1. Background
Hypothermia is defined as internal body temperature below 36°C (1, 2). The American Society of Anesthesiologists (ASA) defines normal body temperature as 36 - 38°C (3). Naturally, core body temperature is precisely controlled by defense mechanisms. Body temperature regulation during general anesthesia follows a specific pattern, with the heat response threshold rising only slightly while the cold response threshold decreases markedly. As a result, hypothermia is a common complication of general anesthesia. In spinal and epidural anesthesia, the threshold for activating the defense mechanisms of vasoconstriction and chills decreases. Furthermore, although the pattern is similar to general anesthesia, it is less severe. Disorders of temperature regulation during anesthesia appear to be more related to central responses, both in general and in local methods, although peripheral systems that regulate body temperature also play a role (4, 5). Unwanted postoperative hypothermia is the most common thermal change following anesthesia and surgery (1, 6). Although the internal temperature in individuals is tightly controlled, general anesthesia significantly disrupts the thermoregulatory system (7, 8).
Central hypothermia can explain the negative cardiac conditions and consequences in high-risk patients. Hypothermia significantly increases blood transfusion and surgical wound infections (1, 9, 10), prolonged recovery after anesthesia (11), negative nitrogen balance after surgery (8), and increased mortality in elderly patients with sepsis (12). A slight change (0.05 - 1.5°C) through the sympathetic causes an average increase in blood pressure. Also, hypothermia disrupts platelet function (13, 14). Inadvertent perioperative hypothermia (IPH) is a known complication of general and local anesthesia; however, body temperature is rarely monitored in hospitals (15).
There are several methods to prevent or treat hypothermia in patients after surgery, including aluminum blankets, head covers, forced-air warming devices, or radiant heaters. Several risk factors for developing hypothermia were reported in previous studies, including age, gender, body mass index (BMI), a history of diabetic neuropathy, emergency surgery, physical well-being based on ASA score, large body cavity surgery, large vessel exposure, anesthesia method, re-warming method, volume and temperature of intravenous (IV) fluids given to patients, and anesthesia or surgery duration (1, 11, 16). It is thought that these factors could be used to reduce hypothermia more effectively after surgery (1).
2. Objectives
Given that internal studies in this field are limited, we decided to investigate the prevalence, predictors, and effective factors of hypothermia in patients after surgery in the present study (17).
3. Methods
3.1. Participants
This descriptive cross-sectional study was conducted in 2017 on 400 adult patients undergoing elective surgery under general or spinal anesthesia. The inclusion criteria were all adult patients undergoing elective surgery. Exclusion criteria were patients undergoing cardiac surgery, patients with fever or abnormal temperature, sepsis, ASA score III or more, traumatic brain injuries and Glasgow coma score lower than 12, and patients with a history of thyroid disorders.
Tympanic membrane temperature was measured and recorded at the time of arrival at the post-anesthesia care unit and every 30 minutes after arrival using an infrared tympanic thermometer TM 80 (Healer Company). This measurement method is ideal because the tympanic membrane and hypothalamus have a common arterial blood source originating from the carotid artery. Therefore, the tympanic membrane is considered a direct reflector of core temperature. All patients were examined for infection or ear wax. The operating room temperature was 21 - 22°C, and hypothermic was determined as a body temperature below 36°C. Patients' demographics and other information, including physical status based on ASA score, anesthesia type, IV fluid volume received by patients, intraoperative blood loss, anesthesia duration, surgery duration, BMI, and visual pain score, were also collected in checklists by the researcher and compared between hypothermic and normothermic patients. All information was collected from patients' medical records.
3.2. Sample Size
The sample size was calculated according to the prevalence of hypothermia in patients hospitalized in the ICU after elective surgery, which was about 40% in Luís et al.'s study (1). Based on Cochran's formula with 95% confidence level and 0.05 precision, the minimum sample size required in this study was about 369 patients.
3.3. Statistical Analysis
Statistical analysis was performed using the IBM SPSS software version 26. Descriptive results of qualitative variables were reported by frequency (percent), and quantitative variables were demonstrated as mean ± standard deviation. Continuous variables were compared using the independent t-test, and the chi-square/Fisher’s exact test was used to compare categorical variables. P < 0.05 was considered statistically significant.
4. Results
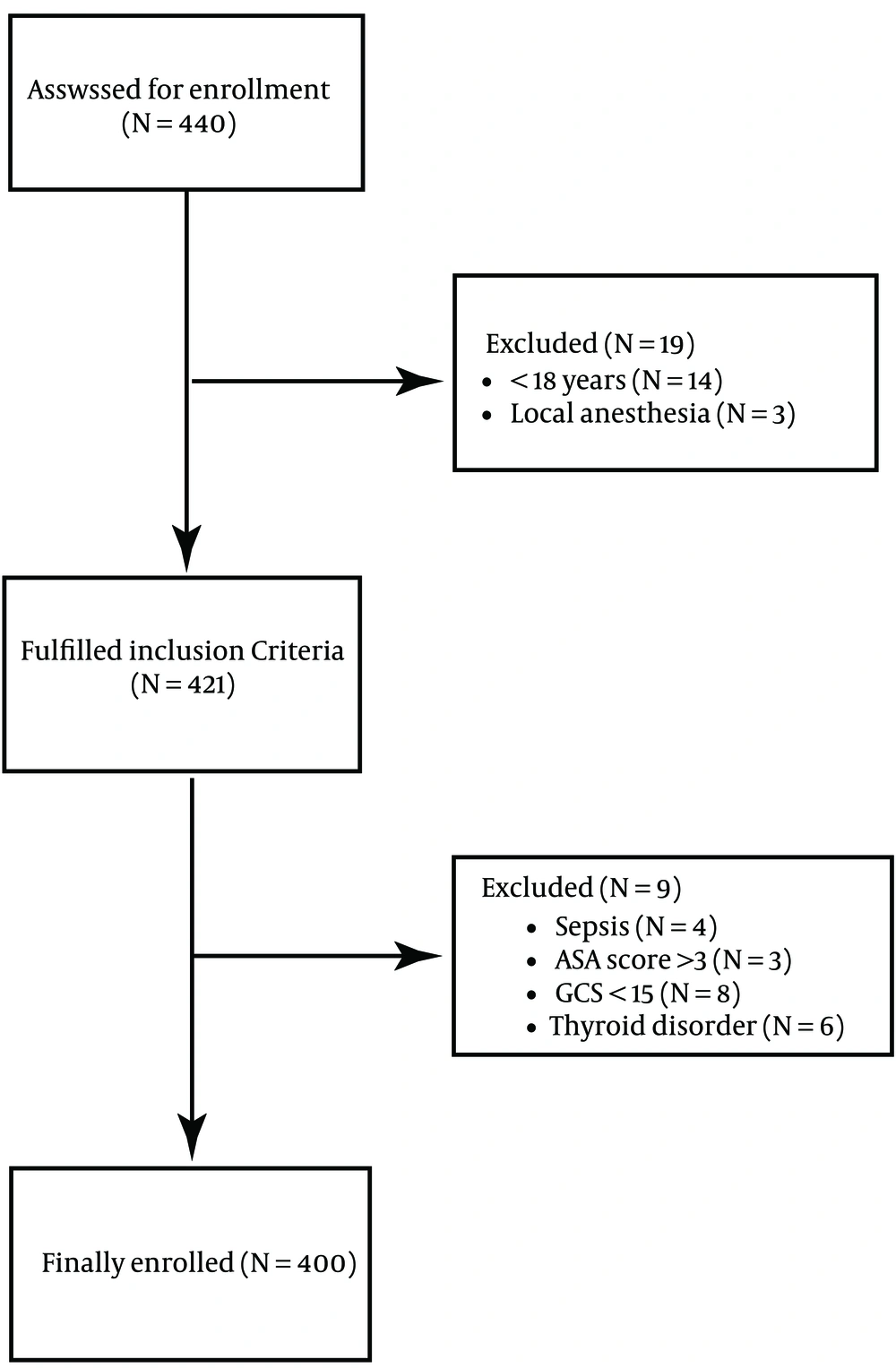
Patients were selected based on the convenience sampling method. Four hundred forty patients were assessed for enrollment, 421 of whom were enrolled in the study based on the inclusion criteria, and 19 were excluded according to the exclusion criteria. Therefore, 400 patients were finally analyzed (Figure 1).
The subjects were in the age range of 16 to 80 years old, with a mean age of 43.02 ± 16.07 years, and 251 (53.8%) of them were male. Based on the classification of patients' physical condition according to ASA score, most patients were classified as ASA score I (70.8%). Most of the patients underwent general anesthesia (58.5%); 33.3% of them underwent surgery in spring, 18.3% in summer, 18% in autumn, and 30.3% in winter. The IV fluids injected into the patients were 1 to 4 liters, averaging 2.65 ± 0.87 liters. The mean anesthesia duration in patients ranged from 35 to 250 minutes, and their mean surgery time was 25 to 240 minutes. Visual pain scores ranged from 1 to 6, averaging 2.4 ± 0.98. Hypothermia was observed in 95 (23.7%) patients at the time of arrival at the post-anesthesia care unit and in 90 (22.5%) patients 30 minutes after recovery. It could be said that the prevalence of hypothermia in patients undergoing elective surgery is 20 to 28% and 18.5 to 26% at the time of arrival at the post-anesthesia care unit and 30 minutes after arrival, respectively.
Findings obtained from the chi-square test showed that the prevalence of hypothermia at the beginning of recovery (P = 0.011) and 30 minutes after recovery (P = 0.014) was significantly higher in females. Also, it was shown that patients who underwent general anesthesia were significantly more prone to hypothermia at the time of arrival at the post-anesthesia care unit (P = 0.029) and 30 minutes after arrival (P = 0.047). The prevalence of hypothermia at the time of arrival at the post-anesthesia care unit (P = 0.043) and after 30 minutes of arrival (P = 0.031) was significantly higher in patients with ASA score II than those with ASA score I.
The independent t-test also showed that the mean BMI of hypothermic patients was significantly lower than patients without hypothermia (P < 0.0001). Results indicated that the mean volumes of IV fluids injected into patients (P < 0.0001) and intraoperative blood loss (P < 0.0001) were higher in hypothermic patients both at the time of arrival at the post-anesthesia care unit and 30 minutes after arrival. The mean scores of anesthesia duration (P = 0.043), surgery duration (P = 0.027), and visual analog scale (VAS) (P = 0.027) in patients who were hypothermic at the time of arrival at the recovery room were significantly higher than in non-hypothermic patients, while no difference was observed between hypothermic and non-hypothermic patients after 30 minutes of arrival. There were no significant differences between the prevalence of hypothermia in the two groups in the year’s seasons. Further details are listed in Table 1.
| Hypothermia at the Time of Arrival at the Post-anesthesia Care Unit | P-Value | Hypothermia After 30 Minutes of Arrival at the Post-anesthesia Care Unit | P-Value | |||
|---|---|---|---|---|---|---|
| Yes (N = 95) | No (N = 305) | Yes (N = 90) | No (N = 310) | |||
| Age, y | 43.36 ± 15.80 | 42.91 ± 16.10 | 0.789 b | 43.01 ± 15.78 | 43.02 ± 16.10 | 0.991 b |
| IV fluids, L | 3.37 ± 0.48 | 2.42 ± 0.84 | < 0.0001 b | 3.35 ± 0.48 | 2.44 ± 0.85 | < 0.0001 b |
| Anesthesia duration, min | 103.73 ± 71.85 | 75.08 ± 34.63 | 0.043 b | 100.72 ± 70.77 | 76.42 ± 36.98 | 0.127 b |
| Surgery duration, min | 93.94 ± 70.91 | 65.15 ± 34.58 | 0.027 b | 91.05 ± 69.91 | 66.45 ± 36.83 | 0.085 b |
| BMI, kg/m2 | 25.68 ± 4.20 | 27.23 ± 4.54 | < 0.0001 b | 25.29 ± 4.17 | 27.13 ± 4.58 | < 0.0001 b |
| VAS score (1-10) | 2.89 ± 1.22 | 2.33 ± 0.86 | 0.027 b | 2.89 ± 1.21 | 2.33 ± 0.88 | 0.085 b |
| Intraoperative blood loss, mL | 385.2 ± 322.7 | 245.8 ± 261.3 | < 0.0001 b | 377.6 ± 316.4 | 255.6 ± 243.4 | < 0.0001 b |
| Gender | 0.011 c | 0.014 c | ||||
| Male | 33 (17.8) | 152 (82.2) | 32 (17.3) | 153 (82.7) | ||
| Female | 62 (28.8) | 153 (71.2) | 58 (27.0) | 157 (73.0) | ||
| ASA score | 0.043 c | 0.031 c | ||||
| I | 60 (21.2) | 223 (78.8) | 56 (19.8) | 227 (80.2) | ||
| II | 35 (29.9) | 82 (70.1) | 34 (29.1) | 83 (70.9) | ||
| Anesthesia type | 0.029 c | 0.047 c | ||||
| General | 64 (27.4) | 170 (18.7) | 60 (25.6) | 174 (74.4) | ||
| Spinal | 31 (72.6) | 135 (81.3) | 30 (18.1) | 136 (81.9) | ||
| Season | 0.935 c | 0.845 c | ||||
| Spring | 29 (21.8) | 104 (78.2) | 27 (20.3) | 106 (79.7) | ||
| Summer | 18 (24.3) | 56 (75.7) | 16 (21.6) | 58 (78.4) | ||
| Autumn | 30 (25.0) | 91 (75.0) | 30 (23.6) | 91 (76.4) | ||
| Winter | 18 (24.8) | 54 (75.2) | 17 (24.8) | 55 (76.4) | ||
Abbreviations: IV, intravenous; BMI, body mass index; VAS, Visual Analogue Scale; ASA, American Society of Anesthesiologists.
a Values are expressed as mean ± SD or No. (%).
b Independent t-test
c Chi-square test
5. Discussion
The present research is a cross-sectional study to determine the prevalence of hypothermia and the variables contributing to its development in individuals undergoing elective surgery. This research is the first study assessing the prevalence of hypothermia following elective surgery and its related factors in Iran. In our study, hypothermia (body temperature below 36°C) was observed in 95 (23.7%) out of 400 patients at the beginning of recovery and 90 (22.5%) patients 30 minutes after recovery. All reported cases of hypothermia in our study were mild, and the temperature was 34 - 36°C. The numbers reported in our study were lower than most studies. This discrepancy could be due to patients' condition (in some studies, patients with ASA scores higher than II were included), surgical conditions (in this study, only patients who underwent elective surgery were considered), and differences in patients’ age, gender, and BMI. Another important factor causing this discrepancy could be different definitions of hypothermia in different studies.
Patients participating in this study were between 16 to 80 years old. The mean age range of patients who developed hypothermia at the time of arrival at the post-anesthesia care unit was 43.36 ± 15.80 years old, and the mean age range of patients who developed hypothermia 30 minutes after arrival was 43.01 ± 15.80 years old. No significant relationship was found between age and the prevalence of hypothermia. This finding is in contrast with Karalapillai et al.’s and Aksu et al.’s studies, the reason for which could be significant differences in sample sizes (11, 18, 19).
A total of 28.8% and 27% of female patients included in this study developed hypothermia at the time of arrival at the post-anesthesia care unit and 30 minutes after arrival, respectively. These values were estimated to be 17.8% and 17.3% in men, respectively. There was a significant relationship between the female gender and postoperative hypothermia. This finding is in contrast with previous studies (18-21). The reason could be accidental differences in the number of female patients included in other studies and ours.
The mean BMI of patients in this study was significantly lower than others. This finding was in contrast with Abelha et al.’s (11) and Aksu et al.’s (19) studies and consistent with Kleimeyer et al.’s and Luís et al.’s (1, 20) studies.
Increased ASA score was associated with increased prevalence of hypothermia; thus, 21.2% of those with ASA score I and 29.9% of those with ASA score II developed hypothermia at the time of arrival at the post-anesthesia care unit. These figures reached 19.8% and 29.1% 30 minutes after recovery, respectively. This finding contrasted with several previous studies (11, 19). Patients with ASA score III and higher were not included in our study. A higher ASA score weakens the thermoregulatory system, which can be the reason for the increased prevalence of hypothermia in patients with ASA score II compared to patients with ASA score I. In general, patients with higher ASA scores are not suitable candidates for surgery due to the higher possibility of anesthesia and postoperative complications. Therefore, if needed to choose between surgery and other treatment options, palliative treatments are a better choice for them.
Patients with higher intraoperative blood loss were more likely to experience postoperative hypothermia. Other studies showed the opposite. The hypothermic patients who experienced low hemoglobin and low hematocrit required a blood transfusion (22). According to Kander and Schott, even mild hypothermia significantly increases blood loss by approximately 16% (4 – 26%) and increases the relative risk of transfusion by approximately 22% (3 – 37%) (23).
Most of the patients in our study underwent general anesthesia (58.5%), of which 27.4% developed hypothermia at the time of arrival at the post-anesthesia care unit and 25.6% developed hypothermia 30 minutes after arrival. On the other hand, the prevalence of hypothermia in patients undergoing spinal anesthesia was 18.7% and 18.1% at the time of arrival at the post-anesthesia care unit and 30 minutes after arrival, respectively. The relationship between the anesthesia type and the prevalence of hypothermia in both groups was significant. The decreased prevalence of hypothermia after 30 minutes of arrival at the post-anesthesia care unit using both types of anesthesia can be due to reducing the effects of anesthetics and leaving the cold space of the operating room. Another reason is the gradual warming of body cavities and vessels, which were openly exposed during surgery. These findings were consistent with the results of several previous studies (1, 11, 19, 24).
Anesthesia and surgery durations in our patients were 25 to 240 minutes and significantly higher in patients who developed hypothermia at the arrival at the post-anesthesia care unit, but there was no significant relationship between developing hypothermia 30 minutes after arrival at the post-anesthesia care unit and the anesthesia and surgery time, which could result from using efficient techniques to warm patients up after arrival at the post-anesthesia care unit. The results of Abelha et al.’s research showed that anesthesia and surgery time of more than 180 minutes were significantly related to the prevalence of hypothermia (11). Increasing the prevalence of hypothermia after long anesthesia and surgery could be due to the operation room temperature, body cavity and vessel exposure during surgery, and inefficient warming-up techniques during surgery. So, increasing operation room temperature, usage of efficient warming up techniques such as injecting warm IV crystalloids to patients, and, if possible, usage of less invasive surgery methods which are shorter and do not expose huge body cavities such as laparoscopy should be considered to prevent postoperative hypothermia.
Patients in this study who developed hypothermia at the time of arrival at the post-anesthesia care unit had higher preoperative VAS scores than other patients. Also, there was no significant relationship between the VAS score before surgery and the prevalence of hypothermia 30 minutes after arrival at the post-anesthesia care unit. The effect of VAS score on the prevalence of hypothermia was not a matter of interest in previous studies, except for one study whose results were consistent with ours (1).
Hypothermic patients in our study received more IV fluids than other patients. Moreover, the relationship between IV fluid volume given to hypothermic patients and the prevalence of hypothermia was significant. This could happen because of two reasons:
(1) One of the techniques to prevent hypothermia is injecting warm IV crystalloids into patients.
(2) Hypothermic patients are prone to shock, increasing the need for IV fluids to maintain normal hemostasis.
These findings were consistent with previous studies (11, 19).
There was no significant relationship between the year’s season and the prevalence of hypothermia in patients undergoing elective surgery.
Due to these significant results and hypothermia complications, such as cardiovascular disorders, surgical site infection, coagulation disorders, negative nitrogen balance, delayed wound healing, delayed patient recovery, the need for longer hospitalization, and other hazards, particularly in patients with underlying disease, and since limited domestic studies have been conducted in this field, it is necessary to provide a platform for further research and studies, as well as appropriate therapeutic and control measures such as the use of heating devices in the post-anesthesia care unit, heating blankets, warm IV fluids and other external measures to increase the temperature to manage this complication (25).
5.1. Limitations
A larger national study of perioperative hypothermia risk factors and associated complications is needed to increase the generalizability of results in other settings and populations. This study was cross-sectional; therefore, there is no preoperative and intraoperative temperature assessment. Confounding variables, such as comorbidities, were not examined.
5.2. Suggestions
Although many variables were examined in this study, future research could focus on describing other factors, such as preoperative and intraoperative patients' body temperature, whether patients were warmed up during the hospitalization before surgery or not (26, 27), operation room temperature (28), and injected IV fluid temperature. It is suggested that the effects of hypothermia on increasing the mortality rate be investigated in future studies.
5.3. Conclusions
More than a quarter of patients develop hypothermia following elective surgery. We found that female patients and patients undergoing general anesthesia were more likely to experience postoperative hypothermia. Also, hypothermia is more common in patients with lower BMIs, higher IV fluid volume injections, more surgery and anesthesia time durations, ASA score II, and higher VAS scores. Continuous and routine measurement of patients' body temperature after surgery, use of preventive methods, and more attention to patients with risk factors related to hypothermia should be considered by medical staff.