1. Background
Prolongation of surgery and postoperative pain relief are major concerns for both anesthesiologists and patients undergoing surgical procedures under the sub-arachnoid block. Apart from standard analgesics such as NSAIDs and narcotics, additives along with spinal drugs are more prevalent to increase the duration of the block and postoperative analgesia.
The most preferred regional anesthesia in patients undergoing surgeries involving the below umbilicus area is by sub-arachnoid block. Most surgeries prolong, and regression of spinal block remains a major concern for anesthesiologists. Hence, various additives, along with spinal drugs, are given to achieve desired outcomes such as rapid onset, safe hemodynamic changes, intra-operative sedation, prolonged action, and postoperative analgesia. This technique is simple and less cumbersome and has gained wide acceptance. Good pain control has the potential to allow early mobilization and hospital discharge.
Clonidine and dexmedetomidine are centrally acting α2 adrenoceptor agonists (1, 2) used as adjuvants to local anesthetics because of their sedative, analgesic, and hemodynamic stabilizing effect. They have been found to prolong the duration of spinal or sub-arachnoid block following intrathecal administration. Clonidine (1-3) is an imidazoline (4) compound, an alpha-adrenergic agonist with selectivity for α2 receptors. Studies suggest that clonidine produces analgesia by depressing the release of C-fiber transmitters and hyperpolarization of postsynaptic dorsal horn neurons (5). Clonidine binding to motor neurons in the dorsal horn may prolong motor block (6). Clonidine affects blood pressure in a complex fashion after neuraxial or systemic administration. It produces hypotension by activating postsynaptic α2 adrenoceptors in the brain stem and directly inhibiting sympathetic pre-synaptic α2 adrenoceptors neurons in the spinal cord (7).
Dexmedetomidine (8) is a second-generation α2 adrenergic receptor-specific, pharmacologically active d-isomer of medetomidine. Dexmedetomidine (8, 9) possesses selective α2 adrenoceptor agonist activity, particularly for the 2A receptor subtype. This makes it a more effective analgesic at lower doses than clonidine, which requires higher doses. Additionally, dexmedetomidine does not have the undesirable cardiovascular effects associated with α1-receptor activation. A significant opioid-sparing effect is noted in dexmedetomidine. The first human study of dexmedetomidine was conducted by Kanazi et al. (9).
2. Methods
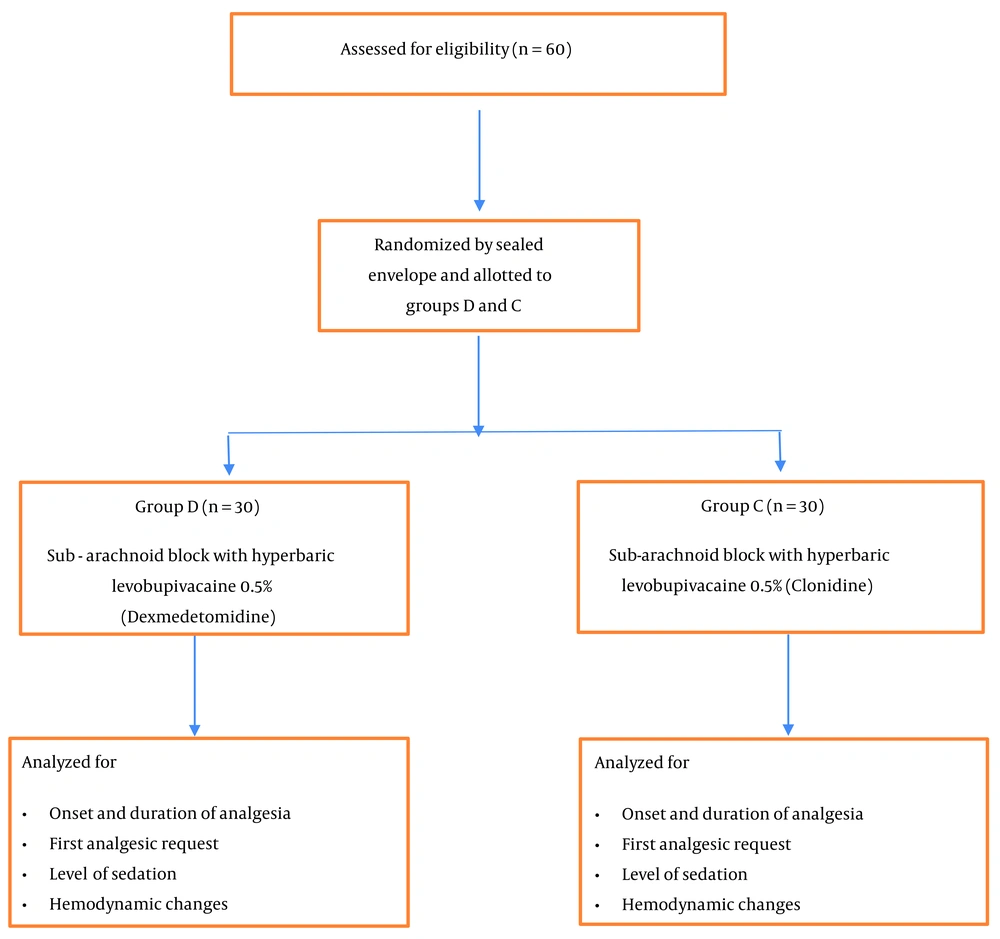
After obtaining clearance from the Institutional Ethics Committee, this double-blind, randomized comparative study was conducted in the Department of Anesthesiology in a tertiary care institute. The sample size calculation was done (α = 0.05 and β = 0.90) with statistical software G Power 3.1 (10). The study enrolled 60 patients (Figure 1), 30 in each group of dexmedetomidine (D) (DEXTOMID 50 µg/0.5 mL manufactured by NEON laboratories, India) and clonidine (C) (CLONEON 150 µg/mL, manufactured by NEON laboratories, India). The inclusion criteria included age between 20 and 50 years of either sex, being scheduled for an elective lower abdominal surgery under sub-arachnoid block using 0.5% hyperbaric levobupivicaine (LEVO-ANAWIN Heavy 0.5%, manufactured by NEON laboratories, India), the American Society of Anesthesiologists Status I and II, and surgery duration of more than 1.5 hours and less than 3 hours. The exclusion criteria included patient denial for sub-arachnoid blocks, sub-arachnoid block contraindications, cesarean section, failed or patchy sub-arachnoid block, and uncontrolled hypertension and diabetes on the day of surgery. Allocation was done randomly into two groups by asking the patients to pick lots from a sealed bag. Written informed consent was taken from all patients. A t-test was used to analyze age, sex, and duration of surgery.
The technique (for both groups): Once the patient had been admitted to the operating room, peripheral venous cannulation was done using 18-gauge (G) venflon. All the basic regular monitors for the sub-arachnoid block were attached, and vitals were noted. As per institution routine, Inj. Glycopyrrolate 0.2 mg and Inj. Emeset 4 mg was given intravenously to both groups for an antisecretory and antiemetic effect prior to Sub-Arachnoid block. Patients were put in right lateral decubitus or a sitting posture, and spine parts were cleaned and draped. Using a 25-Gauge (G) Quincke needle, the patient was given a sub-arachnoid block with additives (Dexmedetomidine or clonidine) along with 0.5% hyperbaric levobupivicaine. Group C received clonidine 50 µg along with 0.5% hyperbaric levobupivicaine 15 mg, and Group D received dexmedetomidine 5 µg along with 0.5% hyperbaric levobupivicaine 15 mg. The analgesia onset, intraoperative hemodynamic changes every 30 min, sedation, duration of the blockade, and postoperative analgesic requisite and frequency were recorded in both groups.
The sensory blockades were assessed by pinprick sensation using a blunt 25-G needle below the umbilicus. The motor level was assessed according to a modified Bromage scale (0 = patient can move the hip, knee, and ankle, 1 = unable to move the hip, but able to move knee and ankle, 2 = unable to move the hip and knee but able to move the ankle, 3 = unable to move the hip, knee, and ankle). Time to reach the T6 dermatome, the highest dermatomal level (peak sensory level), and regression to S1 were recorded. The time to reach Bromage 3 and regression to Bromage 0 was also recorded.
All the durations were calculated from the time of the sub-arachnoid block. Once the regression of blockade to S1 was achieved in both groups, patients were transferred from the recovery room to the postoperative ward. In the postoperative ward, postoperative analgesia was recorded using the Visual Analogue Scale (0 = No pain, 10 = Worst unbearable pain). Also, other parameters were monitored, recorded, and treated appropriately in the first 24 hours, such as the level of sedation using the Cambell sedation score (1 = Wide awake and alert, 2 = Awake and comfortable; 3 = Drowsy and difficult to arouse, 4 = Not arousable), and hemodynamic changes (Bradycardia = less than 50, hypotension MAP = less than 70 mmHg).
2.1. Statistical Analysis
The data are expressed as mean, standard deviation, and range. Normally distributed continuous variables were compared between the groups by the Kolmogorov-Smirnov test. Categorical data were analyzed using the chi-square test or Fisher's exact test, as appropriate. Ordinal categorical data were compared using an independent t-test. Data were entered in Excel and analyzed using SPSS software version 21.
3. Results
Sixty patients were enrolled in the study. Thirty patients were in each group (Group C and Group D). Demographic data in the two groups and the duration of surgery are compared in Table 1.
| Characteristics | Clonidine | Dexmedetomidine |
|---|---|---|
| Age (y) | 37.3 ± 11.6 | 30.5 ± 15.8 |
| Weight (Kg) | 40.1 ± 13 | 46 ± 8 |
| Height (cm) | 163.6 ± 5.4 | 158.3 ± 0.7 |
| Male/Female | 18/12 | 21/9 |
| Duration of surgery (min) | 135.2 ± 15.4 | 143.7 ± 30.2 |
The technique of the sub-arachnoid block was easy, with a single attempt for all 60 patients, and recovery from the sub-arachnoid block was uneventful. The time taken to reach the desired dermatome level T8, i.e., the analgesia onset, was not statistically significant between the groups. Peak sensory level T6 did not differ between the groups. A significant P-value was observed when compared with the two dermatome regressions (T10) in both groups. The time taken to regress two dermatomes T10 delayed in Group D (135 ± 15 min) compared to Group C (130 ± 20 min) (P < 0.05) (Table 2). The desired S1 segment regression to shift the patient from recovery to the postoperative ward was compared, with Group D being prolonged (Group D 305 ± 50.4 min vs. Group C 290 ± 47.2 min; P < 0.05). Concerning the time taken to full regression of blockade Bromage 0, Group D (285 ± 60 min) had a longer time to regress to Bromage 0 than Group C (280 ± 45 min) (P < 0.05) (Table 2). The first rescue analgesic demand was prolonged in Group D (700 ± 160 min) compared to Group C (506 ± 112 min) (P < 0.05) (Table 3). Also, the frequency of rescue analgesics was less in Group D compared to Group C (P < 0.005) (Table 3). Bradycardia and hypotension were observed in 7 patients of both groups, intervened with atropine and ephedrine, but there was no significant difference, as shown in Tables 2 and 3. The level of sedation in Group D (1.3 ± 0.46) differed significantly from Group C (0.4 ± 0.01), with dexmedetomidine showing an increased level (Table 3).
| Characteristics | Clonidine | Dexmedetomidine | P-Value |
|---|---|---|---|
| Time to dermatome T8 (min) | 9.2 ± 0.2 | 9 ± 0.3 | 0.71 |
| Time to peak sensory level T6 (min) | 15.3 ± 2.1 | 14.5 ± 1.9 | 0.08124 |
| Time taken to reach 2-segment regression T10 (min) | 130 ± 20 | 135 ± 15 | 0.001 |
| Time taken to S1 segment regression (min) | 290 ± 47.2 | 305 ± 50.4 | 0.001 |
| Time taken to regression Bromage score ‘0’(min) | 280 ± 45 | 285 ± 60 | 0.001 |
| Characteristics | Clonidine | Dexmedetomidine | P-Value |
|---|---|---|---|
| Mean duration to the first dose of rescue analgesic (min) | 506 ± 112 | 700 ± 160 | 0.01 |
| No. doses of rescue analgesic | 1.99 | 1 | 0.005 |
| Sedation level | 0.4 ± 0.01 | 1.3 ± 0.46 | 0.0001 |
4. Discussion
Additives in the sub-arachnoid block may greatly impact the onset, duration, hemodynamic changes, desired sedation, postoperative analgesia, and subsequent postoperative analgesic requirements. This study compared dexmedetomidine and clonidine as sub-arachnoid block additives along with hyperbaric levobupivicaine 0.5% for patients undergoing surgical procedures involving the lower abdomen.
Rao et al. (11) suggest better anesthesia and a wide variation in sensory levels in 0.5% hyperbaric Levobupivacaine. The hemodynamic profiles of both isobaric and 0.5% hyperbaric Levobupivacaine were similar. Hence, our study used 0.5% hyperbaric Levobupivacaine as the drug of choice for the sub-arachnoid block, added with alpha 2 agonists dexmedetomidine or clonidine.
Verma et al. (12) showed that adding fentanyl to intrathecal levobupivacaine in lower abdominal surgeries had effective sensory-motor blockade for a sufficient duration with stable hemodynamics. Narcotics have undesired effects such as vomiting and pruritis. Hence, we used alpha 2 agonists such as dexmedetomidine and clonidine and compared their analgesic efficacy.
Ganesh and Krishnamurthy (13) concluded that alpha 2 agonists, when added to 0.5% hyperbaric bupivacaine intrathecally, have a faster onset of both sensory and motor blocks and prolong the duration of analgesia. Our study used dexmedetomidine 5 µg and clonidine 50 µg added to 0.5% hyperbaric levobupivicaine as the sub-arachnoid block additives instead of regular 0.5% hyperbaric bupivacaine. Dexmedetomidine had a significantly prolonged duration of action, providing adequate postoperative analgesia. It also resulted in a delayed first rescue analgesic request time and minimal increase in sedation while showing similar onset, peak level, and hemodynamic changes compared to adding 50 µg clonidine to the same block.
Liu et al. (14) used dexmedetomidine 5 µg along with 0.5% hyperbaric bupivacaine in the sub-arachnoid block, proving that it prolonged sensory and motor blocks and delayed first analgesic requisite postoperatively.
Jagtap and Bhure (15) revealed that dexmedetomidine has a longer duration of action with effective postoperative analgesia and fewer side effects when compared to fentanyl. Hence, to prevent the undesirable effects of opioids, our study used alpha 2 agonists dexmedetomidine and Clonidine and compared their analgesic efficacies.
Mohammed et al. (16) revealed that 5µg dexmedetomidine is the suitable additive to prolong sensory and motor blocks and extend analgesia compared to fentanyl 25 µg. Therefore, we compared two alpha agonists as additives to 0.5% hyperbaric Levobupivacaine for the Sub-Arachnoid block. Dexmedetomidine had a better analgesic profile, postoperative analgesia, sedation, and almost similar hemodynamic changes than clonidine.
Shaik et al. (17) found that dexmedetomidine had better sedation and prolonged analgesia than clonidine in combined spinal and epidural anesthesia, with the same side effects. In line with this, our study compared the analgesic efficacy, postoperative analgesic requirement, sedation, and hemodynamic stability of alpha 2 agonists dexmedetomidine and clonidine when given intrathecally with 0.5% hyperbaric Levobupivacaine.
Akhondzadeh et al. (18) revealed that, compared with fentanyl as an additive in epidural anesthesia, dexmedetomidine had earlier onset, prolonged sensory-motor blockade, and desired sedation with fewer side effects. Our study assessed dexmedetomidine as an adjuvant to intra-thecal 0.5% hyperbaric Levobupivacaine and compared it with clonidine.
Gautham et al. (19) proved that clonidine 30 µg with intrathecal 0.5% isobaric Levobupivacaine improved hemodynamic stability, shortened the onset of sensory and motor blockades, and decreased postoperative rescue analgesia requirements with comfortable sedation. Hence, we added dexmedetomidine or clonidine to intrathecal 0.5% hyperbaric Levobupivacaine with a slightly higher dosage of low-dose spectrum alpha 2 agonists to compare their efficacies. Dexmedetomidine prolonged analgesia and decreased postoperative rescue analgesic requirements and desired sedation.
Kataria et al. (20) demonstrated that the addition of low-dose dexmedetomidine 3 µg to 0.5% isobaric levobupivicaine (15 mg) in the sub-arachnoid block had significantly prolonged action, postoperative analgesia, and fewer rescue analgesics. Mishra and Agarwal (21) revealed that adding dexmedetomidine 3 µg to intrathecal 0.5% isobaric Levobupivacaine had desired postoperative analgesia and an ideal intrathecal additive. Thus, our study used the same procedure, except for using 0.5% hyperbaric Levobupivacaine.
Jain et al. (22) added dexmedetomidine 5 µg to 0.5% hyperbaric levobupivicaine (3.5 mL) in the sub-arachnoid block, which had a significantly prolonged action, postoperative analgesia, and delayed first analgesic request. Hence, our study used dexmedetomidine 5 µg, showing a prolonged duration of the blockade and delayed rescue analgesic requirement and frequency with desired sedation.
4.1. Conclusions
To conclude, our study, comparing dexmedetomidine 5 µg and clonidine 50 µg administered intrathecally along with 0.5% hyperbaric levobupivicaine (15 mg), revealed the equipotent least hemodynamic instability in both. Dexmedetomidine 5 µg prolonged the duration of the sub-arachnoid block, provided adequate postoperative analgesia, delayed the first rescue analgesic request, reduced subsequent analgesic requirements, and provided the desired level of sedation compared to clonidine 50 µg.