1. Introduction
The Pancoast tumor is a cancer that starts at the top of the lung (at the apex). The most common Pancoast tumors are referred to as adenocarcinomas and belong to the non-small-cell lung cancer group. This type of cancer starts in the mucus glands that line the airways (1). Although superior sulcus tumors do not always appear in this specific location, this term encompasses all tumors in the apices of the lungs and exhibit hallmark clinical signs and symptoms of Pancoast syndrome (2). A Pancoast tumor is characterized by Horner syndrome (constricted pupil, anhidrosis, ptosis, and enophthalmos), atrophy, and pain in the shoulder/arm region due to the involvement of nerves C8, T1, and T2 (3). Local invasion of the tumor is the most common cause of the presenting symptoms. In addition to neurological symptoms (brachial plexus, Horner syndrome), Pancoast tumors may also cause musculoskeletal symptoms (shoulder pain, vertebral or rib pain) (2).
As an interfascial block, the erector spinae plane (ESP) block is used to provide analgesia to patients suffering from chronic thoracic pain. This procedure involves an injection of local anesthetic into the ESP (4). There are numerous indications for ESP blocks, including acute and chronic pain relief and thoracic and abdominal surgery. The use of ESP blocks is continually expanding. The ESP and paravertebral space are proposed sites of the block’s action (5). After the ESP block, profound visceral anesthesia might be caused by local anesthetic diffusion into the paravertebral space (6). Local anesthetics are reported to diffuse through connective tissues and into spinal nerve roots as the mechanism of action (7). A magnetic resonance imaging (MRI) study demonstrated the spread of local anesthetics throughout the foraminal and epidural spaces during the ESP block. It was found that this spread might make ESP blocks superior to other thoracic interfascial plane blocks in terms of abdominal visceral analgesia (8).
According to the obtained results, the ESP block can be used to provide regional analgesia during several surgical operations in the anterior, posterior, and lateral thoracic and abdominal areas, making it suitable for managing chronic and acute pain (9-11). This case report presents a 66-year-old man with a Pancoast tumor and cervicothoracic pain who underwent an ESP block.
2. Case Presentation
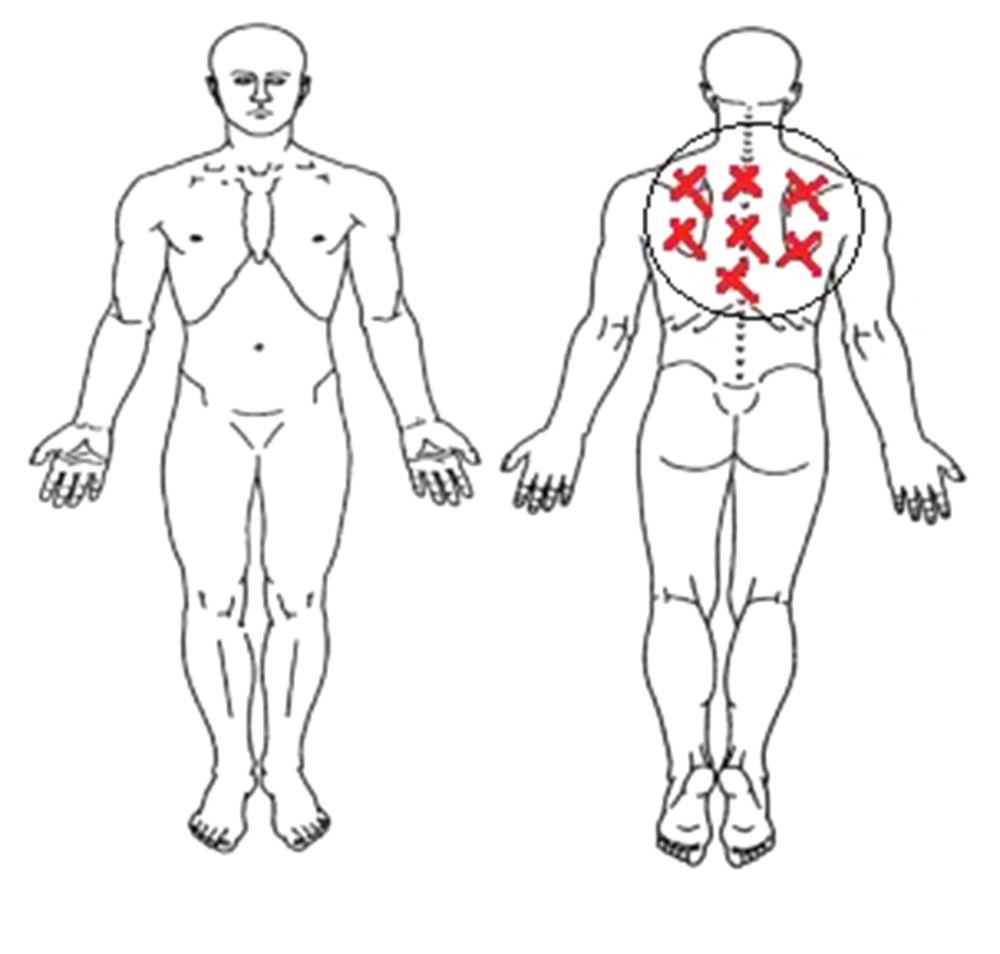
A 66-year-old man with pain in the cervicothoracic junction (neck and thoracic) was admitted to the Post Anesthesia Care Unit (PACU) of Hazrat-e-Rasoole-Akram Hospital, Tehran, Iran (Figure 1). The patient was suffering from a Pancoast tumor (left lung) for two years and had tumors that invaded the spine and involved the thorax parts (T1 and T2). He received 30 sessions of radiotherapy and 16 sessions of chemotherapy. However, the patient’s cervicothoracic pain persisted and was resistant to high-dose drugs, such as opium, oxycodone, and other full-dose drugs. The patient was referred to a pain management specialist. In the first session, the procedures were performed sequentially, with a 20-30-minute interval between the procedures to check the effects. Finally, improvement was achieved by performing the thoracic epidural block for the patient along with a bilateral ESP plane block.
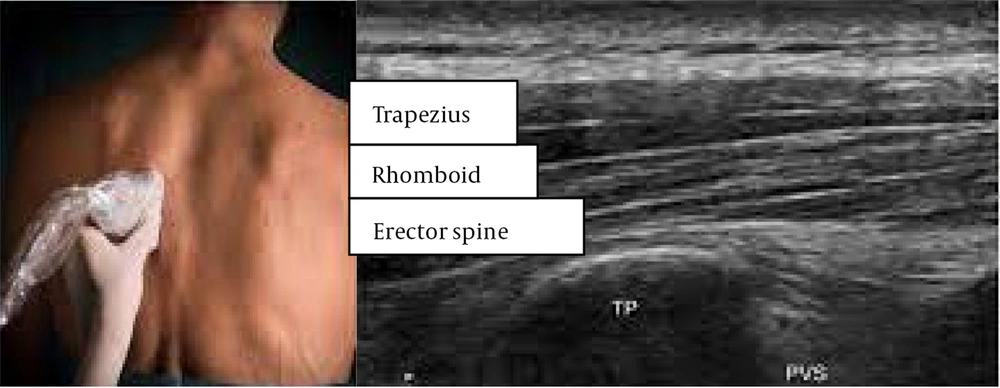
Bilateral ESP plane block (thoracic fascial plane block): The transverse process-rib junction was identified under ultrasound guidance following preparation and draping in a prone position and sterile fashion. Subsequently, 20 cc of ropivacaine 0.2% and 40 mg of triamcinolone were injected into the erector spine muscle. The procedure was also performed for the other side without any complications.
Thoracic epidural block: After obtaining IV access, performing sedation, and preparing and draping the patient in a prone position, a T5-T6 intervertebral space was identified under fluoroscopic guidance. Local anesthesia was then induced with 5 mL of lidocaine 1%. Afterward, epidural Tuohy needle 18G was passed through the T5-T6 intervertebral space using the paramedian approach under fluoroscopic guidance and the loss of resistance technique. The correct position of the tip of the needle was confirmed with 1 mL of non-ionic contrast media (Visipaque, 320 mg/mL), and 3 cc of ropivacaine 0.2% and 80 mg of triamcinolone were injected slowly. The described procedure was performed without any complications.
At the second session (seven days later), the patient’s pain improved by 30% to 40%. The patient was scheduled for the right transforaminal block T2 and T3, bilateral sub-iliocostalis injection, and bilateral ESP block (thoracic fascial plane block).
Right transforaminal block T2 and T3: After preparation and draping in a prone position and applying local anesthesia, (T2-T3) intervertebral space was identified under C-arm guidance and then under oblique (20°) and cephalad (10°) views. A blunt-tipped curved needle (G21-100 mm) was inserted through an introducer (G16) in the tunnel vision (6 o’clock point under the pedicle). The correct position of the tip of the needle was confirmed by injection of 2 mL of the contrast media (Visipaque, 270 mg/mL) under C-arm guidance (AP and lateral views). Afterward, the right transforaminal (T2-T3) epidural block was performed with 4 mL of ropivacaine 0.2% and 20 mg of triamcinolone. The patient was observed for 30 min, and the pain score was not decreased.
Bilateral sub-iliocostalis injection: Thirty minutes later, with the patient in the left lateral position, we placed a high-frequency linear transducer parasagitally at the edge of the scapular spine (4th rib level) and 2 cm from the medial border of the scapula. The bilateral sub-iliocostalis inhection (PSIP) block was performed to identify the lateral boundary of the iliocostalis muscle (ILCM). No significant lateral spread was seen up to the outer border of the ILCM. Injections are superficial to the ribs on the underside of the ribs. After confirmation of the correct needle position, 6 mL of ropivacaine 0.5% and 80 mg of triamcinolone were injected on each side. The procedure was performed for the other side with the same technique without complications. The patient was observed for 30 min and showed no pain reliefs.
Bilateral erector spinae plane block (thoracic fascial plane block): Transverse process-rib junction (T2-T3 level) was identified under ultrasound guidance after preparation and draping in a prone position and sterile fashion. Subsequently, 20 cc of ROPI 0.2% and 5 cc of ozone 30 mics were injected into the erector spine muscle using needle G23 (under ultrasound guidance). The procedure was also conducted for the other side without complications. After this procedure, the patient showed a pain reduction of up to 70 percent.
In the third session (seven days later), the patient had a recovery of more than 50%, eliminating the need for an ESP block (Figure 2).
3. Discussion
Approximately 96% of Pancoast tumor patients report shoulder pain as their first symptom (3, 12, 13). This pain is generally progressive and is probably caused by the invasion of the brachial plexus, pleura, ribs, or vertebrae and may radiate to the head and neck, the axilla, the scapula, the anterior chest, and the arm (weakness in the ulnar nerve distribution and intrinsic muscles of the hand). It is also possible for the tumor to extend into the intervertebral foramina in approximately 5% of patients and cause paraplegia and spinal cord compression (14).
A paravertebral or epidural block is often used to relieve acute or chronic pain after many surgeries, such as cervical, thoracic, or abdominal surgeries (15). Several myofascial blocks and regional techniques have been introduced in recent years, including rectus sheath blocks, transverses abdominis plane blocks, pectoral nerve blocks, quadratus lumborum blocks, intercostals, and interpleural blocks. These methods have indistinct spine anatomical landmarks, and laminectomy makes epidural analgesia difficult. However, ESP blocks can be used for selective multi-dermatomal sensory blockade depending on the surgery type or site of pain. This new method of regional analgesia reduces opioid consumption, and it was found to be convenient and safe (16). The adoption of the ESP block has increased rapidly during the last two years, indicating the effectiveness of this technique. According to a review article by Tsui et al., the single-shot ESP block at the thoracic level seems to be the most frequently operated location in adult patients. In the mentioned study, the authors reviewed 242 cases using the ESP block. The ESP block was used in conjunction with additional analgesic adjuncts in all cases and led to a decrease in the use of opioids. Although sensory variations resulting in reduced cold and sensation of pinprick were described in some studies, several case reports lacked any description of sensory changes. The analgesic benefits of the ESP block can also be attributed to the multimodal analgesia regimen (17).
The ESP block can also be used in situations where conventional therapies have limited effectiveness, such as a lack of identifiable spinal landmarks or the likelihood of epidural analgesia complications related to laminectomy (5). There is an easy way to insert an indwelling catheter in the ESP block due to its sonoanatomy. In contrast to epidural and paravertebral blocks, this procedure needs less expertise and is comparatively simpler and safer, with no procedural complication (10). The procedure eliminates risks of hypotension and epidural spread associated with epidural analgesia, as well as pneumothorax associated with an intercostal nerve block and interpleural block, both of which are procedural complications due to proximity to the spinal cord and pleura (16). The ESP block remains a relatively new technology used limitedly for regional anesthesia. However, the preliminary evidence suggests that it may be an effective alternative to other nerve blocks, such as the paravertebral block. The ESP block has been rapidly adopted due to its simple technique and superficial anatomical landmarks. Before introducing the ESP block, neuraxial and paravertebral blocks were the chosen regional anesthetic methods for posterior thoracic blocks (18). Although effective, paravertebral blocks can contain risks of pneumothorax or subarachnoid injection; they are also technically challenging to perform. The ESP block is a new and simple regional anesthetic method that does not need pneumothorax or subarachnoid injection. It is an attractive alternative to the posterior thoracic block (19). In most studies, the ESP block has been found to be a superior technique to conventional neuroblocks that are performed close to the neuroaxis due to some advantages. First, it is a simple technique to perform since ultrasound is used to visualize the target and direct the needle. In addition, complications have been reported to be rare with this technique. Moreover, critical structures, which can cause serious complications (i.e., major vessel systems, pleura, and medulla), are far from the blockage site (20, 21). Clinical and anatomical studies have shown that the ESP block differs from the retrolaminar block and accidental paravertebral block, although some authors have postulated the opposite (22). Furthermore, it is performed differently, the objective varies in each case, and the diffusion of the local anesthetic differs as well. Catheter insertion is also a simple procedure that can be performed for prolonged analgesia (23).
In their case series, Jain et al. reported the use of T2, T5, and T7 ESP blocks for cervical, thoracic, and lumbar dermatome surgery, respectively (24). Erector spinae plane blocks were successfully used by De Cassai et al. to provide pain relief after laparoscopic surgery (25). Cesur et al. used the ESP block as a pain relief measure after an operation to remove a mass lesion destructing the left fourth and fifth ribs of a 67-year-old male patient and to remove a mass lesion at the level of 8 - 10 ribs from the left hemithorax to the left paravertebral muscles of a 63-year-old female patient (26). Forero et al. also used ESP blocks to treat chronic shoulder pain in an elderly male (10). There is minimal research investigating ESP blocks for chronic cancer pain; however, Ramos et al. successfully treated one case of pleural mesothelioma using this technique (27). Pain control after the ESP catheter placement was excellent in this case report in the case of a patient suffering from chronic pain highly resistant to medication. The ESP block led to more than 50% pain relief in this patient.
The ESP has been the subject of many published case reports, demonstrating that, as an analgesic technique, ESP blocks could be used effectively in a variety of clinical situations. Based on the results of a similar study, high thoracic and low lumbar levels provide adequate analgesia for the upper or lower limbs (17). Analgesia at the thoracic level has been adopted most often for postoperative analgesia. Moreover, it has been reported to have a low complication rate. However, there is a risk of publication bias due to the low evidence, which can be explained by the fact that the studies with negative results might not have been published.
Therefore, the ESP block appears to be an effective analgesic technique that can be used in a variety of clinical settings. Although it might not be the preferred technique in most situations, the ESP block can be a good substitute, particularly in situations where the first-choice technique poses an important risk or is directly contraindicated. Controlled studies should be conducted to compare technical difficulty, efficacy, and patient comfort associated with ESP block and conventional analgesic techniques. In addition, studies should be conducted to evaluate the variability of the sensory dermatomal block associated with injections at different levels of transverse processes, the volume of injectates, and the direction of catheters, as well as the duration of pain relief among chronic pain patients.
3.1. Conclusions
Based on the obtained results, the use of the ESP in this case study resulted in an uneventful, long-term analgesic delivery and improved quality of life in a patient with cervicothoracic junction pain caused by an advanced Pancoast tumor. Further studies are needed to evaluate the safety and effectiveness of continuous blocks in outpatient settings.