor (General Electric: Madison, USA) was performed. The HR and blood pressure were continuously monitored and documented every 10 min.
For the dexmedetomidine group, after the exclusion of inadequate analgesia or anesthesia as the cause of uncontrolled hypertension, patients were assigned to receive dexmedetomidine bolus of 1 µg/kg infused over 20 min and then continuous infusion of 0.2 - 0.7 µg/kg/h adjusted according to each patient’s hemodynamic response. Initially, dexmedetomidine infusion was started after the elevation of blood pressure 20% above the baseline and was adjusted according to blood pressure values. The infusion was deescalated when blood pressure values reached the baseline and/or HR lowered below 50 bpm. Infusion was stopped in cases where blood pressure decreased 20% below the baseline or reported persistent bradycardia with HR less than 45 bpm. In case of persistent bradycardia after the cessation of infusion, a bolus of intravenous 0.5 mg atropine was administered and repeated as needed. For the nitroglycerine group, data retrieved included patients who received nitroglycerine infusion due to uncontrolled intraoperative elevation of blood pressure. Patients received nitroglycerin infusion (0.3 - 1 µg/kg/min) titrated according to each patient’s hemodynamic response. First, nitroglycerine infusion was started according to our institutional protocol after elevation of blood pressure 20% above the baseline and was adjusted based on blood pressure values. Infusion was deescalated when blood pressure values reached the baseline and stopped in cases where the blood pressure values decreased 20% below the baseline values. In both groups, lowered MAP less than 60 mmHg was managed by administration of a bolus dose of ephedrine 10 mg which was repeated as needed and documented. Data about blood loss and blood transfusion were not collected due to the difference in the types of surgeries included in the study.
3.2. Sampling and Sample Size
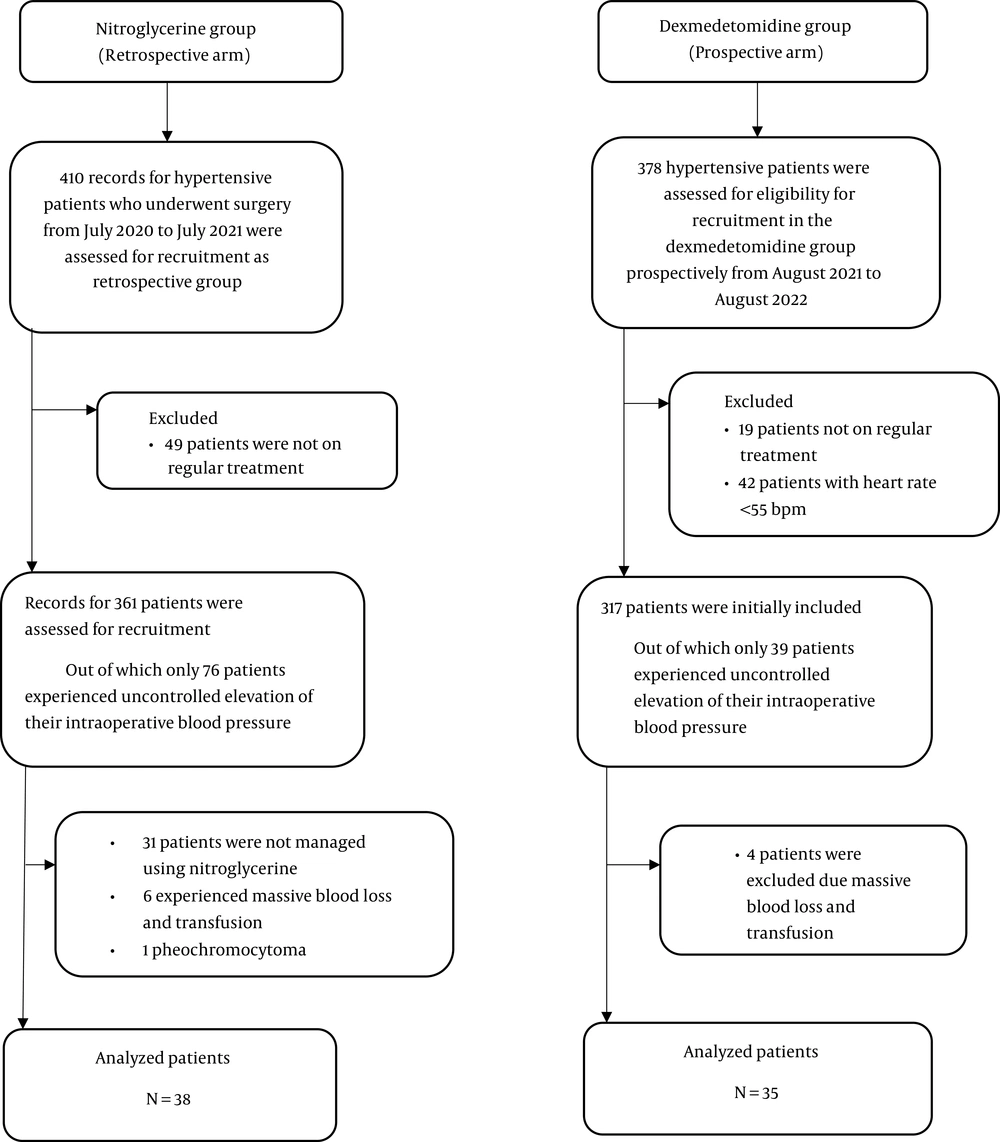
Consecutive sampling technique was used to recruit all eligible patients in both groups during one year. For retrospective control arm (nitroglycerin group), the records of 410 hypertensive patients were assessed for eligibility during July 2020-July 2021 and only 76 records were included. Finally, records meeting the eligibility criteria were retrieved for 38 patients. For prospective arm (dexmedetomidine group), a total of 378 hypertensive patients were assessed for eligibility during August 2021-August 2022, and 317 patients were first included, out of which only 39 cases were eligible and finally, 35 patients were included in the analysis (Figure 1).
3.3. Statistical Analysis
Data were analyzed using IBM statistical package for social sciences (SPSS) version 27 (SPSS Inc., Chicago, IL). The chi-squared test and independent t-test were used to compare nitroglycerine and dexmedetomidine groups for categorical and numerical variables, respectively. The RASS scores were compared between the studied groups by Mann-Whitney test. P-value < 0.05 was considered statistically significant.
3.4. Study Outcomes
Primary outcome included intraoperative blood pressure values. Secondary outcomes were perioperative HR values, postoperative blood pressure values, postoperative opioid consumption, episodes of bradycardia, episodes of rebound hypertension, and postoperative sedation score based on the Ramsay Sedation Scale (RSS) in the post-anesthesia care unit (PACU) (Table 1).
| Score | Definition |
|---|---|
| 1 | Anxious and agitated or restless or both |
| 2 | Cooperative, oriented, and tranquil |
| 3 | Responds to commands only |
| 4 | Brisk response to a light glabellar tap or loud auditory stimulus |
| 5 | Sluggish response to light glabellar tap or loud auditory stimulus |
| 6 | No response to light glabellar tap or loud auditory stimulus |
Ramsay Sedation Scale
4. Results
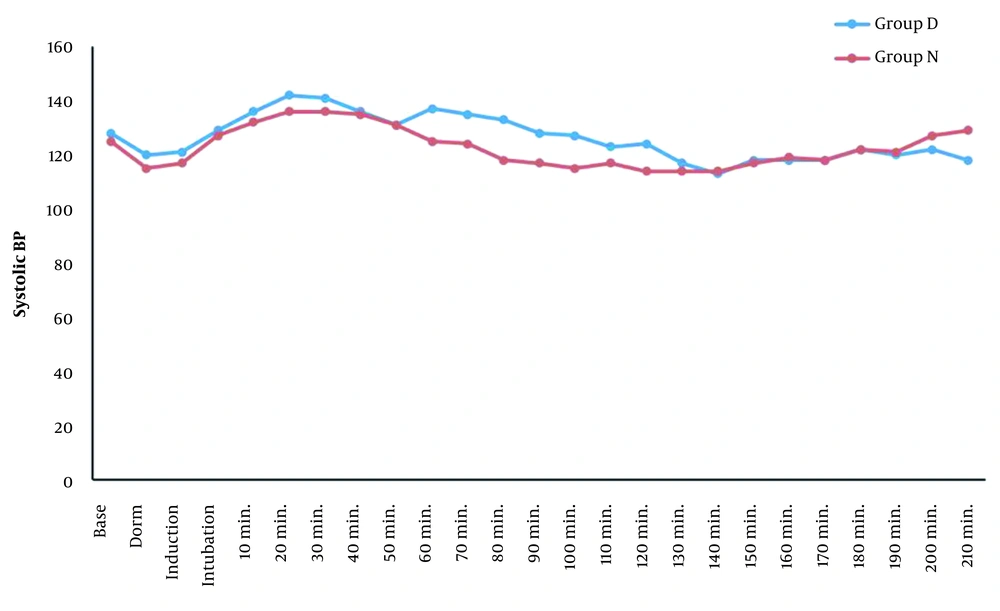
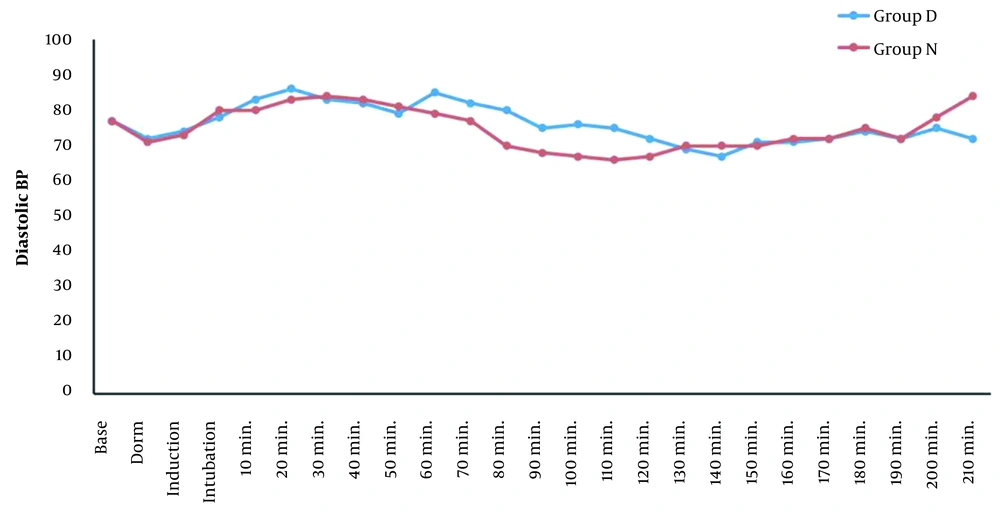
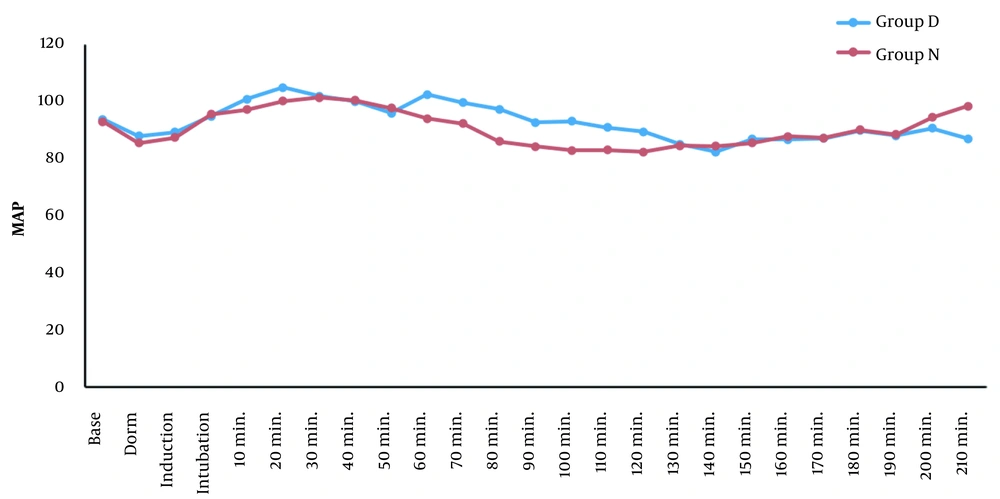
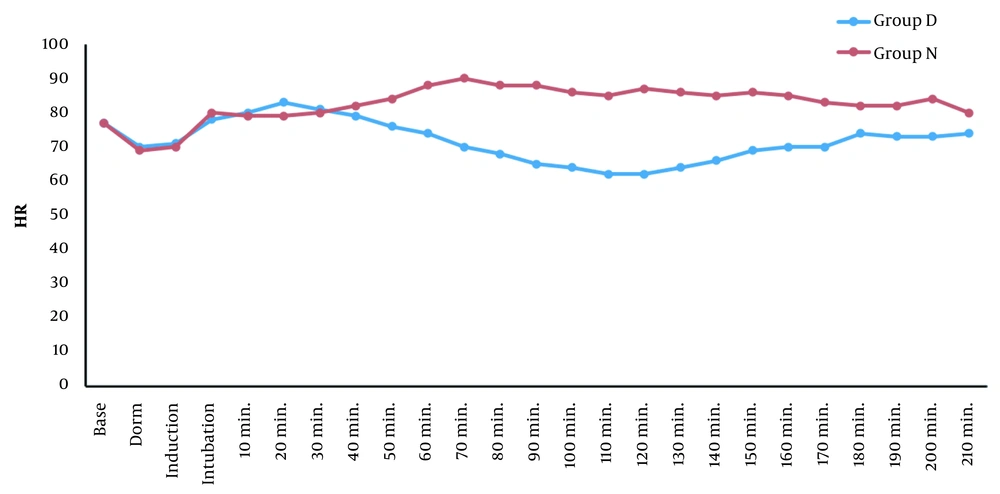
Demographic data, clinical characteristics, and the type of surgery were comparable for the two groups (Table 2). There was no significant difference recorded between the groups for systolic pressure, diastolic pressure, and MAP values for the baseline, after sedation, during induction, after intubation, the first 50 min intraoperatively, and the last 1.5 h of the surgery. On the other hand, systolic pressure, diastolic pressure, and MAP were significantly lower in the nitroglycerine group staring from 60 min intraoperatively until 120 min (Figures 2, 3 and 4). The HR was comparable between the two groups for the baseline, after sedation, during induction, after intubation, the first 40 min intraoperatively, and the last minutes of surgery. Alternatively, HR values were significantly lower in the dexmedetomidine group staring from 50 min intraoperatively almost until the end of surgery (Figure 5). Seven patients in the nitroglycerine group experienced hypotension with MAP < 60, of which five patients needed intervention with a bolus of 10 mg ephedrine versus three patients in the dexmedetomidine group where only one received 10 mg ephedrine. Incidence of bradycardia was higher in the dexmedetomidine group, where nine patients experienced bradycardia versus no patients in the nitroglycerin group (P < 0.001). On the other hand, the incidence of rebound hypertension was significantly higher for the nitroglycerine group (n = 7) compared to the dexmedetomidine group (n = 1) (P = 0.003; Table 3). In the post-anesthesia care unit, the dexmedetomidine group had lower HR values, lower systolic pressure, diastolic pressure, and MAP, compared to the nitroglycerin group (Table 4). The RSS scores were significantly higher with more sedation in the dexmedetomidine group compared to the nitroglycerine group (P < 0.001). Furthermore, the dexmedetomidine group showed lower postoperative morphine consumption compared to the nitroglycerine group in the PACU (P < 0.001; Table 3).
| D (n = 35) | N (n = 38) | P-Value | |
|---|---|---|---|
| Age (y) | 54.9 ± 9.0 | 51.7 ± 9.7 | 0.144 |
| Range | 37 - 69 | 33 - 70 | |
| Gender | 0.415 | ||
| Female | 19 (54.3) | 17 (44.7) | |
| Male | 16 (45.7) | 21 (55.3) | |
| BMI (kg/m2) | 27.7 ± 4.9 | 27.2 ± 3.6 | 0.621 |
| Range | 20.3 - 37.1 | 21.1 - 34.4 | |
| Treatment of HTN * | |||
| ACEIs | 7 (20.0) | 6 (15.8) | 0.639 |
| ARBS | 12 (34.3) | 15 (39.5) | 0.646 |
| Ca channel blocker | 9 (25.7) | 10 (26.3) | 0.953 |
| Diuretics | 6 (17.1) | 9 (23.7) | 0.490 |
| B blocker | 14 (40.0) | 12 (31.6) | 0.453 |
| DM | 0.729 | ||
| No | 17 (48.6) | 20 (52.6) | |
| Yes | 18 (51.4) | 18 (47.4) | |
| Type of surgery | NA | ||
| Thyroidectomy | 7 (20.0) | 10 (26.3) | |
| Hemicolectomy | 7 (20.0) | 7 (18.4) | |
| Hysterectomy | 8 (22.9) | 3 (7.9) | |
| Mastectomy | 6 (17.1) | 7 (18.4) | |
| Nephrectomy | 4 (11.4) | 6 (15.8) | |
| Ovariectomy | 1 (2.9) | 2 (5.3) | |
| Hemi glossectomy | 0 (0) | 2 (5.3) | |
| Lymph node excision | 1 (2.9) | 0 (0) | |
| Scalp ulcer excision | 1 (2.9) | 0 (0) | |
| Glossectomy | 0 (0) | 1 (2.6) |
| D (n = 35) | N (n = 38) | P-Value | |
|---|---|---|---|
| Incidence of bradycardia | < 0.001 | ||
| No | 26 (74.3) | 38 (100.0) | |
| Yes | 9 (25.7) | 0 | |
| Rebound HTN | 0.033 | ||
| No | 34 (97.1) | 31 (81.6) | |
| Yes | 1 (2.9) | 7 (18.4) | |
| Postoperative morphine consumption | 0.001 | ||
| 0 | 22 (62.9) | 8 (21.6) | |
| 3 | 12 (34.3) | 24 (64.9) | |
| 6 | 1 (2.9) | 5 (13.5) | |
| RSS | < 0.001 | ||
| Median (range) | 3 (2 - 5) | 2 (1 - 3) |
| PACU (min) | D | N | P-Value |
|---|---|---|---|
| SBP | |||
| 30 | 122 ± 13 | 137 ± 15 | < 0001 |
| 60 | 121 ± 7 | 131 ± 10 | < 0001 |
| 90 | 121 ± 5 | 128 ± 8 | < 0001 |
| 120 | 123 ± 5 | 127 ± 7 | 0.004 |
| DBP | |||
| 30 | 75 ± 9 | 83 ± 8 | < 0001 |
| 60 | 74 ± 5 | 79 ± 6 | < 0001 |
| 90 | 74 ± 5 | 78 ± 4 | < 0001 |
| 120 | 75 ± 4 | 77 ± 4 | 0.030 |
| MAP | |||
| 30 | 91 ± 10 | 101 ± 10 | < 0.001 |
| 60 | 90 ± 6 | 96 ± 7 | < 0.001 |
| 90 | 90 ± 5 | 95 ± 5 | < 0.001 |
| 120 | 91 ± 4 | 94 ± 5 | 0.011 |
| HR | |||
| 30 | 65 ± 8 | 78 ± 10 | < 0001 |
| 60 | 66 ± 6 | 75 ± 7 | < 0001 |
| 90 | 67 ± 4 | 76 ± 5 | < 0001 |
| 120 | 68 ± 4 | 76 ± 5 | < 0001 |
Systolic Pressure, Diastolic Pressure, Mean Arterial Pressure, and Heart Rate Values in Post Anesthesia Care Unit a
5. Discussion
Cancer resection surgeries usually have a complex extensive operative field. Consequently, proper control of intraoperative blood pressure results in a clearer surgical field with lower incidence of operative blood loss (7). Intraoperative hypertension can be encountered in hypertensive patients undergoing surgeries under general anesthesia. This elevation may result from intubation or sympathetic stimulation following surgical stimulation (3). Although it has been reported that the elevation of blood pressure can be encountered in hypertensive as well as non-hypertensive patients following stress response to intubation or surgical stress (8), such hypertensive episodes in non-hypertensive patients usually respond to anesthesia and/or analgesia deepening. In the current study, patients showed variable responses to different stimuli where some patients experienced hypertension following intubation, while others had hypertension after experiencing surgical stimulation. Both stimuli were managed initially with the administration of analgesic drugs or deepening the level of anesthesia. However, such maneuvers did not result in the control of blood pressure elevation in all patients. Judicious control of blood pressure was our target, with individualized tailoring of the accepted lower threshold for each patient. Generally, mean arterial blood pressure of 65 mmHg or lowering 20% - 30% of the preoperative baseline were considered tolerated as the lower accepted threshold. We avoided further reduction of intraoperative blood pressure as such reduction could result in the increased risk of postoperative morbidity, especially in elder patient population (2). We prospectively examined dexmedetomidine infusion for hypertension control versus the retrospective use of nitroglycerine infusion from our institutional medical reports. Nitroglycerine infusion has long been used as a hypotensive agent during general anesthesia (9). Such continuity might be due to the potential merits offered by the medication usage as it was initially used to reduce intraoperative blood loss, and then, it was used widely as a controlled hypotensive agent (9, 10). However, nitroglycerine infusion results in reflex tachycardia with the increased risk of hypotensive episodes especially in older patients (11, 12). Dexmedetomidine was first introduced as a sedative and anxiolytic drug that exerts hemodynamic effect through both central and peripheral receptor stimulation. It was noticed that the rapid infusion of dexmedetomidine loading dose over less than 10 min can lead to hypertension through activating peripheral α2a receptors, while slow infusion results in the activation of central α2a receptors with the subsequent inhibition of noradrenaline release and lowering of HR and blood pressure (5). Moreover, dexmedetomidine infusion has a neuroprotective effect with reducing cerebral oxygen consumption and decreased incidents of cognitive dysfunction postoperatively (7). In the current study, we observed that patients who received dexmedetomidine infusion showed more hemodynamic stability with fewer episodes of intraoperative hypotension, tachycardia, and rebound elevation of blood pressure after discontinuation of the drug infusion. In addition, there was longer time to receive postoperative analgesia, less postoperative opioid consumption, and better postoperative sedation scores. In a study with similar results to the current study, Vali et al. compared the efficacy of dexmedetomidine versus nitroglycerine infusion for inducing controlled hypotensive anesthesia during spine surgeries. They reported that dexmedetomidine infusion showed better intraoperative and postoperative outcomes regarding more hemodynamic stability, less rebound hypertensive episodes, and better immediate postoperative sedation scores (13). Bajwa et al. assessed the impact of nitroglycerin, dexmedetomidine, and esmolol infusion on controlled hypotensive anesthesia in patients undergoing functional endoscopic sinus surgeries. They reported that patients who received dexmedetomidine showed more intraoperative hemodynamic stability with clearer operative bed, lower postoperative analgesic requirements, and better postoperative sedation scores (14). In a study by Salah et al., rebound hypertension and tachycardia were reported following the cessation of dexmedetomidine infusion in 32% of their study population. Such complication was not encountered during our analysis. The latter difference might be related to the variation in the population analyzed and that they continued the infusion up to 6 h, while in the current study, the infusion lasted not more than 3 h (15). In the present investigation, only three patients in the dexmedetomidine group had a decrease of below 45 bmp in their HR values which was reversed in two patients after infusion cessation and one patient needed to receive 1 mg intravenous atropine. Bradycardia reported with dexmedetomidine infusion was noticed to predominantly affect young age patients with increased vagal tone. However, dexmedetomidine use should not be advocated for patients with any degree of heart block, structured heart disease, or reduced ventricular function (16). Here, we report that both nitroglycerine infusion and dexmedetomidine infusion can be used to control uncontrolled elevation of intraoperative blood pressure in cancer patients undergoing cancer surgery. However, the medication choice should be customized based on each individual case to obtain the optimal response.
5.1. Conclusions
The results of the current study showed that both nitroglycerine and dexmedetomidine infusion can be used in the control of elevated intraoperative blood pressure in hypertensive patients, with additional merits for dexmedetomidine infusion, such as hemodynamic stability and better postoperative sedation scores with less opioid consumption.