1. Introduction
The celiac plexus block (CPB) is used for motility disorders and chronic pain (1). As it covers visceral pain blocking afferents from the viscera, this block is considered effective and used extensively in cancer pain (2). Particularly in pancreatic cancer pain, CPB is done percutaneously under fluoroscopy, ultrasound or endoscope guidance and also laparoscopically (3-5). But its role is limited in acute postoperative pain management. Though it was used for anaesthesia for laparotomy in 1927, there are limited studies on its use in the intraoperative period for acute postoperative pain management (6-8). When there are no appropriate randomized trials, case reports can be useful to provide a greater insight into interventions to practice evidence-based medicine (9). Transversus abdominis plane (TAP) block has been used as postoperative analgesic technique for somatic pain relief in both upper and lower abdominal surgery (10, 11). To obtain relief from both somatic and visceral pains, there are no reports of combined local anaesthetic (LA) infiltration at Celiac Plexus and continuous TAP block for post-operative analgesia. Therefore, we report its use in two cases.
2. Case Report
A 62- year-old female patient weighing 81 kg presented for gastric bypass. Her co-morbidities were hypertension, type 2 diabetes mellitus, obesity, depression, and many previous uneventful abdominal surgeries. She had spinal injuries resulting in chronic back pain and receiving Pregabilin 75mg BD. For post-operative pain management, she was reluctant to have an epidural although she consented for the TAP block catheters with CPB and Fentanyl (Fentanyl citrate AstraZeneca Pty Ltd NSW Australia) patient-controlled analgesia (PCA).
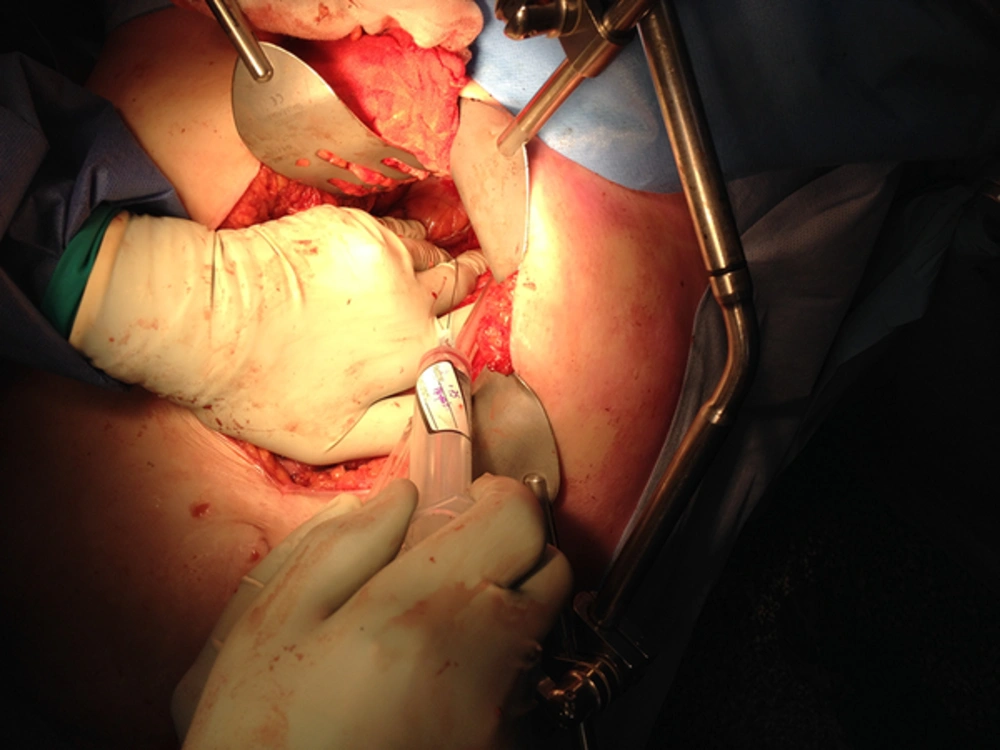
A GA was given with Propofol (Fresofol, Fresenius Kabi, Australia) and Remifentanil (Ultiva, Glaxo SmithKline Australia Pty Ltd. Vic. Australia). Anaesthesia was maintained with Propofol and Remifentanil TCI infusions, O2, air, and Rocuronium. Before closure of abdomen, under direct vision, the surgeon identified and performed the CPB using a 22-gauge spinal needle. At the left crux of the diaphragm, 2 mL Ropivacaine 0.75% (Naropin, AstraZeneca Pty Ltd NSW Australia) was injected followed by 3ml injection at the right crux (Figure 1). There was 15 mmHg fall in blood pressure which did not require any vasopressor.
Ultrasound guided bilateral subcostal TAP was performed postoperatively using an 18 g Touy’s needle followed by catheter insertion. A 20 mL bolus of 0.5% ropivacaine was injected into each side. This was followed by 0.2% ropivacaine infusion at 8ml/hour each side for 48 hours. In the recovery room, the patient did not require any analgesia. However, 8 hours later, she started experiencing sharp pain requiring fentanyl 20mcg bolus and using 700 mcg on day 1 and 680 mcg on day 2. Her dynamic pain scores were 2/10 and 5/10 on day 1 and 2, respectively. Other administered analgesia was Paracetamol 1 gm 6hourly and Pregabalin for the back pain.
The second patient was a 90- year-old man with similar co-morbidities for Whipple’s procedure; he also did not show eagerness for epidural and he had similar GA as mentioned above; but for CPB, 15 mL ropivacaine 0.75% was administered. Post CPB, the patient had 20 mmhg fall in blood pressure although it was uneventful. He had neither dull pain from the viscera nor sharp pain from the incision for 12 hours. His dynamic pain scores were 5/10 on day one and two.
A combination of CPB and TAP block resulted in pain relief for the first 8 to 12 hours negating the use of opioids. This short-term complete pain relief could be due to the local anaesthetic blocking the pain arising from the visceral and somatic at the abdominal wall level. The advantage of CPB is that it is easier to visualise and could be easily performed by the surgeons. The main disadvantages may be hypotension/diarrhoea and inability to visualise the retroperitoneal LA spread. Care must be taken as a case of paraplegia has been reported in an intraoperative CPB (12). The short duration of action was limited by the reduced dosage in the first patient. A continuous CPB could have prolonged the duration of analgesia as demonstrated in one study (8). When conventional options of analgesics are contraindicated, then the combination of CPB and TAP may be useful for post-operative analgesia for laparotomy.
3. Conclusion
The combination of CPB and continuous TAP block improved analgesia and reduced the need for opioids. More studies are needed to evaluate the combination of continuous CPB and TAP infusion in post-operative pain management.