1. Introduction
Diphtheria, also known as the ‘strangling angel of children,’ is an infectious disease caused by exotoxin-producing Corynebacterium diphteriae (1). Diphtheria was a leading cause of death in childhood during the prevaccine era, but the cases decreased rapidly upon diphtheria-tetanus-pertussis (DTP) vaccine introduction (2). In 2017, there was a spike in its incidence, with more than eight thousand cases reported worldwide (2). Indonesia also showed the same trend in 2010 - 2017 despite the implementation of the DTP immunization program, with the highest number of cases being 939 children reported in 2017 (3).
Diphtheria causes cell death by inactivating the elongation factor, and the toxin binds to a membrane receptor for cell entry. Diphtheria toxin is usually localized in the upper respiratory tract, entering the mucosa and forming a pseudomembrane. The toxin will also be absorbed into the circulation, causing potential death due to damage to the remote organs (4). Diphtheria is transmitted through respiratory droplets and most commonly infects the upper respiratory tract of children (5). Signs and symptoms usually begin 2 to 5 days after a person becomes infected, characterized by a wing-shaped oropharyngeal pseudomembrane. Fatal airway obstruction may occur if the pseudomembrane dislodges or extends to the larynx or trachea, which could result in sudden death. To this day, airway management in children with diphtheria remains a challenge.
In pediatric difficult airway management, basic principles of airway management, including proper airway assessment, planning, and monitoring, must be achieved (6). In the case of diphtheria, where the patient is difficult to intubate due to pseudomembrane, a tracheostomy can be performed using inhalation anesthesia via face mask or intravenous. The most crucial principle in pediatric difficult airway management is maintaining spontaneous ventilation until the airway is secure. In children without good cooperation, the child must be anesthetized, tailored to the individual situation. The best technique depends on the available equipment and expertise. For inhalation induction, sevoflurane is generally recommended. Intravenous access should be gained before airway instrumentation (6). Orotracheal intubation has been used by many to secure the airway in diphtheria cases. However, the merits and risks of tracheostomy under sedation while maintaining spontaneous ventilation and analgesia using trans-tracheal and superficial cervical block have yet to be confirmed. Here, we present a case of airway management using tracheostomy in a pediatric patient with airway obstruction using a combination of dexmedetomidine, sevoflurane, and analgesia using a combination of trans-tracheal and superficial cervical block.
2. Case Presentation
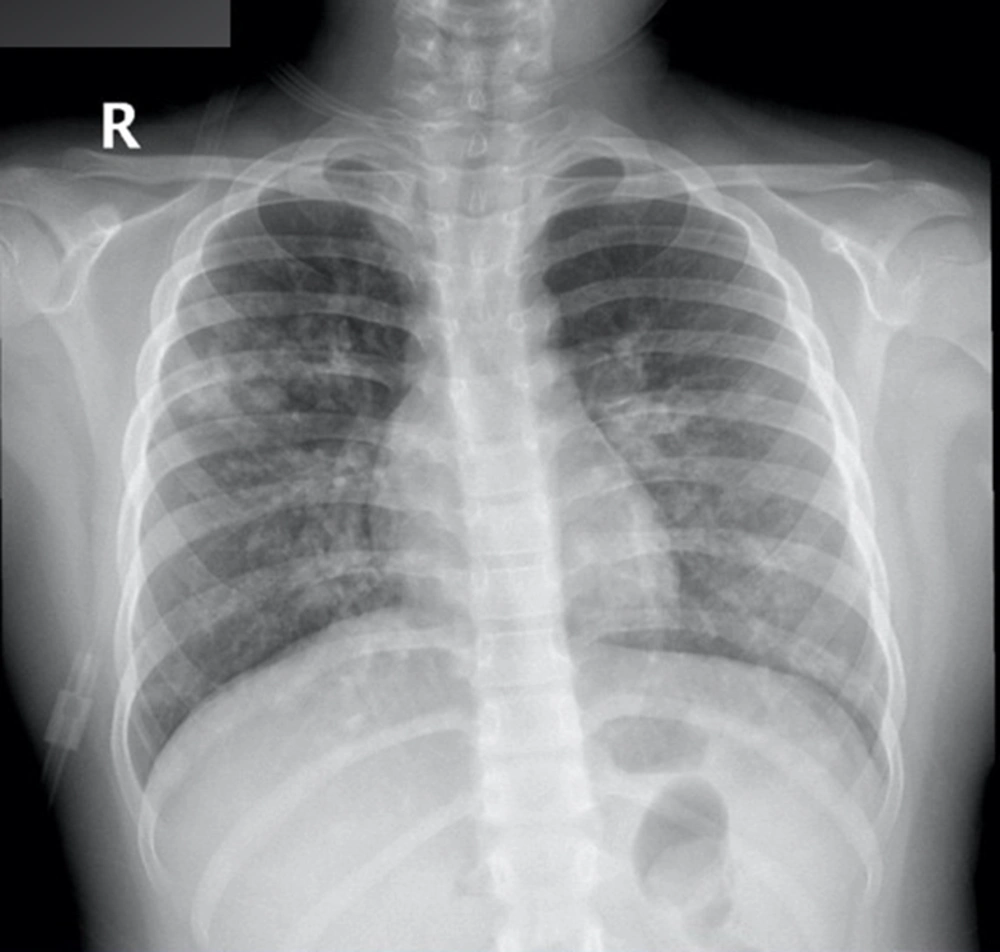
A 6-year-old patient presented to the Universitas Indonesia Hospital emergency room at noon on 4th October 2022 with dyspnea five days before, accompanied by odynophagia and sore throat. The patient also had a fever from the day before. The patient did not receive the nation-regulated mandatory immunizations as an infant. On primary assessment, he exhibited signs of dyspnea with increased work of breathing. Airway examination demonstrated tonsils the size of T4/T4, partially covered with a white-greenish pseudomembrane (Figure 1). Respiratory rate (RR) was 40X/minute with an oxygen saturation of 88% in room air. Physical examination of the chest showed symmetrical breathing with crackles and wheezing heard during auscultation of both the right and left chest. Chest X-ray showed evidence of infiltrations in the middle-lower lobes of both right and left lungs, indicative of pneumonia (Figure 2).
The patient’s saturation was 88% on room air and improved to 98% after being given 8 L/min of oxygen using the simple mask. After Ventolin nebulization, the patient’s shortness of breath improved with a respiratory rate of 24X/minute, but deep inspirations remained. Crackles on auscultation were still heard, but the wheezing had resolved. The patient’s blood test result showed an increase in leukocytes (36.89 × 103/u) and C-reactive protein (CRP) (8.4 mg/L). He was then given 500 mg of intravenous (IV) paracetamol every 8 hours and IV fluid maintenance with KA-EN 3B, a crystalloid solution containing dextrose and potassium (KA-EN 3B, Otsuka). The pediatric, ENT, and anesthesia teams further assessed the patient.
The patient was then scheduled for an emergency tracheostomy at around 2 PM, performed by the ENT specialist. The patient was sedated using dexmedetomidine on an initial titrated dose of 0.5 μg/kg/hour and sevoflurane with a dose of 1 MAC. As for the analgesics, the patient was given a trans-tracheal injection of 3 mL of 2% lidocaine and a bilateral cervical superficial block with 4 mL of 2% lidocaine on both sides. The sedation process was performed by a team of three: one anesthesiologist consultant and two anesthesiology residents. A superficial cervical plexus block was performed using a landmark technique. The needle insertion site was marked from behind the posterior border of the sternocleidomastoid muscle, where the branches of the superficial cervical plexus emerge.
The tube used for tracheostomy was Shiley pediatric tracheostomy tube non-fenestrated type, cannula size 5, inner diameter 5 mm, and outer diameter 7.3 mm. The total time from arrival to the emergency room to the operating room was around 2 hours. After the tracheostomy, the patient’s heart rate was 26X/minute, with an oxygen saturation of 97%. Unfortunately, the patient’s condition deteriorated the next day. On bronchoscopy through tracheostomy, it was found that the pseudomembrane had spread to the carina and mainstem bronchus, obstructing the airway below the tracheostomy (Figure 3). Two days after admission, the patient eventually succumbed to the illness despite antibiotics and treatment in intensive care.
3. Discussion
In this paper, we highlighted the success of airway management through a primary tracheostomy procedure in a pediatric patient with obstructed airway due to diphtheria. The main challenge in airway management of pediatric patients is cooperation and the need to keep the patient still during the procedure.
Previous studies reported that intubation or tracheostomy could be the primary intervention in airway obstruction cases due to diphtheria (7, 8). However, in 2016, Jain et al. reported that tracheostomy was superior to intubation because intubation runs a high risk of pseudomembrane dislodgement (9). Maintenance and toileting for tracheostomy was also easier than intubation, and it had a good prognosis.
In a case series reported by Kin et al., four out of five patients were intubated using video laryngoscope assistance. One patient failed to be intubated and had to undergo a tracheostomy (10). However, no details were mentioned on the analgesia used. Without video laryngoscope intubation, there is a high risk of intubation failure due to pseudomembrane obstruction, airway edema, and bleeding in the pseudomembrane area. Thus, in a medical center with no video laryngoscope, we decided that tracheostomy was superior to direct laryngoscopy.
In this case, the patient presented to the emergency room with respiratory distress, and a thick pseudomembrane was found on examination of the oropharyngeal area. Since using a simple mask was insufficient in improving oxygen saturation, we considered the patient eligible for sedation with maintained spontaneous ventilation during the tracheostomy procedure. When the pseudomembrane has already spread to the plica vocalis, visualization during laryngoscopy would be impaired due to a higher risk of massive bleeding. Therefore, intubation was not the preferred method, and we concluded that the patient could still undergo ventilation. Bronchoscopy later demonstrated that the membrane had already spread to the carina and main bronchus. After consultation with the ENT surgeons, we decided that primary tracheostomy under sedation was the best way to secure the airway.
As mentioned earlier, tracheostomy in pediatric patients can be challenging as it needs patients’ cooperation to keep them stay still. Thus, proper sedation and analgesia are needed. We aimed to sedate the patient while maintaining spontaneous ventilation. Hence, we chose dexmedetomidine and sevoflurane as the sedation agents. Dexmedetomidine was considered beneficial for this situation due to its sedative and analgesic effects with minimal impact on ventilatory function, even in high doses (11). It also has anti-sialagogue properties, which could potentially decrease upper airway secretion and maintain sufficient ventilation (11). Furthermore, sevoflurane also has minimal effect on respiratory depression. Hence, the ventilation could be maintained spontaneously using the combination of sevoflurane and dexmedetomidine.
We preferred not to give the loading dose of dexmedetomidine, considering the risk of hemodynamic instability. To achieve prompt sedation, we used a combination of sevoflurane starting from 1 MAC with a face mask and a maintenance dose of intravenous dexmedetomidine starting from 0.5 μg/kg/hour titrated until the patient was sedated (7). Patient’s ventilation was sufficient using assisted ventilation. It is important to note that the patient was obese, and the oropharyngeal airway was also used to facilitate assisted ventilation.
Besides sedation, we also administered additional analgesia to ensure the patient did not move during painful stimulation and to obviate the need for any increased sedative dose. We performed a 3 mL trans-tracheal injection of lidocaine 2% and bilateral cervical superficial block by anatomical marker using 4 mL of lidocaine 2% on each side. Previous studies demonstrated that a superficial cervical block would be appropriate analgesia for an incision around the neck, including a tracheostomy, and the trans-tracheal injection should give additional analgesia in the intra-tracheal area (8). Compared to a deep cervical plexus block, a superficial cervical plexus block is advantageous due to a lower risk of complications involved in deep cervical plexus blocks, such as nerve root injury, vertebral arterial puncture, and neuraxial spread of local anesthetics (12). Moreover, conventional local infiltration usually has less analgesic effect and needs a large volume of local anesthetic. This may lead to the dissemination of the local anesthetic and cause bilateral recurrent nerve palsy and airway obstruction, worsening the patient’s condition (13, 14). Superficial cervical plexus block can be performed using landmark technique or with ultrasound guidance. We operated using the landmark technique as it is less time-consuming compared to the ultrasound-guided approach. Previous studies have demonstrated that using ultrasound guidance in superficial cervical plexus block has longer effects and does not increase the success rate (15).
The main difficulties faced by the ENT surgeons during tracheostomy were the patient’s obese body, thick fat tissue, and short neck. Fortunately, using a superficial cervical plexus block and trans-tracheal injection, there was no need for increased sevoflurane or dexmedetomidine doses. This provided excellent hemodynamic stability and pain relief. The skin and tracheal incision were successfully performed with minimal patient movement, which resulted in a secured tracheal tube. From skin incision to tube placement, the procedure took 45 minutes without desaturation or hypotension.
In conclusion, this case demonstrated the effectiveness of analgesia sedation for tracheostomy in a pediatric patient with airway obstruction due to diphtheria using sevoflurane and dexmedetomidine in combination with spontaneous assisted ventilation for the tracheostomy procedure. Superficial cervical plexus block provides more comfortable and can secure patient cooperation, especially in pediatric patients with poor cooperation. Additionally, the combination of trans-tracheal and superficial cervical block proved to be excellent analgesia, and it can be used in emergency tracheostomy to secure the airway. This case also highlights the need to be vigilant in facing rapidly progressing and lethal airway obstruction due to diphtheria in children.