1. Context
Global statistics show an increase in the prevalence of chronic diseases (1, 2), such as cerebrovascular accidents (CVA) (3, 4). The most common and debilitating neurological lesion in adults is CVA, known as the third cause of death after cancer and cardiovascular diseases (5, 6). Also, CVA is one of the upper motor neuron diseases, characterized by non-coordination in the normal movement pattern, and hemiplegia is considered one of the symptoms of neurovascular diseases of the brain (7-9). The length of stay and the complications of CVA are effective in managing and planning costs, resources, facilities, and the healthcare system (10). The prevalence of CVA-related complications is reported to be about 40 - 96%, and pain is one of the most common complications of CVA (19% - 74%) (11). Different types of CVA complications, including infections, deep vein thrombosis, and pain, have been reported, which can lead to death (12). Besides, CVA-related pain includes central pain, headache, spinal nerve pain, muscle pain, and hemiplegic shoulder pain (13, 14).
Hemiplegic shoulder pain (HSP) is the most common CVA-related complication that forces the patient to use other organs to compensate for the resulting disability or reduce the patient's quality of life by putting pressure on the damaged organ (5, 15). Also, HSP may become more painful due to joint immobility, muscle weakness, and soft tissue changes that occur after a stroke, negatively affecting all aspects of the patient's life (16). Several factors, such as paralysis, sensory disorders, spasticity, limited range of motion in the shoulder, and shoulder capsulitis, are involved in the development and aggravation of HSP, and effective steps can be taken to prevent HSP by identifying the above risk factors (17, 18).
Pain is an unpleasant experience that must be mitigated by taking preventive and therapeutic measures (19-21). One of these measures is to identify the prevalence of pain related to the anatomical parts of the body in different patients, and appropriate interventions can be performed accordingly (22-24). We can use oral or injectable pain medications (25) or physiotherapy (26) to reduce HSP. The subsequent disorders and disabilities are a big challenge to medical and nursing care in the hospital and at home. Families must also take care of CVA patients and undergo elevated stress levels. For this reason, it is a priority to identify the prevalence of the above disorders and disabilities and take necessary measures to improve or mitigate them (27, 28).
2. Objectives
Considering the importance of chronic diseases, the present meta-analysis study aimed to determine the HSP prevalence in CVA patients.
3. Methods
This meta-analysis study searched English and Persian descriptive or descriptive-analytical full-text studies on CVA patients. Review articles, case reports, intervention studies, and letters-to-the editors were excluded.
The search was carried out in all databases by two researchers with scientific and practical mastery of CVA, pain, and orthopedic diseases. In addition to the above databases, the references of all the above articles that entered the final stage were investigated by both researchers. Keywords such as stroke, pain, CVA, hemiplegic, hemiplegic shoulder pain, and shoulder pain were used for searching. Data analysis was done with the software CMA3.
4. Results and Discussion
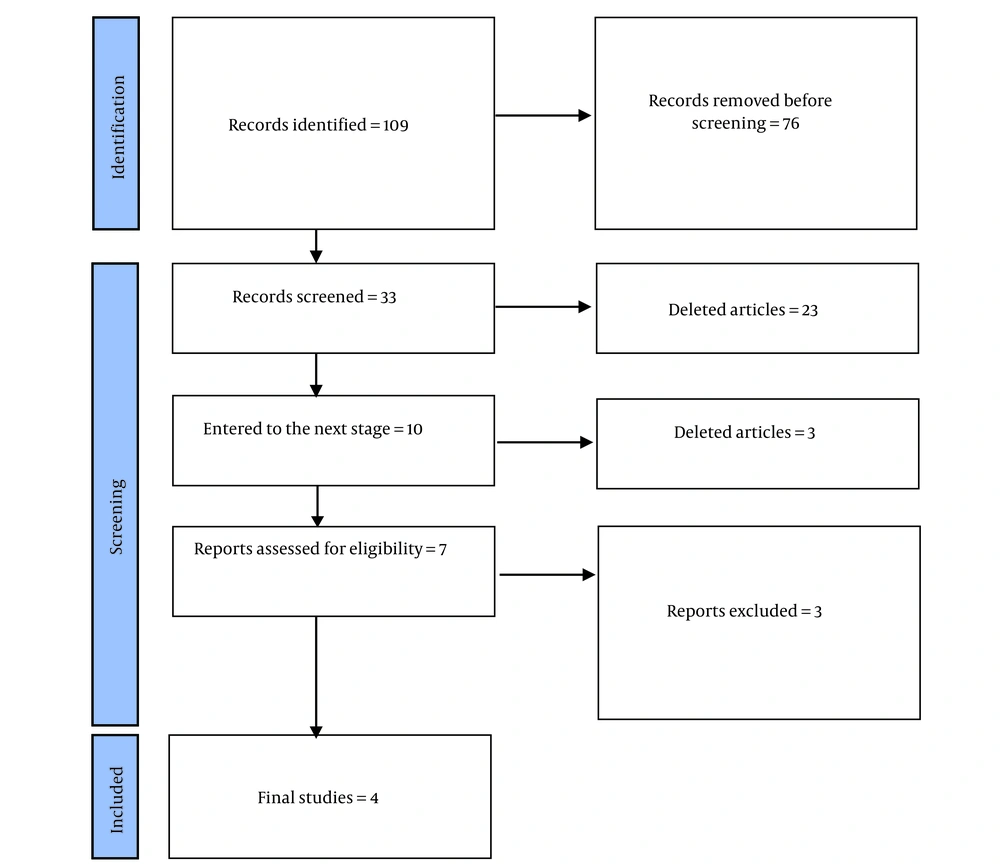
In the initial search, 109 articles were found, and finally, the data from four articles were analyzed (Figure 1). The lowest prevalence was 7.2% in the study of Ghayeghran et al. (29), and the highest rate was 34% in the study of Ghahremani et al. (30) (Table 1).
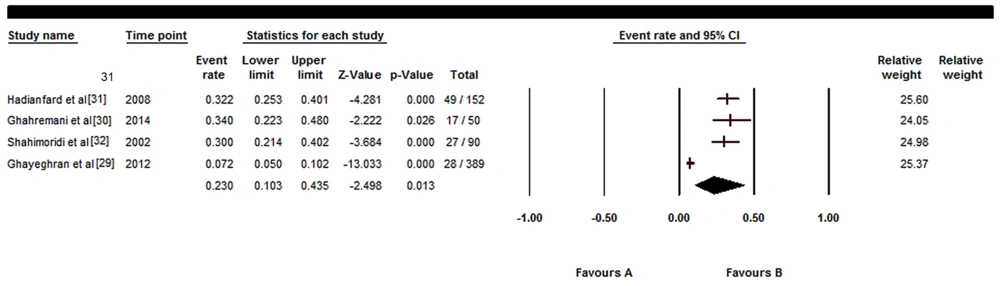
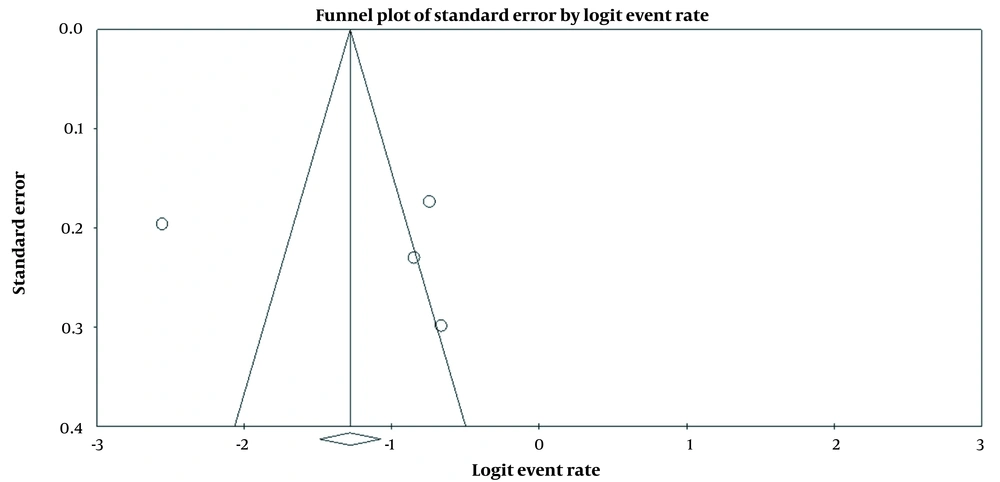
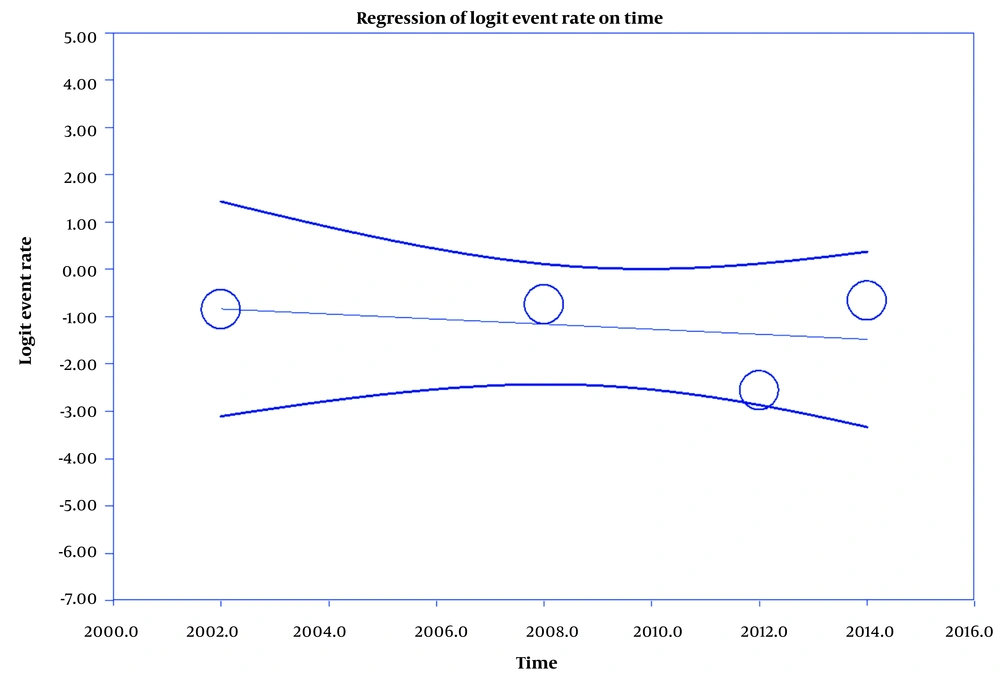
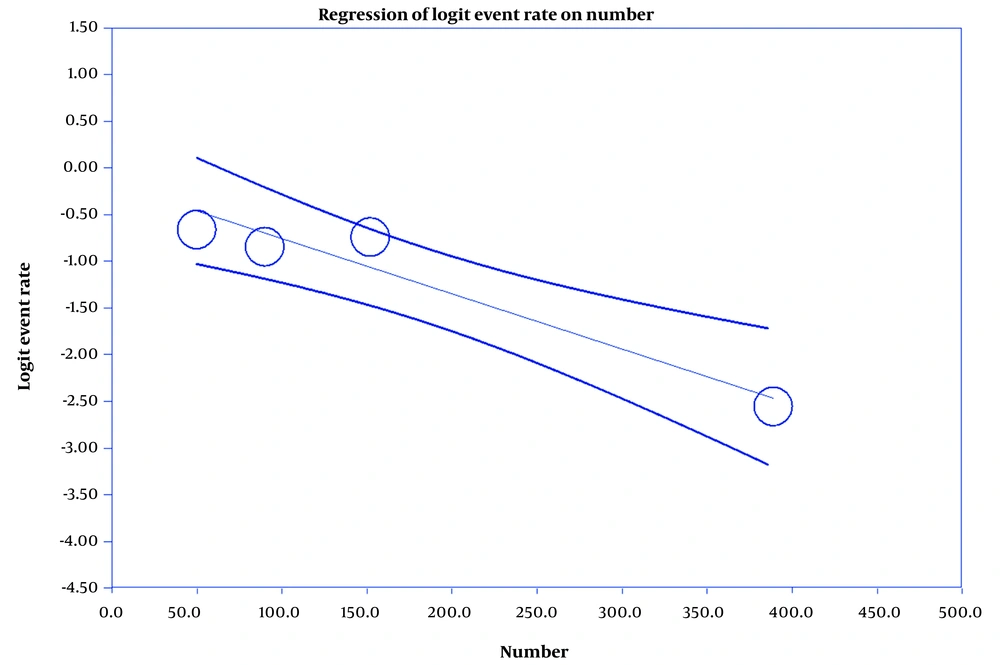
The results showed that the prevalence of HSP was 23% (confidence interval (CI) = 10.3% - 43.5%) (Figure 2). Figure 3 shows the final plot of the studies, and Figures 4 and 5 indicate the relationships between the prevalence of HSP and the time of conducting studies and sample size.
A meta-analysis study was conducted on the prevalence of HSP among Iranian CVA patients. The prevalence of HSP was 23% (CI = 10.3% - 43.5%). Hatefi et al. studied 200 patients with confirmed CVA and showed that the mean scores ± SD of lifestyle and pain were 21.83 ± 3.91 and 16.22 ± 1.99 (33). Pouy et al. also showed that the mean score ± SD of the patient's lifestyle was 118.20 ± 6.00 (34). In a meta-analysis study, Holmes et al. identified 54 risk factors for shoulder pain after CVA, including reduced motor function in the upper limb, type of CVA, diabetes, gender, and previous history of shoulder pain (35). In a review of 21 articles, Kumar et al. also referred to glenohumeral subluxation, reduced function, and range of motion in the shoulder as HSP risk factors (36).
Various studies investigated the prevalence of myofascial trigger points (MTrPs) in patients with HSP. For example, Villafane et al. investigated 50 CVA patients who had HSP and found that the prevalence of MTrPs was 40% - 68% (37). Menoux et al. and Paolucci et al. also stated that the HSP prevalence was 8% - 13% and 29.56%, respectively (38, 39).
Various studies have been conducted on the HSP prevalence in different patients and study populations. For example, Luime et al. found that the HSP prevalence in 18 articles in the general population was 0.9% - 2.5% (40). Similarly, Tessaro et al. found that the HSP prevalence among Italian teenagers was 51% (41). In a study on individuals aged 58.7 to 76 years, Anwer and Alghadir found that the HSP prevalence was 10% - 12%. Other risk factors and predictors of HSP include female fertility, sensory disorders, age, hemorrhagic stroke, and medical history of previous chronic disease (42).
5. Conclusions
Considering the HSP prevalence (23%) among CVA patients, it is necessary to carry out rehabilitation interventions to prevent such pain in these patients. It is also suggested that rehabilitation interventions be included in the patient education of the healthcare system.