1. Context
Prescription opioid use has become an epidemic in the United States (1, 2). Nonetheless, the use of opioid analgesics to treat acute, postoperative pain is a well-established practice included in pain management guidelines (3). There is a lack of evidence to support the effectiveness of long-term opioid therapy in patients with chronic, noncancer pain (4). Despite this, opioids are the most commonly prescribed drug to treat chronic back pain (5).
Many patients undergoing spinal surgery have trialed opioids before surgery for conservative pain management. For example, in a cohort of 34,186 patients presenting for surgery, those undergoing spinal or spinal cord surgery reported the most preoperative opioid use (57.1%) (6). A separate insurance database analysis found 57.8% of patients undergoing lumbar spinal fusion had a history of preoperative opioid use (7). Unfortunately, preoperative opioid use has been shown repeatedly in the literature to negatively affect spinal surgery outcomes (8).
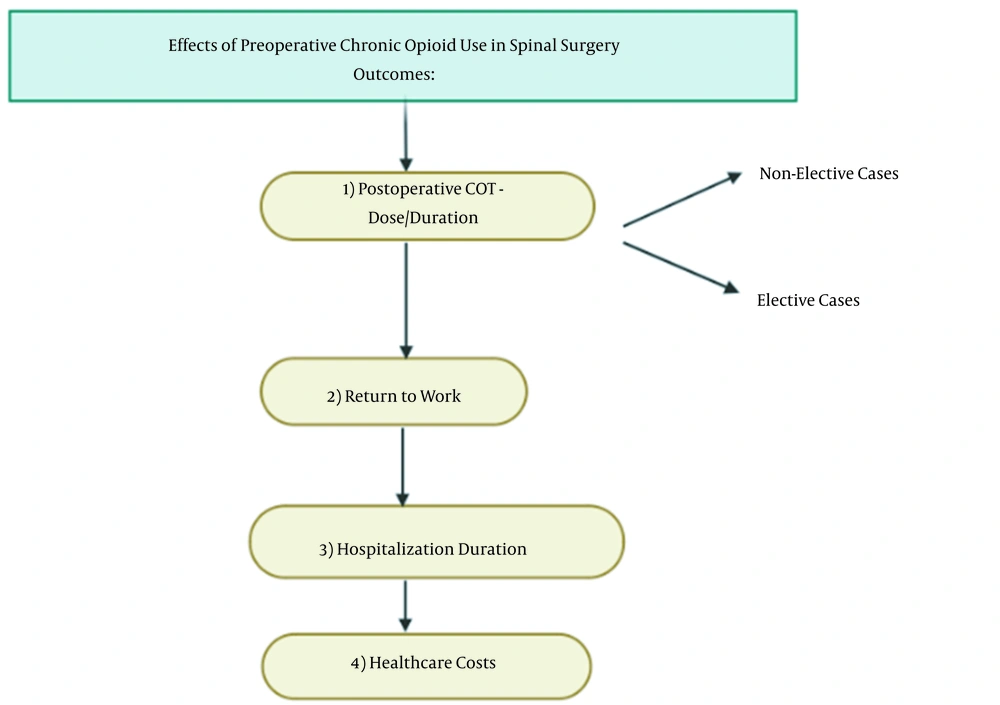
This article provides a narrative review of the available literature on preoperative opioid use and its influence on postoperative outcomes following spinal surgery. Figure 1 illustrates a flow diagram which defines the structure of this review where COT is defined as chronic opioid therapy. We aim to highlight and summarize the main postoperative associations with preoperative opioid use that have been found in previously published studies, specifically (1) increased postoperative chronic opioid use; (2) decreased return to work (RTW) rates; (3) increased length of hospital stay (LOS); and (4) increased healthcare costs.
2. Data Sources
This was a narrative review. The sources for this review are as follows: Searching on PubMed, Google Scholar, Medline, and ScienceDirect; using keywords: Opioid Dependency, Postoperative, spinal surgery
3. Postoperative Chronic Opioid Therapy
3.1. Lumbar
Postoperative chronic opioid therapy (COT) was the most frequent outcome measured across studies that examine preoperative opioid usage in spinal surgery. Specifically, 24 studies identified in the literature analyze the association between preoperative opioid use and COT (8-31). Twelve studies reviewed this association in spinal surgery of the lumbar region (9-12, 20, 25-31). In a retrospective cohort of patients undergoing lumbar fusion surgery in the workers’ compensation (WC) setting, a higher preoperative opioid load and duration of use was associated with increased rates of postoperative COT (9). The strongest predictor of postoperative COT (greater than 1 year after the 6-week acute postoperative period) was preoperative COT, in which 79.6% of patients receiving opioid therapy before surgery were found to be on COT after surgery. Bohl et al. retrospectively analyzed patients undergoing lumbar interbody fusion (20). They found a 2.2 times greater risk of continued opioid use at the second postoperative visit in patients who were using opioids before surgery. These results suggest patients with preoperative opioid usage may require additional counseling or supervision regarding COT in the postoperative period.
Another study in adults who underwent lumbar spinal fusion surgery found preoperative opioid use to be the strongest predictor of COT (25). This study used one of the nation’s largest commercial insurance databases, making it the first to investigate this association in a nationally representative sample of lumbar fusion patients. A similar study using commercial insurance data included patients who underwent the posterior lumbar fusion (PLF) (26). Twenty-two percent of patients in this cohort had documented opioid usage > 6 months preoperatively, while 87.4% were documented to use COT postoperatively. Those on preoperative COT were more likely to document postoperative persistent COT, as well as receive steroid epidural and facet injections and undergo repeat lumbar surgery. Adogwa et al. used another insurance company database to retrospectively analyze patients who underwent 1, 2, or 3-level index lumbar decompression and fusion (27). Aside from observing female sex was independently associated with prolonged opioid use after surgery, opioid usage at least 6 months preoperatively was associated with increased prolonged (> 1 year) opioid use (OR: 3.43).
Kalakoti et al. studied patients undergoing lumbar interbody fusion (28, 32). At one year postoperatively, significantly more patients who were using opioids before surgery had filled an opioid prescription compared to those who were opioid naïve before surgery. Consistent with other studies, preoperative opioid use was the strongest predictor of 1-year postoperative COT, regardless of the surgery performed.
Oregon’s prescription drug monitoring program was used to retrospectively quantify preoperative and postoperative opioid use in adults undergoing lumbar fusion surgery (29). The authors found cumulative preoperative opioid dose to be the strongest independent predictor of long-term postoperative opioid use (OR: 15.47), consistent with previous studies. These results indicate lumbar fusion surgery rarely eliminates opioid usage in those who have been on COT, while also placing opioid-naïve patients at risk for developing chronic opioid use.
Another TRICARE insurance claim study analyzed patients who underwent lumbar surgery (30). Most patients who were using opioids before spinal surgery discontinued their opioids postoperatively; 67.1% had discontinued opioid usage by 30 days and 86.4% discontinued use by 90 days. However, among the 8.8% that continued opioid use beyond 90 days postoperatively, the duration of preoperative opioid use was the greatest predictor. A dose-response effect was even observed for preoperative opioid use on postoperative cessation.
Another retrospective review of patients undergoing surgery for lumbar spondylolisthesis used the MarketScan database to identify what factors influenced postoperative opioid dependence (31). Among all the variables analyzed, prior opioid dependence was the strongest independent predictor of postoperative opioid dependence (OR 16.29), while the type of surgery had no impact. However, the results from this study indicate that those who undergo surgery for degenerative spondylolisthesis were two times as likely to be opioid independent as they were to become opioid dependent.
Lall and Restrepo was the only article to perform a prospective, longitudinal study to determine what factors affected the length of opioid cessation following lumbar fusion surgery (10). The preoperative opioid use was the only significant positive predictor of weeks to opioid cessation postoperatively. They suggest nurses can use this data to identify patients at risk for postoperative COT by screening for preoperative opioid use.
Two studies examined preoperative opioid use in lumbar discectomy (LD) procedures (11, 12). The first retrospective cohort of WC patients undergoing LD found long-term COT associated with increased rate of postoperative opioid use and for a longer duration (11). Qureshi et al. also conducted a retrospective analysis of 1,321 patients undergoing LD; however, this data was pulled from a commercial healthcare database and was not restricted to the WC population (12). Unsurprisingly, preoperative opioid use increased the odds of long-term opioid prescription (> 3 months postoperatively) by more than 3 times. As compared to major spine procedures, discectomies are relatively benign procedures that can typically be performed in an outpatient setting; thus, these results indicating long-term opioid usage following LDs indicate other factors contribute beyond surgical pain management (32).
3.2. Cervical
Cervical spinal surgery patients are another population with a propensity for preoperative opioid use. Five studies analyze the association between preoperative opioid use and postoperative COT in this population (8, 13-15, 28). A review by Lawrence et al. of patients undergoing cervical arthrodesis found chronic COT, defined as greater than 6 months before surgery, associated with continued opioid use following surgery (8). Consequently, the authors argue the Robinson et al. criteria—a measurement used to evaluate clinical outcomes of cervical spine surgery—should be modified to account for preoperative narcotic use (33).
Recently, Jain et al. conducted a review of Humana commercial insurance data including patients undergoing primary cervical fusion (13). Preoperative opioid use for at least 6 months was associated with a 4.72 odds ratio (OR) of opioid use at least 1-year postoperatively. These outcomes indicate unrelieved pain from surgery in patients who are chronic opioid users, further supporting the outcomes shown by Lawrence et al. (8). The results from Jain et al. (13) also show that cessation of opioids for at least 6-weeks before surgery or restriction of preoperative opioid use within 3 months before surgery can significantly reduce the risk of postoperative complications.
In another study analyzing patients who underwent cervical fusions, over 50% of patients reported using opioids preoperatively (28). The rates of opioid use fell dramatically at 3-months postoperatively in those who did not use opioid preoperatively; however, 45.3% of those who used opioids preoperatively were observed to remain on opioids at 1-year postoperatively. These findings are consistent with outcomes from other studies, indicating that cessation of opioid use should be encouraged before cervical spinal surgery.
A separate study of patients undergoing cervical spine arthrodesis found preoperative COT—defined by opioid prescription filling within 3 months preoperatively—to be associated with prolonged opioid use at 3 months (OR: 1.30), 1 year (OR: 5.17), and 2 years postoperatively (OR: 5.75) (14). In agreement with previous authors, these researchers suggest the development of a multi-disciplinary preoperative opioid weaning protocol to minimize the risk of postoperative COT and optimize outcomes and patient safety.
Karhade et al. performed a study including cervical fusion patients to develop machine learning algorithms to help predict sustained postoperative opioid usage in this patient population (15). Preoperative opioid use duration was one of the most important predictors of sustained postoperative use. The authors have made their online web application available to help clinicians identify patients who might benefit from multidisciplinary interventions from areas like social work, mental health, and pain medicine.
3.3. Other
An additional studies were identified that used pooled data from different types of spine surgery, all of which reported preoperative opioid use associated with increased postoperative chronic opioid use (16-19). A prospective cohort of patients undergoing elective spine surgery were enrolled by Armaghani et al (16). The authors found increased immediate postoperative opioid demand in the PACU and decreased opioid independence at 1-year postoperatively in those patients who reported greater preoperative opioid use. Interestingly, in patients taking opioids preoperatively, those predisposed to depression were more likely to continue opioid usage at 1-year postoperatively than those not predisposed to depression. This finding highlights the effect psychological conditions have on postoperative opioid use as psychiatric diagnoses in those using preoperative opioids were predictors of continued use at 12 months (16). Additional factors such as age, degree of surgery invasiveness, and anxiety were significantly associated with increased intraoperative opioid demand. However only the invasiveness of the surgery, anxiety, revision surgery, and greater preoperative opioid use were significantly associated with decreased incidence of opioid independence at 12 months postoperatively (16). Another study following patients undergoing elective spine surgery found 21% of patients using preoperative opioids (17). In addition to reporting less improvements following surgery, both preoperative COT and high-preoperative dosage were independently associated with postoperative COT. This study is the first to analyze preoperative opioid dosage. Given these results, the authors argue opioid weaning protocols before spine surgery have the potential to significantly increase postoperative outcomes and decrease the risk of COT.
Dunn et al. conducted another study of patients who scheduled for elective major spine surgery, of which 72.3% used opioids preoperatively (18). The results showed that preoperative opioid users were almost 4 times more likely to use opioids at 1-year postoperatively than those who did not use opioids preoperatively. This study also assessed intraoperative intravenous ketamine or lidocaine; however, these interventions did not show any decrease in COT at 1-year postoperatively. These results were in contrast to previously published studies reporting decrease postoperative opioid use in those who received intraoperative ketamine (34, 35).
A separate study used the Illinois Prescription Monitoring Program to query patients who had spine surgery (19). Similar to prior results from other studies, the authors found the use of opioids at least 6 months preoperatively was the strongest risk factor for continued usage and at higher doses 6 months postoperatively, even more so than the number of spinal levels fused. This study's novel use of a state-run prescription dispensation database likely provides more accuracy than other studies that rely on self-reported opioid usage.
Cook et al. conducted a study of patients undergoing spinal surgey (21). The results indicated that only 15% to 18% of preoperative opioid naïve patients continued to fill prescriptions at 1 year postoperatively, while 50% to 64% of preoperative chronic users continued to fill prescriptions. Additionally, this was the first study to report the average size of opioid prescriptions, in which preoperative chronic opioid users obtained more pills postoperatively than preoperative opioid naïve patients (127 - 152.5 mg oxycodone equivalent pills vs. 76 - 91 mg).
To examine the accuracy of patient self-reporting, Ahn et al. compared the postoperative opioid consumption between preoperative opioid users who accurately self-report and those who do not accurately self-report preoperative opioid usage (22). Their self-reported preoperative opioid usage responses were confirmed with data from the Illinois Prescription Monitoring Program (ILPMP). Contrary to findings from previous studies, patients who used opioids preoperatively were no more or less likely to be dependent on opioid medications at the first or second postoperative visit; however, these results were not statistically significant. Interestingly, postoperative opioid consumption was independent of the self-reported accuracy of preoperative consumption.
3.4. Scoliosis
Sharma et al. analyzed this association in adult with degenerative scoliosis undergoing decompression and fusion (23). The researchers used the national MarketScan database to analyze patients and determine what factors were associated with postoperative opioid dependence, defined as continued opioid use or greater than 10 opioid prescriptions filled between 3 and 15 months postoperatively. Interestingly, there was no increased likelihood of opioid dependence following surgery to repair adult degenerative scoliosis; however, patients who were regularly on COT preoperatively were more likely to remain on COT postoperatively than those who were opioid independent before surgery. These results indicate close clinical follow-up is encouraged in those patients who were opioid dependent before surgery.
Yang and Werner studied risk factors associated with postoperative COT in the adolescent idiopathic scoliosis population undergoing posterior spinal fusion (24). In this study, preoperative opioid use was the most significant predictor of prolonged postoperative opioid use (OR: 2.93). The authors hypothesize this association may result from preoperative opioid users having poorer pain coping abilities or higher preoperative pain levels. Patients undergoing fusion of 13 or more spinal levels were also more likely to report prolonged opioid use.
4. Return to Work
4.1. Lumbar
Return to work status is a common validated measurement utilized in WC patients to assess successful improvement following spinal surgery (9, 36). Following rates of postoperative COT, RTW was the second most common outcome reported in studies assessing the effects of preoperative opioid use. Some studies reported RTW status, all of which examined the WC patient population and showed a negative effect of preoperative opioid use on RTW (9, 11, 36-41). Anderson et al.’s study described earlier that showed preoperative opioid use was associated with postoperative COT also found RTW to be negatively associated with postoperative COT (OR: 0.38), in which only 11.0% of the postoperative COT group returned to work (9). These poor outcomes suggest there may be a limited role for discogenic fusion as a treatment for degenerative disk disease (DDD) in WC patients. A similar study in patients undergoing lumbar fusion for DDD reinforced these findings and found prolonged preoperative opioid use to be a strong negative predictor of RTW, with only 11.9% of these patients returning to work (36). The strong negative predictive value of preoperative COT followed behind only two other factors, a preoperative psychiatric disorder and prolonged time out of work. Similarly in another study, long-term preoperative opioid use was found to be a strong negative predictor for postoperative RTW status in WC patients undergoing lumbar fusion for spondylolisthesis (37).
O’Donnell et al. determined preoperative opioid use to be an independent negative predictor of RTW rates (OR: 0.54) (11). A significant difference in RTW rates were identified between the no preoperative opioid use group (64.1%), moderate preoperative opioid use group (52.7%), and long-term preoperative opioid use group (36.7%). These findings highlight the importance of identifying patients preoperatively on long-term opioid therapy to predict those at risk for not returning to work.
A cohort study of WC patients found a significantly higher RTW rate in patient who were on opioids less than 3 months preoperatively (42%) as compared to those who used opioids for greater than 3 months preoperatively (23%) (38). Duration of preoperative opioid usage was a significant negative predictor of RTW. The researchers argue that a shorter course of opioids and earlier initiation of surgical intervention may improve clinical outcomes in this patient population.
4.2. Cervical
Furthermore, three additional studies found a negative association between preoperative opioid use and RTW status following cervical spine surgery (39-41). A retrospective cohort comparative study was performed to evaluate presurgical factors that affect RTW status after multilevel cervical fusion in patients with work-related injuries (39). Like the findings from lumbar studies, preoperative opioid use negatively affected RTW status within three years postoperatively. A separate study investigated similar outcomes after only single-level cervical fusion cases for radiculopathy in the same population (40). Unsurprisingly, prolonged preoperative opioid use was also a significant negative predictor of RTW status (OR: 0.73). As a result, the authors suggest a shorter course of preoperative opioid use and earlier surgical intervention may provide RTW status benefits in WC patients undergoing cervical fusion. Preoperative opioid use as a negative predictive factor for RTW status was additionally supported in a separate study analyzing again patients undergoing single-level cervical fusion for radiculopathy in the Ohio WC population (41).
5. Hospitalization Duration
Length of hospital stay is another metric used to measure recovery following spine surgery. Some studies were identified that measured duration of hospital stay following spine surgery. Siemionow et al. performed an analysis of patients undergoing minimally invasive (MIS) TLIF to assess what parameters predict LOS (42). Contrary to the authors’ hypothesis, preoperative opioid use was associated with a shorter LOS. It is believed that this results from the “protective” effect of preoperative oral opioid use on the nociceptive pathway which reduces nociceptive transmission from the procedure. Haws et al. conducted another similar study on patients undergoing MIS TLIF, finding preoperative opioid use to not be associated with an increased risk of longer LOS (43). Although, preoperative opioid use was independently associated with increased postoperative pain. Walid et al. studied patients who underwent different spinal surgery procedures and found the same paradoxical relationship in those patients undergoing lumbar microdiscectomy (44). Preoperative opioid use was associated with shorter LOS and less hospital charges in those undergoing microdiscectomies. The authors suggest this finding may be due to an opioid-restrictive pain regimen in the hospital given the minimally invasive nature of the surgery, which may not be compatible with the desire for opioids in chronic users.
Conversely, a larger retrospective cohort of adults undergoing elective lumbar fusion found preoperative opioid dependence associated with a 2.11 times higher odds of a prolonged LOS, even when surgical complications are controlled for (5). The authors argue this negative association is likely due to challenges in perioperative pain control in opioid-dependent patients, which have been well documented in the literature.
Martini et al. also performed a study of patients undergoing different lumbar fusion procedures to examine how recovery is affected in those specific patients with opioid use disorders (45). It was determined that patients with concurrent opioid use disorders had longer LOS, independent of other factors. Consequently, the authors argue patients with opioid use disorders are challenging to treat effectively with traditional enhanced recovery after surgery (ERAS) protocols. Thus, personalized ERAS protocols should be developed for this patient population to account for their unique risk profile during hospitalization.
Armaghani et al. analyzed patients undergoing spinal surgery for a structural lesion to assess this relationship (46). Consistent with previous studies, the data showed an association between preoperative opioid use and increased LOS, specifically a 1.1-day extension for every 100 mg morphine equivalents the patient consumes preoperatively. Interestingly, this association was still observed when invasiveness of the surgical procedure was controlled for. The researchers hypothesize this association is secondary to the challenge of controlling postoperative pain in chronic opioid users, resulting in delayed mobilization and discharge milestones. Similarly, Cozowicz et al. reviewed the data from an additional spine fusions and found a stepwise increase in LOS with low to medium to high preoperative opioid prescriptions, with high preoperative opioid prescription being associated with a 22% increase in LOS (47).
Another review by Madineni et al. examined if the association between preoperative opioid dosage and LOS is similar in patients who underwent thoracic spinal cord stimulator placement surgery (48). The results from 47 patients showed that patients on high-dose COT (greater than 100 mg morphine equivalent dose) tended to have an increased LOS compared to patients on lower-dose opioid therapy. A separate review by Raad et al. sought to examine this relationship in adult patients undergoing spinal deformity surgery (49). The results showed daily preoperative opioid usage independently increased duration of hospital stay (OR: 1.7). Daily opioid usage was also independently associated with an increased ICU stay (by 16 hours), the first time this has been reported in the literature. This finding is likely explained by the higher risks of postoperative delirium, respiratory depression, longer respiratory rehabilitation, and pneumonia observed in preoperative daily opioid users.
6. Healthcare Costs
Chronic back pain is a common problem that has placed a high cost on the healthcare (50-52). The impact of preoperative opioid usage on healthcare costs is another metric commonly explored in these studies. Some studies already identified earlier in this review also performed a cost analysis, and found higher healthcare costs associated with preoperative opioid use. Walid et al.’s review of spinal surgery patients was the only one of these that found preoperative opioid use to be associated with less hospital charges in those patients who underwent lumbar microdiscectomies (44). This effect is likely due to the shorter LOS resulting from opioid-restricting pain regimens in the hospital, which may encourage opioid users to be discharged earlier.
A review of WC patients undergoing lumbar decompression found patients on opioid therapy greater than 3 months preoperatively (compared with less than 3 months) cost the Ohio Bureau of Workers’ Compensation more than $70,979 (38). Similarly, O’Donnell et al. analyzed WC patients who underwent lumbar discectomy and found long-term preoperative opioid use to be associated with $64,635 greater in medical costs than those with no preoperative opioid use (11).
In Cozowicz et al.’s study of spinal fusions, the risk for increased healthcare costs was 76% in patients who reported high preoperative opioid prescriptions (47). Additionally, healthcare costs significantly increased by 14% in patients who reported high preoperative opioid prescriptions compared to those who reported low preoperative opioid prescriptions. The authors hypothesize these findings result from higher postoperative complications requiring additional treatments and hospital resources. The review by Jain et al. on patients undergoing spinal fusion also found an association between preoperative COT and healthcare costs, likely due to increased rate of readmission, epidural and facet joint injections, and revision fusion (26). This increased utilization of healthcare resources suggests a lack of improvement in pain following fusion surgery in chronic opioid users. Tank et al.’s review of lumbar fusions were consistent with previous studies and showed the same association (5). The mean hospital cost of opioid-dependent patients was $35,827 compared to $29,349 in non-opioid-dependent cohort.
Martini et al. reviewed patients with an opioid use disorder undergoing lumbar fusion and found this condition to be independently associated with greater total hospital charges (45). The researchers believe it’s imperative to create individualized ERAS protocols for this subset of the population undergoing spine surgery to improve patient care and reduce cost burden.
Preoperative opioid use also affected healthcare costs following cervical spinal fusion. Jain et al.’s cohort of patients undergoing primary cervical fusion found an additional cost ranging from $623 - $27,360 per patient for those on preoperative COT (13). The increases cost is believed to be secondary to the increased use of resources, such as medication, ED visits, constipation, injections and revision fusion in the postoperative period. The retrospective review of WC patients undergoing cervical fusion by Faour et al. also demonstrated an association between prolonged preoperative opioid use and higher net medical costs (40).
7. Conclusions
The literature has general consensus that preoperative opioid use leads to poorer outcomes following spinal surgery. The present investigation highlights some common themes identified in this patient population. Namely, preoperative opioid exposure in patients undergoing spinal surgery is associated with increased risk of postoperative COT, decreased RTW rates, increased length of hospitalization, and increased healthcare costs. As previously mentioned, this study is the first to analyze preoperative opioid dosage and its effects on the measured outcomes. When examining drug databases, preoperative COT users were prescribed more opioid pills and/or higher doses (127 - 152.5 mg oxycodone equivalent pills vs. 76 - 91 mg) than those who were not using opioids before the operation. Likewise, patients who used opioids chronically preoperatively were found to maintain opioid usage for a longer time after surgery compared to patients who were opioid naïve. Additionally, despite previous studies proposing that intraoperative ketamine use decreased postoperative COT at one year postoperative, this association was not found in our review.
We also acknowledge the limitations of this review. We did not impose a systematic methodology of the available literature, which may introduce selection bias. Additionally, most of the studies cited were retrospective and did not include any randomized controlled studies. Furthermore, the definition of preoperative opioid use varied between studies and many relied on self-reporting opioid use data.
Nonetheless, this review provides a comprehensive summary of previously published findings to help clinicians set realistic expectations when discussing surgical options with patients on preoperative opioids. The conclusions from these studies also highlight the importance of recognizing patients on opioids preoperatively to effectively risk stratify and identify those who will benefit most from multidisciplinary counseling and guidance. It is imperative for modern healthcare providers to work together to better understand how to manage preoperative pain and minimize opioid usage preoperatively in the spinal surgery population.