1. Background
Following an abdominal hysterectomy, extreme pain must be treated using a multi-modal pain control strategy. Opioids may lead to lethargy, vomiting, nausea, constipation, tolerance, physical dependency, respiratory depression, and others. To limit opiate consumption and its negative implications, alternative pain management options are required (1-3).
Pain fibers from the uterine body travel with sympathetic nerves via the lumbar splanchnic nerves and hypogastric plexus to the T10-L1 dorsal roots (4). Ultrasound-guided Ilioinguinal/Iliohypogastric nerve blocks (IINB) and transversus abdominis block (TAB) reduce surgical incisional discomfort by blocking the afferent sensory nerves running among the abdominal muscles (5).
TAP, also called inter-fascial plane block, is different from the quadratus lumborum block (QLB). It is a block of the posterior abdominal wall. Since it involves the injection of a locanesthetictic into the thoracolumbar fascia (TLF), it is the posterior continuation of the abdominal wall muscle fascia involving the muscles of the back (namely psoas major [PM], quadratus lumborum [QL], and the erector spinae [ES] muscles). To the best of our knowledge, no study has compared the QLB for patients having hysterectomies with the dual TAB with IINB6 (6).
2. Objectives
This study compared the analgesic effectiveness of bilateral ultrasound-guided QLB for total abdominal hysterectomy with that of the bilateral ultrasound-guided TAB and IINB. The total amount of morphine utilized within the first day postoperatively was the main consequence. Other outcomes included several individuals who needed rescue analgesia, postoperative analgesia duration, and the postoperative pain visual analog score (VAS) half an hour and two, four, six, twelve-, and 24 hours after surgery.
3. Methods
From May to October 2020, 60 female patients aged 45 - 60 years were scheduled to undergo the surgery of total abdominal hysterectomy anesthesia spinal anesthesia. They were in ASA Physical Status Classes I and II at the Gynecologic Department of the Tanta University Hospital and enrolled in this randomized prospective study.
The study was approved by the Research Ethics Committee of the Faculty of Medicine of the Tanta University (Code: 33799/4/20 registered on the ClinicalTrials.gov website (ID: NCT04382274)). From May to October 2020, 60 female patients aged 45 - 60 years were scheduled to undergo the surgery of total abdominal hysterectomy under spinal anesthesia. They were in ASA Physical Status Classes I and II at the Gynecologic Department of the Tanta University Hospital and participated in this randomized trial.
The participants were excluded due to injection site infection, local anesthetics allergy, bleeding issues, mental or physical diseases affecting the pain score assessment, morbid obesity, liver failure, and renal failure.
Routine preoperative laboratory testing was performed for all participants. Pulse oximetry, non-invasive blood pressure monitoring, and electrocardiography were all performed when the patient first arrived in the operating room. The following vital signs were recorded at baseline. An intravenous line (IV) was placed, and IV fluid administration began. Oxygen was delivered by nasal cannula at a rate of 4 liters/ minute, and spinal anesthesia by 25 mcg fentanyl and 15 mg hyperbaric bupivacaine was carried for the two groups.
After confirming an adequate dermatomal blockade level (to at least the T8 dermatome), the 60 individuals were randomly assigned to either the QLB or dual TAB groups (30 patients each). After constructing a list of numbers, each one was wrapped in an opaque envelope and referenced to one of the two groups. An anesthesiologist then delivered one of the envelopes to each patient and assigned them to one of the two groups based on a comparison to the computer-generated list. The block was conducted by an anesthesiologist not participating in data collection and result analyses.
Both blocks were carried out using an ultrasonic machine, a probe sheathed in sterile material under strict aseptic conditions (China, Sonoscape® SSI-6000 with 12-6 MHz linear probe with high or low frequency), and 22G, 100 mm needle (B Braun Medical Inc., Bethlehem, PA, USA).
The dual-TAB group had bilateral ultrasound-guided dual TAB (integrating II nerve blocks with TAB). The layers of the external, internal, and transverse oblique muscles (EO, IO, TA) were found when the probe was positioned at the anterior axillary line between the lower costal margin and the iliac crest. Then 20 mL of bupivacaine 0.25% was injected between the TA and IO muscles after negative aspiration. On the other hand, a similar strategy was adopted. The umbilical–anterior superior iliac spine (ASIS) line was used to scan the abdomen for IINB. The ilioinguinal nerve runs between the transverse and internal oblique nerves. Following a negative aspiration, 10 milliliters of bupivacaine 0.25% was injected. On the other side, a similar technique was used.
In the QLB group (anterior termed QLB3), to get greater exposure in this group, the operating table was inclined to the opposite side. Above the iliac crest, a convex low-frequency probe was mounted vertically, and an anteromedial needle was inserted into the plane via QL. Between the QL and PM muscles, the tip of the needle was inserted. PM, QL, and erector spinae act as the "three cloves of the shamrock," while the transverse process of L4 serves as the "stem" of the "shamrock symbol," and the precise needle site was confirmed with hypoechoic imaging and the hydro dissection of 1 - 2 mL of normal saline following negative aspiration. On the other side, the procedure was performed once more with a 20 mL injection of 0.25% bupivacaine (7).
The same surgeon performed an open hysterectomy with a low transverse incision in both groups. All patients received a gram of paracetamol IV about 30 minutes before the operation. The patients were transported to the post-anesthesia care unit (PACU) after being released from the operating room.
Age, body mass index (BMI), Physical Status Class of American Society of Anesthesiologists (ASA), duration of anesthesia, and surgery duration were all involved in the demographic data. The VAS for pain (an analogue scale with 0 representing no pain and 10 representing maximum discomfort) was used to measure the severity of postoperative pain at intervals of half an hour and 2, 4, 6, 12, and 24 hours. Three milligrams of morphine was administered intravenously to patients with VAS = 4. A one-gram intravenous paracetamol infusion was given to the patients with VAS = 4. The total quantity of morphine consumed after surgery (rescue analgesia) and the duration of postoperative analgesia during the first 24 hours after surgery (the interval between recovery and the first dosage of morphine), as well as the number of individuals who required rescue analgesia, arrhythmia, bradycardia (50 beats/min), postoperative hypotension (systolic arterial pressure 90 mmHg), vomiting or nausea, lower limb muscular weakness, as well as any additional complications, were also recorded.
3.1. Statistical Analysis
The G*Power tool, edition 3.1.9.2 (University of Düsseldorf, Düsseldorf, Germany), was used to calculate the sample size. Each group requires a sample size of 26 instances regarding the following parameters: 0.05 error and 90% power to demonstrate a 35% reduction in the need for postoperative morphine (the primary outcome) with QLB versus TAB/ IINB (according to a prior study). To prevent dropout, four instances were added to each group (8). IBM SPSS software version 20.0 was used to analyze the data used as the input to the computer (IBM Corporation, Armonk, New York). When analyzing and comparing categorical variables between the two groups, the chi-square test (Fisher's Exact correction) was used to investigate the distribution normality of the variables. The Mann-Whitney test was used to compare both groups with non-normally distributed quantitative data, whereas the student t-test was used to compare both groups with normally distributed quantitative data. In this study, P < 0.05 was set as the significance level.
4. Results
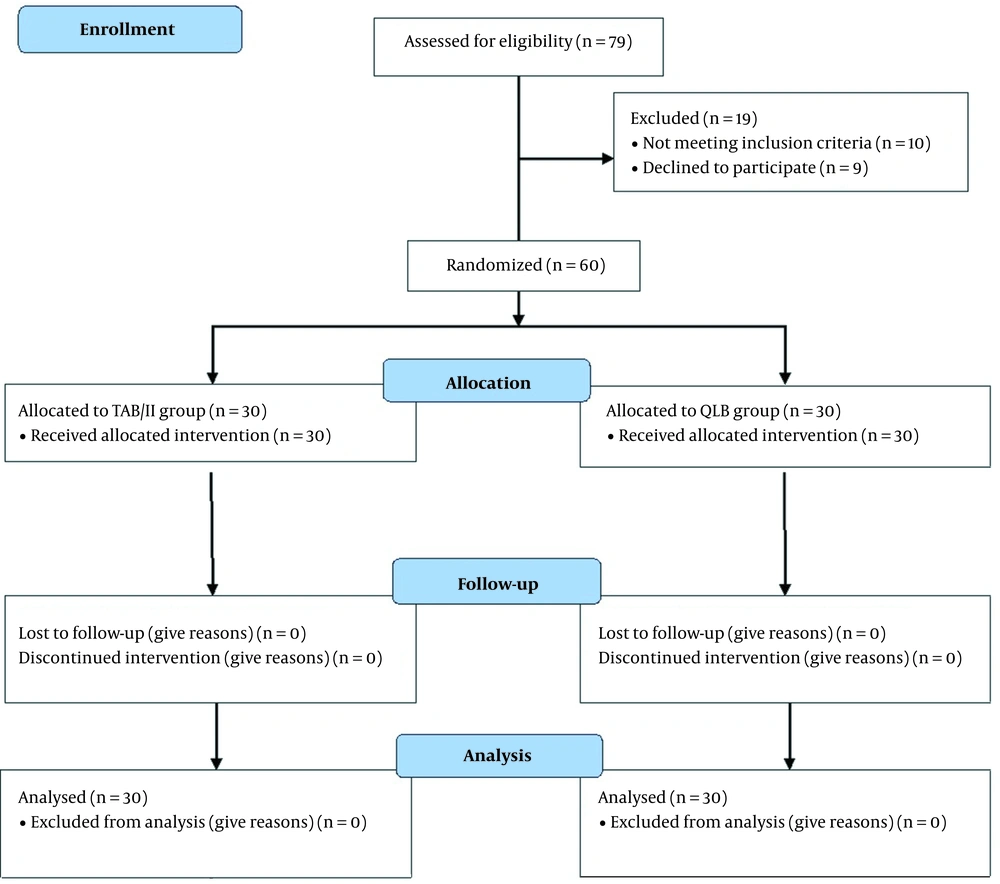
Seventy-nine individuals participated in this study, of whom 19 persons were excluded (nine refused to participate, 10 owing to exclusion criteria), and 60 individuals were assigned to two equal groups (Figure 1).
The participants’ mean age was 53.8, and 53 years in Groups A and B., with BMI of 30 and 29.6 kg/m2, respectively. The patients with ASA class I accounted for 60% and 66.7% of patients in the same groups, respectively; however, the others had ASA class II. The three research parameters were statistically equivalent between the two study groups (P > 0.5). There was no statistically significant difference in anesthesia or surgical time between the two groups (P = 0.908 and P = 0.873, respectively).
Morphine consumption was comparable (P = 0.908) between the two groups, with the mean values of 10 and 9.9 mg, respectively. Furthermore, the analgesia duration was statistically non-significant (P = 0.879) between the two groups, with mean values of 15.4 and 15.6 hours, respectively. There was no statistically significant difference between the groups regarding postoperative complications. In the two study groups, 16.7% of the patients experienced hypotension. Furthermore, bradycardia was found in 13.3% and 16.7% of the patients, respectively, while nausea and vomiting were at the same rate in the QLB and TAB/IINB groups (Table 1).
| QLB (n = 30) | TAB/IINB (n = 30) | Statistics a | P-Value | |
|---|---|---|---|---|
| Age, y | t = 0.570 | 0.571 | ||
| Mean ± SD | 53.8 ± 5.1 | 53 ± 6.2 | ||
| Median (min – max) | 55 (39 – 60) | 55 (39 – 60) | ||
| BMI, kg/m2 | t = 0.606 | 0.547 | ||
| Mean ± SD | 30 ± 2.7 | 29.6 ± 2.8 | ||
| Median (min – max) | 30 (23 – 35) | 30 (23 – 35) | ||
| ASA | χ2 = 0.287 | 0.592 | ||
| I | 18 (60%) | 20 (66.7%) | ||
| II | 12 (40%) | 10 (33.3%) | ||
| Anesthesia duration, min | t = 1.003 | 0.321 | ||
| Mean ± SD | 130.4 ± 5.4 | 132.2 ± 8.2 | ||
| Median (min – max) | 130 (120 – 140) | 130 (120 – 150) | ||
| Surgical duration, min | t = 0.116 | 0.908 | ||
| Mean ± SD | 107.1 ± 5.1 | 106.8 ± 9.8 | ||
| Median (min – max) | 107.5 (99 – 118) | 105 (90 – 125) | ||
| Intravenous morphine dose, mg | t = 0.160 | 0.873 | ||
| Mean ± SD | 10 ± 1.8 | 9.9 ± 2.4 | ||
| Median (min – max) | 10 (6.8 – 13) | 10 (6 – 14) | ||
| Duration of analgesia, min | t = 0.154 | 0.879 | ||
| Mean ± SD | 15.4 ± 4.4 | 15.6 ± 5.6 | ||
| Median (min – max) | 13 (12 – 24) | 12 (12 – 24) | ||
| Hypotension | 5 (16.7%) | 5 (16.7%) | χ2 = 0.000 | 1.000 |
| Bradycardia | 4 (13.3) | 5 (16.7%) | χ2 = 0.131 | 1.000 b |
| PONV | 4 (13.3) | 5 (16.7%) | χ2 = 0.131 | 1.000 b |
Abbreviations: QLB, quadratus lumborum block; TAB/IINB, transversus abdominis block/ilioinguinal/iliohypogastric nerve block; PONV, postoperative nausea and vomiting; SD, standard deviation; ASA, American Society of Anesthesiologists; BMI, body mass index.
at, student t-test; χ2, chi-square test
b Fisher’s exact test
Regarding postoperative VAS, it was statistically equivalent between the two study groups 24 hours after surgery (P > 0.05). (Table 2).
| VAS | QLB (n = 30) | TAB/IINB (n = 30) | P-Value |
|---|---|---|---|
| 30 min | 0.690 | ||
| Mean ± SD | 1.9 ± 0.3 | 1.9 ± 0.3 | |
| Median (min – max) | 2 (1 – 2) | 2 (1 – 2) | |
| 2 h | 0.690 | ||
| Mean ± SD | 1.9 ± 0.3 | 1.9 ± 0.3 | |
| Median (min – max) | 2 (1 – 2) | 2 (1 – 2) | |
| 4 h | 0.426 | ||
| Mean ± SD | 2 ± 0.4 | 1.9 ± 0.3 | |
| Median (min – max) | 2 (1 – 3) | 2 (1 – 2) | |
| 6 h | 0.970 | ||
| Mean ± SD | 2 ± 0.5 | 2 ± 0.2 | |
| Median (min – max) | 2 (1 – 3) | 2 (1 – 2) | |
| 12 h | 0.178 | ||
| Mean ± SD | 3.6 ± 1.1 | 3.6 ± 0.7 | |
| Median (min – max) | 4 (1 – 5) | 4 (2 – 4) | |
| 24 h | 0.358 | ||
| Mean ± SD | 3.9 ± 1.1 | 3.7 ± 1 | |
| Median (min – max) | 4 (2 – 6) | 4 (2 – 6) |
Abbreviations: SD, standard deviation; U, Mann Whitney test; QLB, quadratus lumborum block; TAB/IINB, transversus abdominis block/ilioinguinal/iliohypogastric nerve block; VAS, visual analog score; h, hours.
5. Discussion
The present study aimed to evaluate the analgesic efficacy of bilateral ultrasound-guided QLB with bilateral ultrasound-guided TAB/ IINB after a hysterectomy. Similar to the TAB/IINB group, the QLB group was provided with postoperative analgesia. To the best of our knowledge, this study was the first study comparing the two blocks.
In the present study, the two groups' postoperative VAS scores, morphine intake, and analgesia duration were comparable. To avoid postoperative morphine side-effects such as nausea, itching, respiratory depression, and somnolence, the lower doses of both blocks were also required (9, 10).
The T12-L2 nerves anatomically offer significant sensory innervation to the inguinal area. T12 and L1 branches carry the ilioinguinal nerve and iliohypogastric nerve between IO and TA at a level directly above ASIS (11). TAB and IINB both include injecting a local anesthetic into the area between the IO and TA; however, at various locations along the nerve pathways, the injection in IINB is closer to the nerve. Compared to the TAB block, IINB may need less local anesthesia to provide the same degree of analgesia, particularly when delivered with ultrasound guidance (12).
According to some cadaver investigations (13, 14), the thoracic paravertebral space, intercostal spaces, somatic nerves, and thoracic sympathetic trunk up to the level of T4 may all be covered by the contrast injection. The subcostal, iliohypogastric, and ilioinguinal nerves are all persistently suppressed. Both lateral femoral and the genitofemoral cutaneous nerves are likely to get partly inhibited. Obviously, there are differences in the breadth of analgesia accomplished and the dermatomes number covered by QLB. As mentioned in many reports , analgesic effects at the T7-L1 dermatomes explained by dispersion of local aneasthetics cranially to T4-T5 & caudally spreading to L2-L3 dermatomes. The site of the local anesthetic administration, both in terms of QLM and distance from the costal margin and iliac crest, can affect the height of the block (15).
Although their study did not contain TAB, Edwards et al. discovered that IINB and a transmuscular QLB are equally effective at providing postoperative analgesia following herniorrhaphy (16).
When Yousef compared TAB and QLB in women undergoing total abdominal hysterectomy, the QLB group required less morphine. According to the visual analogue scale, the TAB block group also reported much more discomfort. He discovered that the patients who required analgesia postoperatively were significantly less frequent in the QLB group than in the TAB group having a shorter period of postoperative analgesia (8).
Oksuz et al. compared QLB to TAB in children having orchidopexy or unilateral inguinal hernia surgery. In the first 24 hours after surgery, significantly fewer children in the group of QLB (P < 0.05) needed analgesia (17). This discrepancy can be explained by a single TAB in previous studies as opposed to the severe block performed in our study when TAB and IINB were combined.
Ishio et al. reported similar findings and concluded that the main advantage of QLB was its analgesic efficacy which had similar effects on opioid analgesics without the side effects as vomiting and nausea (18).
In this investigation, several limits must be addressed. Because we were primarily concerned with opioid usage and demand, the block's dermatomal levels were not evaluated. Nevertheless, we do not believe this may compromise the accuracy of our findings, and it may be addressed in future studies. Because some patients required more surgical dissection and manipulation and suffered greater postoperative visceral discomfort than others, the findings could have been skewed by small sample size of the study. Moreover, all the effects of postoperative analgesia may be related to the spinal block or the block; however, both blocks are similar in the analgesic effects to our results; hence, we cannot confirm without explanation. Accordingly, a new study containing a third group taking only spinal anesthesia should be conducted.
TAB/IINB and QLB provide comparable analgesia for hysterectomy patients, with no variation in opioid-related adverse consequences, time until the first dose of oral analgesia, or the overall number of opioids consumed. Accordingly, QLB accelerates postoperative healing and mobilization.