1. Context
The prevalence of chronic diseases is increasing, and paying attention to them is a priority (1, 2). Pain is one of the most important symptoms that lead to distress. Pain is an unpleasant experience caused by various types of injuries and can be alleviated using various drug treatments (3-6). Pain might be caused by chronic diseases, such as diabetes, surgeries, traumas, or even internal diseases (7-9). If left untreated, the pain might become chronic and, in turn, causes many problems and complications in patients. Chronic pain refers to treatment-resistant pain that has persisted beyond normal tissue healing time (10). Chronic pain is defined as a group of pains that persist or recur for more than three months and lead to poor quality of life and life satisfaction (11). Considering the subjective nature of pain, studies have often investigated its intensity, nature, duration, and other characteristics in a self-reported manner (12-14).
If a disease occurs during childhood and adolescence, it will affect the rest of the patient’s life (15-17). The fact that children and teenagers, especially during school age, lack information about the specifications of basic equipment, such as bags and shoes, can affect their health, and if repeated, these individuals will suffer from skeletal and muscular problems in adulthood (18, 19). The lack of physical activity and stressful situations due to busy and industrial life have led to many physical and mental complications among school students, including skeletal and muscle pains (20-22).
Musculoskeletal disorders are among the main causes of death and disability and can impose high costs on individuals and countries (23). There are various causes and occupations that are involved in the etiology of musculoskeletal pains. These pains can be local, regional, or widespread (24). Skeletal muscle pain occurs in body areas, such as ligaments, muscles, joints, and bones, and can cause serious local problems, such as fractures, tumors, and infections (25). Some factors, such as computer work, lack of regular physical activity, female gender, high stress, and mental pressure, are effective in causing skeletal and muscle pain (26).
2. Objectives
Considering the importance of pain, the present meta-analysis study aimed to investigate the prevalence of orthopedic pains in Iranian children and adolescents.
3. Methods
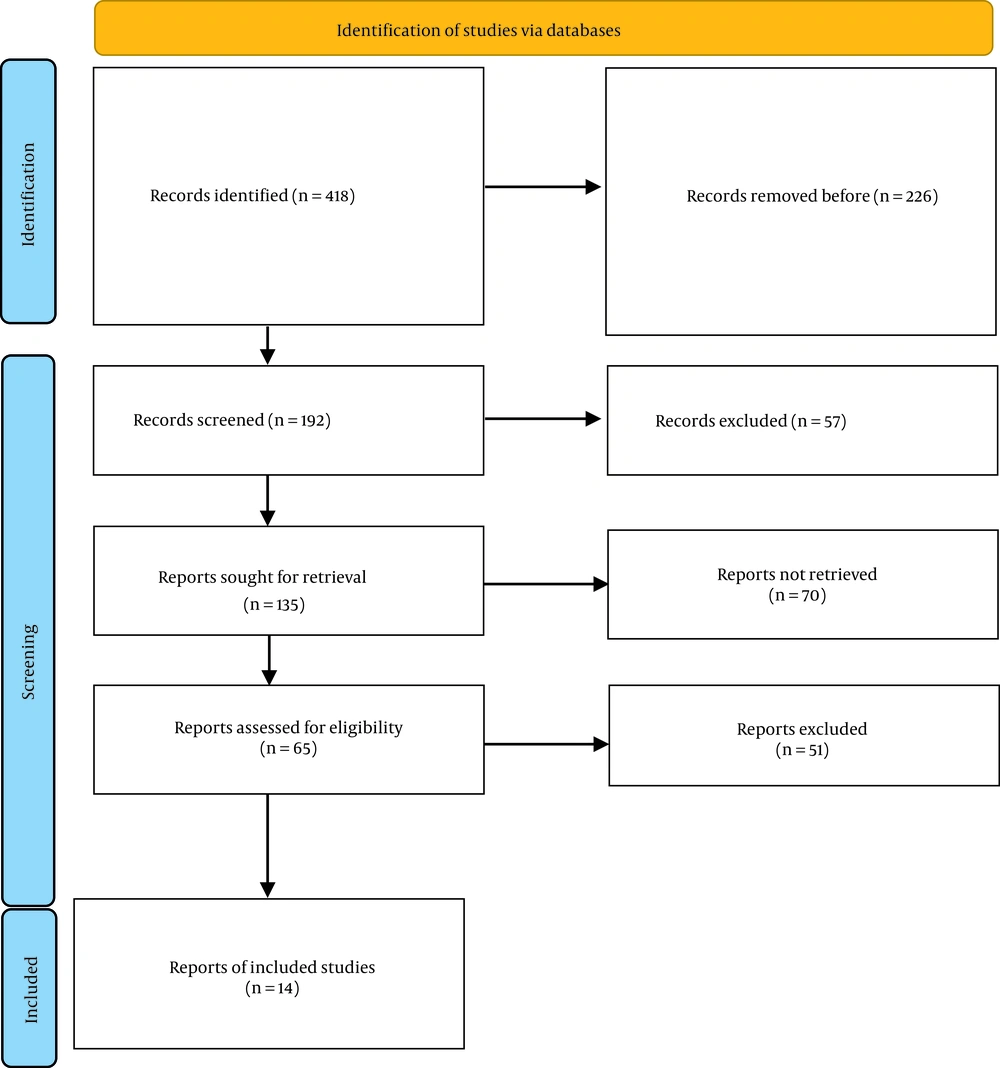
The present study was reported in line with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) (27). This study reviewed the articles that reported the prevalence of neck and shoulder pains among the 5-18-year age group in Iran and extracted their results. Two researchers conducted the search quite independently and extracted the necessary data using a researcher-made checklist.
At first, a list of the titles and abstracts of all the articles was prepared by the researcher and then investigated in order to determine and select the relevant titles. The searching process was carried out using keywords, including adolescents, pain, youth, school-age children, shoulder pain, neck pain, shoulder, and neck, and AND/OR operators for the articles published during 2000 and 2022 in Scopus, Embase, PubMed, Scientific Information Database, Magiran, International Statistical Institute, and Islamic World Science Citation Center databases.
In this study, the PICO criteria include the following:
P: Children and adolescents
I: Prevalence of pain
C: Comparison of pain to healthy children
P: Frequency (%) of pain in children
After searching in the domestic and international databases, the eligible articles entered the meta-analysis phase. The inclusion criteria included access to full-text articles and reports of pain prevalence in a quantitative method. The exclusion criteria also included insufficient data and irrelevant and duplicate studies, meta-analysis articles, and case reports. The collected data were analyzed using Comprehensive Meta‐Analysis software (CMA3) and a random-effect model.
4. Results
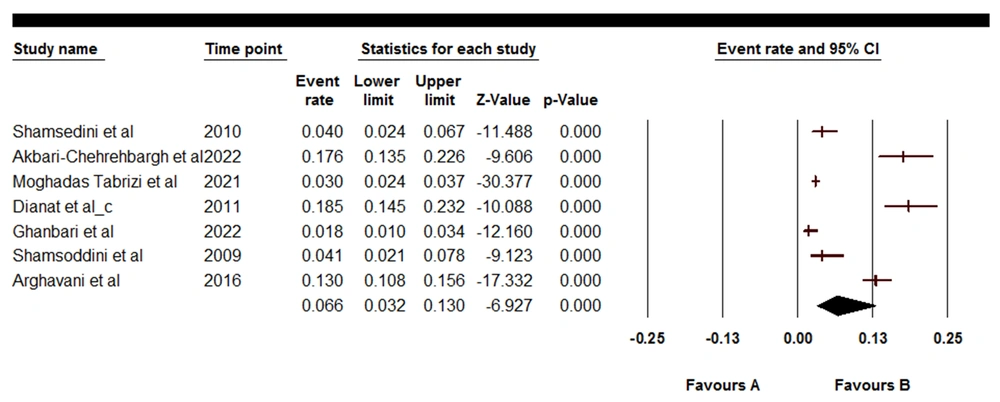
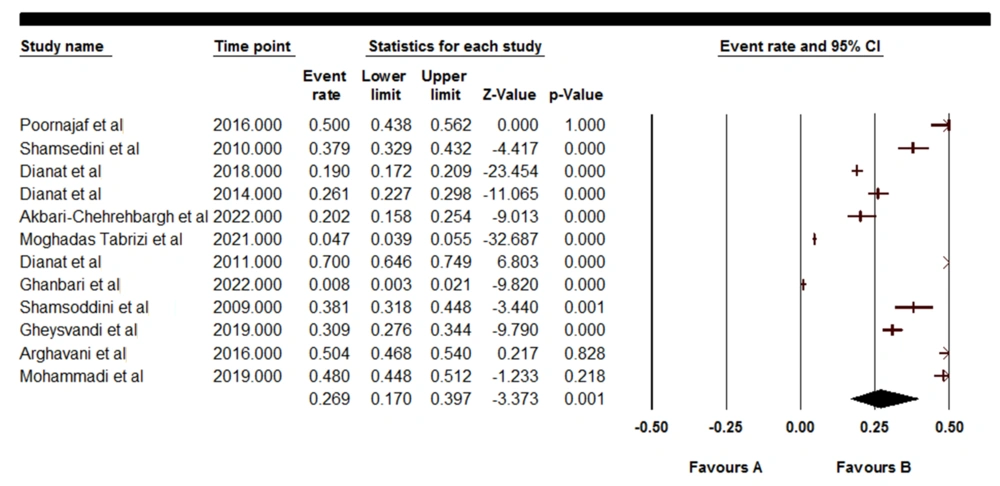
Figure 1 shows that, initially, 418 articles (in all searched databases) were identified, and 14 articles were entered into the systematic review stage (Table 1). The prevalence rates of pains related to wrists/hands, shoulders, elbows, and knees were 6.6 (95% confidence interval [CI]: 3.2 - 13.0), 26.9 (95% CI: 17.0 - 39.7), 2.9 (95% CI: 1.3 - 6.3), and 6.6 (95% CI: 3.0 - 14.2), respectively (Figures 2-5).
| Authors | Year | Place | No. | Mean ± SD | Orthopedic Pains, % | |||
|---|---|---|---|---|---|---|---|---|
| Wrists/Hands | Shoulders | Elbows | Knees | |||||
| Poornajaf et al. (28) | 2016 | Ilam | 244 | - | - | 50 | 0.8 | 4.5 |
| Ja'fari et al. (29) | 2014 | Babol | 998 | 15.96 ± 1.13 | - | - | - | - |
| Shamsoddini et al. (30) | 2010 | Tehran | 340 | 13.4 | 4.01 | 37.9 | 7.23 | - |
| Dianat et al. (31) | 2018 | Tabriz | 1700 | 13.4 ± 0.89 | - | 19.0 | - | - |
| Dianat et al. (32) | 2014 | Tabriz | 586 | 12.8 ± 1.27 | - | 26.1 | - | - |
| Akbari-Chehrehbargh et al. (33) | 2022 | Tehran | 267 | 15.9 ± 1.72 | 17.6 | 20.2 | 4.1 | 8.2 |
| Moghadas Tabrizi et al. (34) | 2021 | Tehran | 2641 | 23.40 ± 5.58 | 2.95 | 4.65 | 0.55 | 5.75 |
| Dianat et al. (35) | 2011 | Tabriz | 307 | - | 18.5 | 70 | - | - |
| Ghanbari et al. (36) | 2022 | Hamadan | 523 | 10.7 ± 1.81 | 1.8 | 0.8 | 1.6 | 2.4 |
| Shamsoddini et al. (37) | 2009 | Tehran | 213 | 13.4 ± 0.53 | 4.1 | 38.1 | - | - |
| Gheysvandi et al. (38) | 2019 | Hamadan | 693 | 35.88 ± 16.85 | - | 30.9 | - | - |
| Arghavani et al. (39) | 2016 | Sanandaj | 735 | - | 13 | 50.4 | 4.7 | 20.4 |
| Ilbeigi et al. (40) | 2017 | Birjand | 60 | - | - | - | - | - |
| Mohammadi (41) | 2019 | Kermanshah | 950 | 11.78 ± 3.6 | - | 48 | 10 | - |
4.1. Wrists/Hands Pain
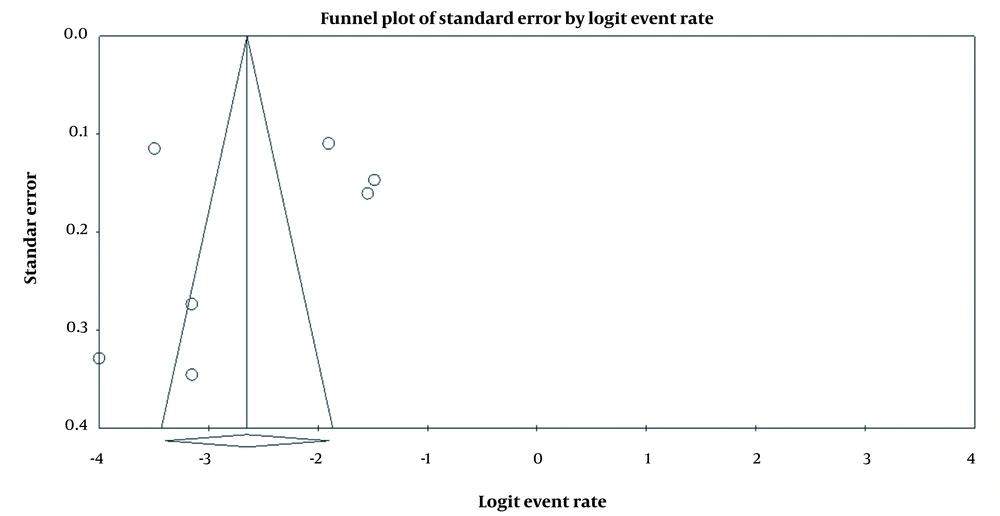
Figures 2 and 3 depict the highest (17.6%) and lowest (1.8%) rates of pain in studies by Akbari-Chehrehbargh et al. (33) and Ghanbari et al. (36), respectively. In addition, the overall prevalence was equal to 6.6 (95% CI: 3.2-13.0) (Q=214.342, I=97.201).
4.2. Shoulder Pain
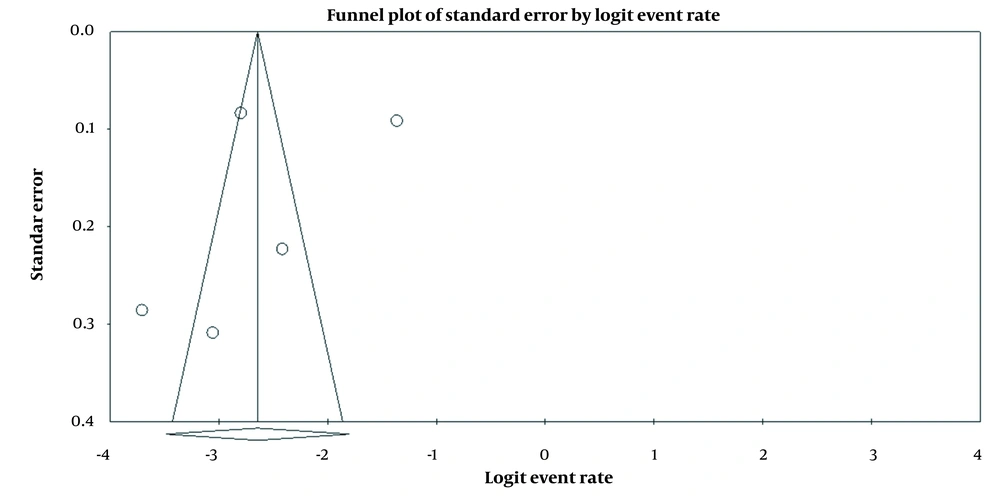
Figures 4 and 5 illustrate the highest (50%) and lowest (0.8%) rates of pain in studies by Poornajaf et al. (28) and Ghanbari et al. (36), respectively. Moreover, the overall prevalence was equal to 26.9 (95% CI: 17.0-39.7) (Q=1247.321, I=99.118).
4.3. Elbow Pain
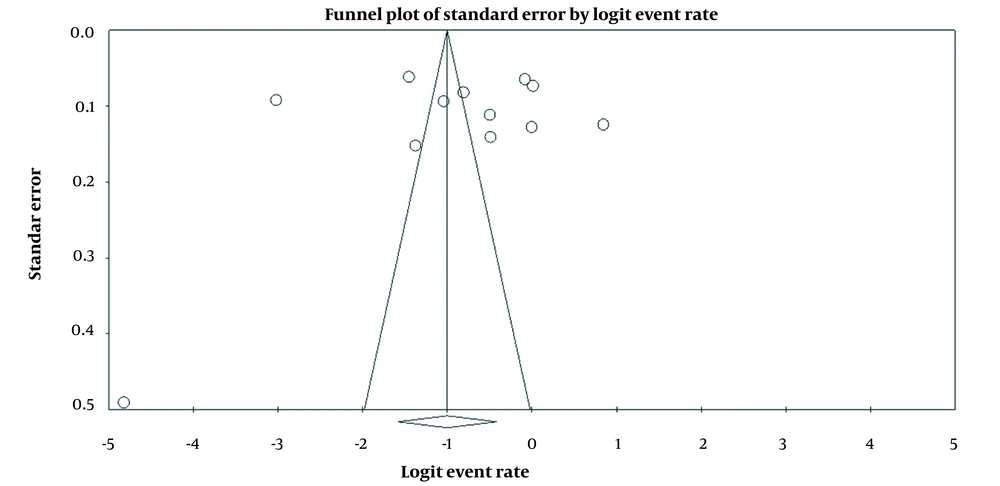
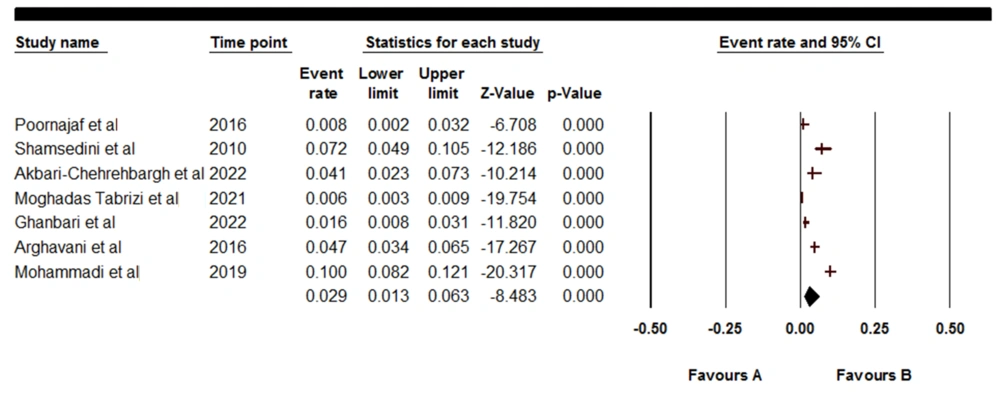
Figures 6 and 7 show the highest (10%) and lowest (0.8%) rates of pain in studies by Mohammadi (41) and Poornajaf et al. (28), respectively. Furthermore, the overall prevalence was equal to 2.9 (95% CI: 1.3 - 6.3) (Q = 140.135, I = 95.72).
4.4. Knee Pain
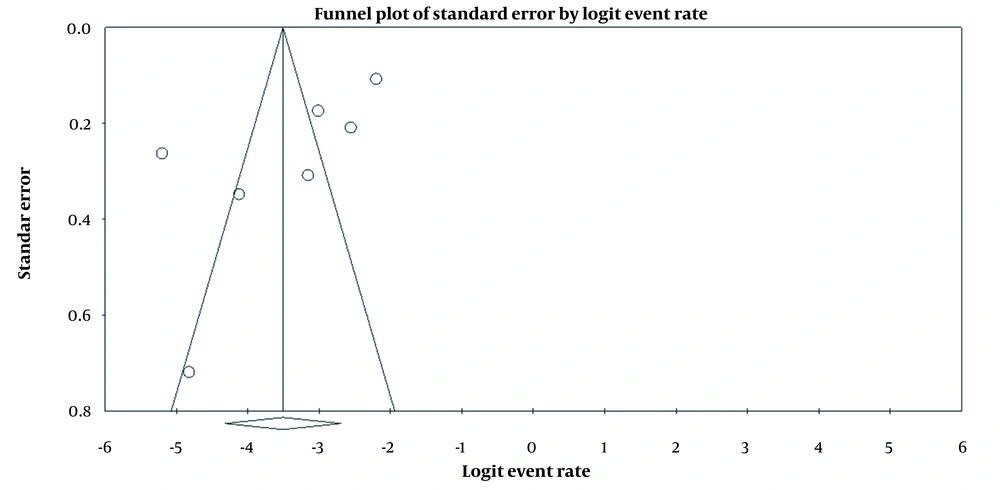
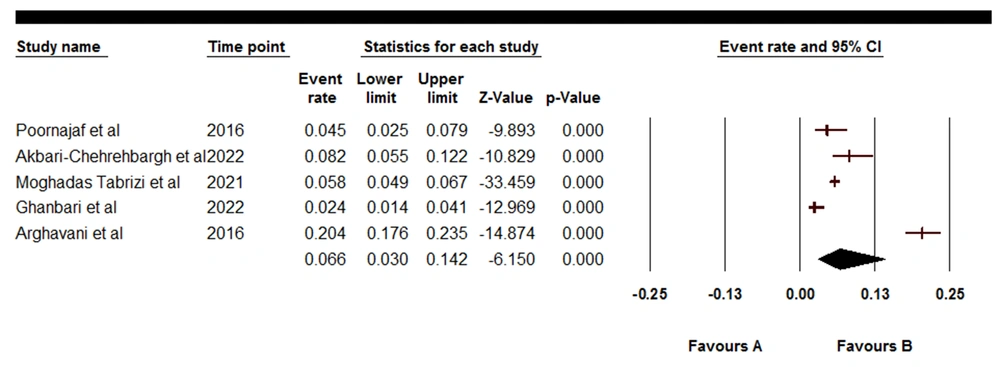
Figures 8 and 9 depict was equal to 6.6 (95% CI: 3.0 - 14.2) (Q = 170.296, I = 97.651).
5. Discussion
According to the level of their activities and prosperity, young individuals play an important role in the development of each country (37, 38). It is important to investigate the clinical and laboratory findings in individuals under 18 years because it allows for identifying disease risk factors and making appropriate interventions to improve the clinical symptoms (39, 40, 42). Additionally, in all age groups, pain causes numerous complications for patients (43-45). For this reason, the present meta-analysis aimed to investigate the prevalence of shoulder and knee pains in individuals under 18 years in Iran.
According to the obtained findings, the prevalence of knee and shoulder pains was 6.6 (95% CI: 3.0 - 14.2) and 29.7 (95% CI: 19.2 - 43.0), respectively. In the meta-analysis of 24 articles on nurses, Clari et al. reported that shoulder pain prevalence was 44% (46). Govaerts et al. also stated that the prevalence of shoulder/neck and neck pains was 54% and 51%, respectively (47). In a study on an adolescent baseball group, Salamh et al. observed great shoulder and knee pains (48), which is consistent with the results of the present study that suggested great shoulder and knee pains among individuals under 18 years in Iran.
Previous meta-analyses also investigated the prevalence of shoulder and neck pains in different medical professions. In this regard, Bedi et al. reported that the prevalence rates of shoulder and neck pains among dentists were 29% and 58%, respectively (49). Lietz et al. also showed that the prevalence of neck, shoulder, upper back, and lower back pains among dentists is 58.5%, 43.1%, 41.1%, and 56.4%, respectively (50). Epstein et al. also demonstrated that the prevalence of lumbar spine disorders and carpal tunnel pain among surgeons was 19% and 9%, respectively (51).
In the meta-analysis of eleven articles, Tavakkol et al. showed that the prevalence of neck and shoulder pains among operating room personnel was 53.66% and 55.63%, respectively (52). In addition, in a meta-analysis of 24 articles, Clari et al. stated that the prevalence of shoulder pain was 44% (46).
Moreover, in other studies, the pain condition has been investigated, especially in the group of teenagers and children. Accordingly, in a study by Hakala et al., the prevalence of shoulder and neck pains was reported in 24% and 12% of females and males aged 14 years (53). Furthermore, in a study by de Oliveira et al. on 310 adolescent athletes, the prevalence of shoulder pain was reported to be 43.5% (54).
One of the limitations of this study was the study of pain in Iran and the study of only certain types of pain, including orthopedic pains. Therefore, it is suggested to carry out further extended studies at the local level. The strength of the study was pain examination as an important variable in a special group of children and adolescents. Considering that children are the future builders of society, it is important to examine their pain.
5.1. Conclusions
The prevalence of shoulder and knee pains in individuals under 18 years in Iran was high. Therefore, it is necessary to make necessary interventions and take preventive measures.