1. Background
In recent years, the elderly population has grown, boosting demands for surgeries pertaining to these people (1). The better the pain management in the perioperative phase, the better and more successful pain relief and faster postoperative recovery (2). Preemptive analgesia depends on the prevention of central sensitization during surgery, which results in postoperative hypersensitivity (3).
Anesthesiologists aim to decrease perioperative pain with fewer complications through regional analgesia techniques that eliminate or decrease dependence on traditional opioids and postoperative delirium. Novel analgesic techniques encourage many elderlies to undergo major surgeries (4, 5).
Preemptive ultrasound-guided pericapsular nerve group (PENG) block was first described by Giron-Arango et al. (6) as a novel promising regional analgesia procedure that spares the motor function of the hip joint by blocking the articular branches of the obturator and femoral and accessory obturator nerves via injecting the local anesthetic between the superior pubic ramus and psoas muscles (6). This technique has been suggested as an effective alternative regional anesthetic approach for managing acute pain following hip fracture (7-9).
In 2016, erector spinae plane block (ESPB) was widely used at the thoracic vertebral level by ultrasound-guided injection of the local anesthetic between the erector spinae muscle and the transverse process of the thoracic vertebrae (10). In the only case study published in 2018, lumber ESPB (L-ESPB) was used as postoperative analgesia after hip arthroplasty (11), where the local anesthetic injected at the fourth lumbar spine level (L4) was spread toward cephalic and caudal directions in the paravertebral space, delivering satisfactory hip analgesia (11).
2. Objectives
An ideal regional analgesic technique in the elderly undergoing hip fracture surgery would be the one that reduces pain scores during spinal anesthesia, prolongs the time for needing postoperative analgesia, and allows good spine positioning. So, the primary aim of the present study was to compare the analgesic effects of PENG block and L-ESPB block in the elderly undergoing hip arthroplasty by measuring the time needed for the first postoperative rescue analgesia. Also, secondary outcomes included the oneset of sensory block, block performance time, ease of spinal positioning (EOSP), block complications (such as hypotension, nausea & vomiting), and patient satisfaction.
3. Methods
The present study was a prospective interventional single-blinded, randomized controlled study. Institutional review board approval (ZUIRB#: 6818/14-1-2021) was obtained on 14-1-2021, and the study was registered at clinicaltrials.gov (NCT04899388) on 1/06/2021. The protocol was in accordance with the Declaration of Helsinki guidelines. Patients were enrolled from July 2021 to December 2021.
Sixty-nine elderly patients undergoing elective hip arthroplasty, with ages of 65 to 75 years old, American Society of Anesthesiologists Physical Status (ASA-PS) II and III, and a body mass index (BMI) of 25 to 30 kg/m2, were enrolled. Informed written consent was obtained from all patients.
Patients with mental health problems, a history of trauma or multiple fractures, uncontrolled hypertension, diabetes, coagulopathies, preexisting advanced diseases of the kidney or liver, heart disease, allergies (or other contraindications) to administrated drugs, as well as those with prolonged using of opioids, were excluded from the study.
However, group assignments and blocks were obscure to the observer, and an independent anesthesiologist recorded the primary and secondary outcomes. The surgeon and the attending anesthesiologist were not blinded. The primary outcome of the present study was the time to the first postoperative rescue analgesia, and secondary measurements were the oneset of sensory block, block performance time, EOSP scores, complications (such as hypotension, nausea, and vomiting), and patient satisfaction.
Patients eligible to join the study were contacted before the surgery to conduct a detailed clinical history taking and physical examination. On a numeric rating scale (NRS) of 0-10, the patients were taught and instructed to quantify their pain intensity (12), where 0 indicated no pain, and ten was equal to maximum pain. The NRS score was recorded at the baseline and after the surgery. Patients were kept nil prior to the procedure (6 - 8 hours for solid meals and 2 hours for fluids).
After transferring the patient to the operating room, intravenous access was secured by an 18-G cannula. Standard monitoring equipment included an electrocardiogram device, pulse oximetry, and a noninvasive blood pressure monitoring device. The baseline parameters were recorded. All patients received oxygen supplementation by nasal cannula at the rate of 4 L/min and were premeditated with 0.03 mg/kg IV midazolam.
A computer-generated randomization table was used for random allocation. Before positioning for spinal anesthesia, patients were allocated to either of the three following groups (n = 23 per group):
(1) The PENG group, where patients received PENG block using 20 mL of bupivacaine 0.25%.
(2) The L-ESPS group, where patients received L-ESPS block using 20 mL of Bupivacaine 0.25%.
(3) The control group, in which patients received spinal anesthesia only.
3.1. Block Techniques
All blocks were carried out using low-frequency convex Sonosite M Turbo ultrasonography (FUJIFIM Sonosite, Inc., Bothell, WA, USA) after skin sterilization and draping.
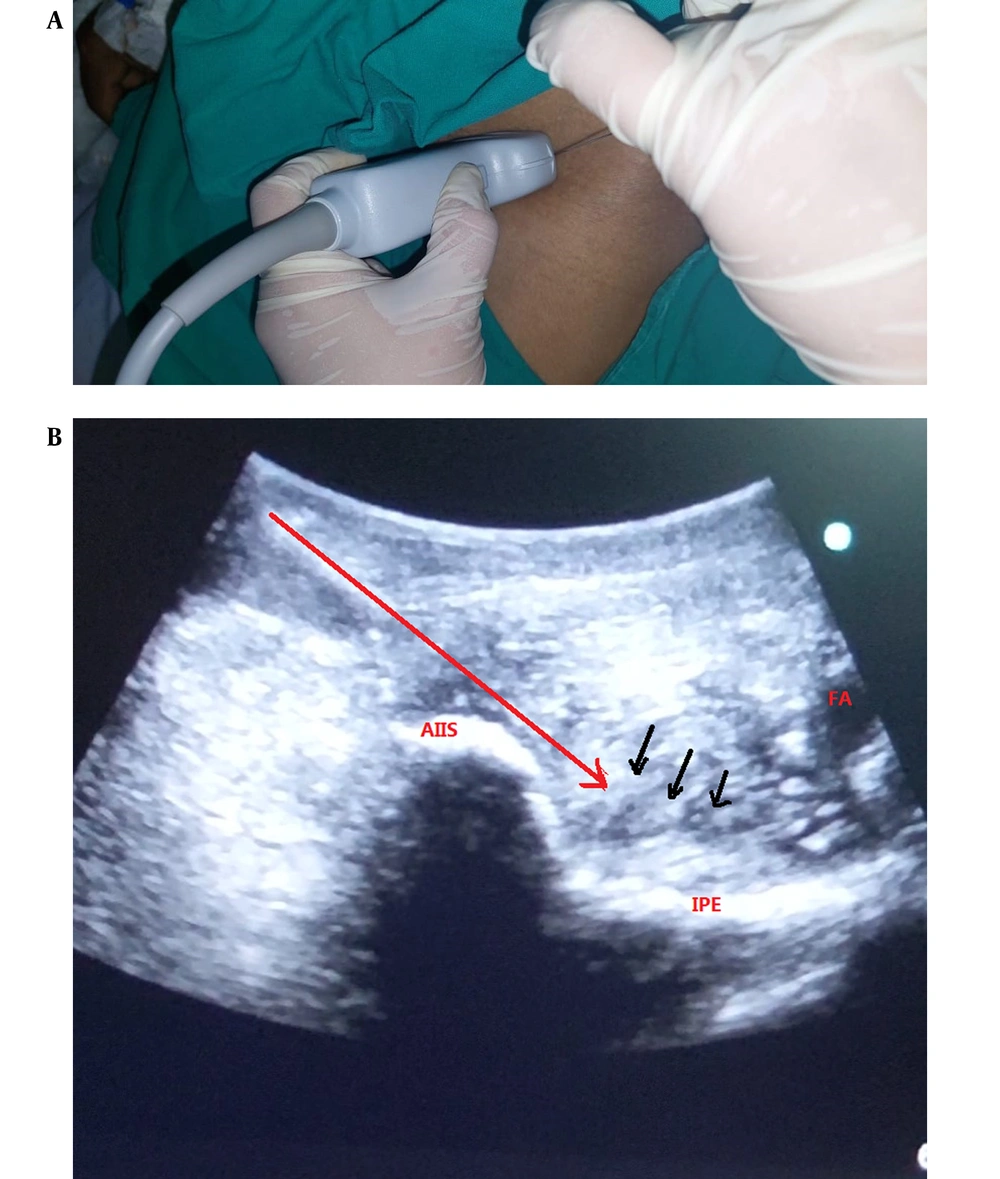
PENG block: While the patient was laying in the supine position, the probe was initially placed in a transverse plane above the anterior superior iliac spine at the ipsilateral surgical site and then was rotated counterclockwise about 45 degrees to line up with the pubic ramus. The iliopubic eminence, iliopsoas muscle and tendon, femoral artery, and pectineus muscle were all visible in this view (Figure 1A). Using an in-plane technique from lateral to medial, a 22-gauge 80-mm needle was placed in the musculofascial plane between the psoas tendon (anterior) and the pubic ramus (posterior) (6). The local anesthetic medication was delivered after negative aspiration while looking out for proper fluid distribution at a total volume of 20 mL of Bupivacaine 0.25% (Figure 1B).
(A) The site of ultrasound probe placement in PENG. (B) Ultrasound-guided pericapsular nerve group (PENG) block. Red arrows: The lateral-to-medial insertion of the needle, AIIS: Anterior inferior iliac spine, IPE: Ilio-pubic eminence, FA: Femoral artery, Black arrow: The spread of local anesthetics.
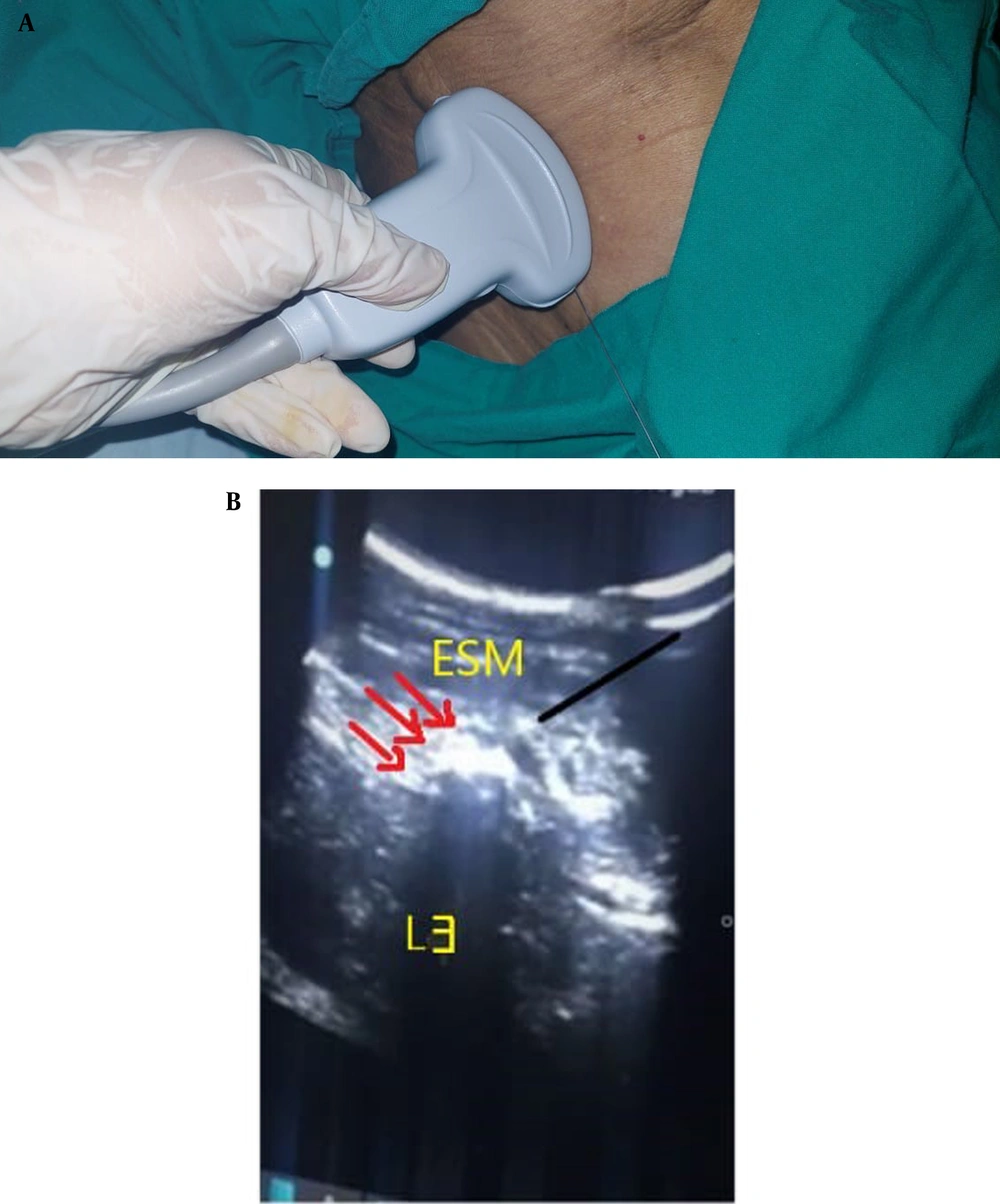
L-ESPB block: The patient was positioned in the lateral decubitus posture at the ipsilateral surgical site. The convex USG transducer was moved from the midline to the side of the operation and positioned 4 – 6 cm lateral to the L3 spinous process on a longitudinal parasagittal plane. The needle was advanced using the in-plane superior-to-inferior approach until the tip was introduced up to the plane anterior to the "erector spinae muscle" and the posterior surface of the L3 transverse process (Figure 2A). For hydro-dissection, 0.5 - 1 mL of normal saline 0.9% was administered to ensure the proper placement of the needle (11). If there was any resistance during administering local anesthesia, the needle’s position was modified by drawing it back a few millimeters. Bupivacaine 0.25% (20 mL) was delivered between the transverse process and the erector spinae muscle (Figure 2B).
The block performance time was recorded as the time from the placement of the ultrasound probe on the patient’s skin to the end of the local anesthetic injection. Also, the oneset of the sensory block was recorded as the time from the end of the injection of local anesthetic (bupivacaine) to the loss of pinprick sensation using a sterile 25-G needle in the operation field.
Ease of Spinal Positioning (EOSP) (13) was evaluated and recorded on a scale from zero to three (zero = unable to be positioned; one = abnormal posture of the patient due to pain requiring support for positioning; two = mild discomfort but no need for assisted positioning; three = optimal condition where the patient could sit without feeling pain).
If the patient’s EOSP was less than 2, an IV dose of fentanyl (20 µg) was administered every five minutes until the NRS score reached 2. The number of patients who needed fentanyl was recorded. Then patients were permitted to be seated for spinal anesthesia. A 26-G pencil-point needle was used to deliver spinal anesthesia in all groups using heavy bupivacaine 0.5% (1.8 mL) and fentanyl (20 µg, 0.4 mL) under strict sterile conditions.
After the end of the surgery and in the recovery room, pain intensity was assessed using a 10-point NRS [(0 = no pain, 10 = worst imaginable pain), 1 – 3: Mild pain (nagging, annoying, slightly interfering with activities of daily living (ADLs), 4 – 6: Moderate pain (significantly interfering with ADLs, 7 – 10: Severe pain (disabling, unable to perform ADLs)]. Pain intensity was measured both at rest and during movement (i.e., 45-degree passive flexion of the hip with flexed ipsilateral knee) 30 minutes after the end of the surgery, as well as 3, 6, 12, and 24 hours postoperatively. Postoperative analgesia was administered to all patients (IV administration of 1 g paracetamol every eight hours). If the postoperative NRS score was ≥ 3, rescue analgesia was administered (2 mg, IV bolus morphine) every 10 min until the NRS score fell below 3. The time (minutes) to the first episode of calling for rescue analgesia (morphine) was recorded in patients reporting NRS scores ≥ 3. The total dose of the rescue analgesic (morphine) consumed during the first 24 hours post-operation was recorded.
Patient satisfaction was evaluated using a 10-point satisfaction scale (0 = unsatisfied and 10 = most satisfied), 0 - 3 (not satisfied), 4 - 6 (partly satisfied), and 7 - 10 (highly satisfied) (14). Postoperative complications, such as nausea, vomiting, hypotension, bradycardia, and hematoma, were recorded and managed accordingly.
3.2. Sample Size
According to a previous study (15), assuming a mean time (hours) to the first call for opioids as 12 ± 6.7 in the PENG group and 6 ± 4.9 in the control group, 90% study power, 95% confidence interval (CI), and a drop-out rate of 10%, the sample size was estimated as n = 23 patients in each group using the (Open Epi) database.
3.3. Statistical Analysis
All data were collected, tabulated, and statistically analyzed using SPSS for Windows, Version 23.0. (Armonk, NY: IBM Corp., released 2015). Quantitative data were expressed as mean ± SD & median (range), and qualitative data were expressed as frequency and percentage. The student t-test and Mann-Whitney U test were used to compare normally- and non-normally-distributed variables, respectively, between the two groups. The ANOVA and Kruskal-Wallis tests were used to compare normally- and non-normally-distributed variables, respectively, between more than two groups, followed by the Least significant difference to ascertain which two groups are different. The distribution of categorical variables was compared using the chi-square test. All the tests were two-sided at a P-value of < 0.05 as the statistical significance level. A P-value < 0.001 was considered highly statistically significant, and a P-value ≥ 0.05 was considered statistically insignificant.
4. Results
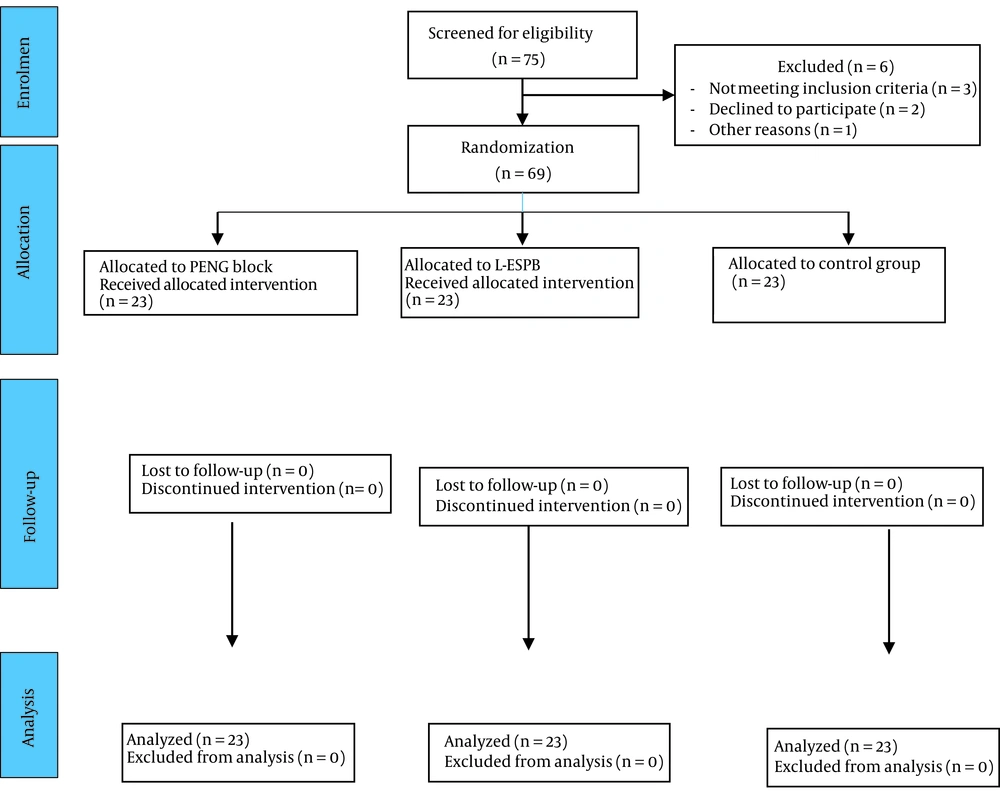
Sixty-nine patients were enrolled in the present study (Figure 3).
The patients’ characteristics (age, sex, BMI, and ASA) and the duration and type of surgery were comparable among the groups (Table 1).
| Characteristics | PENG Group (n = 23) | L-ESPS Group (n = 23) | Control Group (n = 23) | P-Value b |
|---|---|---|---|---|
| Age, y | 71.1 ± 4.3 | 72.4 ± 5.1 | 72.6 ± 4.6 | 0.456 c |
| Sex | 0.493 d | |||
| Female | 15 (65.2) | 11 (47.8) | 13 (56.5) | |
| Male | 8 (34.8) | 12 (52.2) | 10 (43.5) | |
| BMI, kg/m2 | 26.9 ± 1.9 | 26.5 ± 1.8 | 23.3 ± 1.8 | 0.324 c |
| ASA ps. | 0.461 d | |||
| II | 15 (65.2) | 14 (60.9) | 11 (47.8) | |
| III | 8 (34.8) | 9 (39.1) | 12 (52.2) | |
| Duration of surgery, min | 138.3 ± 19.7 | 146 ± 22.9 | 146.9 ± 20.6 | 0.313 V |
| Type of surgery | 0.435 d | |||
| Partial hip prosthesis | 13 (56.5) | 12 (52.1) | 13 (56.5) | |
| Total hip prosthesis | 10 (43.4) | 11 (47.8) | 10 (43.4) |
Abbreviations: N, total number of patients in each group; BMI, body mass index; ASA ps., American Society of Anesthesiologists physical status.
a Data is expressed as mean ± SD or number (%). P > 0.05 = insignificant. P1: PENG vs. L-ESPS, P2: PENG vs. control, and P3: L-ESPS vs. control. test,
b Kruskal Wallis Test
c ANOVA
d Chi-square test
The time to the first administration of the rescue analgesic (morphine) was significantly more prolonged in the PENG group (13.3 ± 3.5 h) compared to the L-ESPB (2.6 ± 0.4 h) and control groups (P = 0.001). The total dose of morphine was significantly lower in the PENG group (4.1 ± 1.6 mg) compared to the L-ESPB (8.4 ± 1.7 mg) and control (12.7 ± 1.9 mg) groups (p = 0.001) (Table 2).
| Variables | PENG Group (n = 23) | L-ESPS Group (n = 23) | Control Group (n = 23) | P-Value b | P1 | P2 | P3 |
|---|---|---|---|---|---|---|---|
| Time to the first rescue analgesic, h | 13.3 ± 3.5 | 9.5 ± 2.3 | 2.6 ± 0.4 | 0.001 | 0.001 | 0.001 | 0.001 |
| EOSP | < 0.001 c | < 0.001 | 0.001 | 0.01 | |||
| 0 | 0 (0.0) | 0 (0.0) | 10 (43.5) | ||||
| 1 | 0 (0.0) | 9 (39.1) | 13 (56.5) | ||||
| 2 | 13 (56.5) | 14 (60.9) | 0 (0.0) | ||||
| 3 | 10 (43.5) | 0 (0.0) | 0 (0.0) | ||||
| Block performance time, s | 182.6 ± 19.7 | 229.2 ± 50.7 | ---- | < 0.001 | --- | -- | -- |
| Onset of sensory block, min | 7.2 ± 1.8 | 26.3 ± 3.2 | - | 0.0001 d | --- | -- | -- |
| Total dose of analgesic (morphine) in 24 h, mg | 4.1 ± 1.6 | 8.4 ± 1.7 | 12.7 ± 1.9 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Patient satisfaction | 8 (6 - 10) | 5 (4 - 7) | 4 (0 - 7) | < 0.001 e | < 0.001 | 0.085 | < 0.001 |
Abbreviations: P1, PENG vs. L-ESPS; P2, PENG vs. control, and P3, L-ESPS vs. control n = total number of subjects in each group; EOSP, ease of spinal positioning.
a Data is expressed as mean ± SD, No. (%), or median (range). P < 0.05 = significant.
b Kruskal Wallis Test
c Chi-square test
d Student's t-test
e ANOVA
The block performance time was significantly shorter in the PENG group (182.6 ± 19.7 sec) compared to the L-ESPB group (229.2 ± 50.7 sec) (P < 0.001). Moreover, the duration of sensory block was significantly shorter in the PENG group (7.2 ± 1.8 min) compared to the L-ESPB group (26.3 ± 3.2 min) (P < 0.001) (Table 2).
The mean EOSP score was significantly higher in the PENG group when compared to the L-ESPB group (P < 0.001). Patients in the control group had significantly lower EOSP scores compared to the PENG and L-ESPB groups (P = 0.001 and 0.01, respectively) (Table 2).
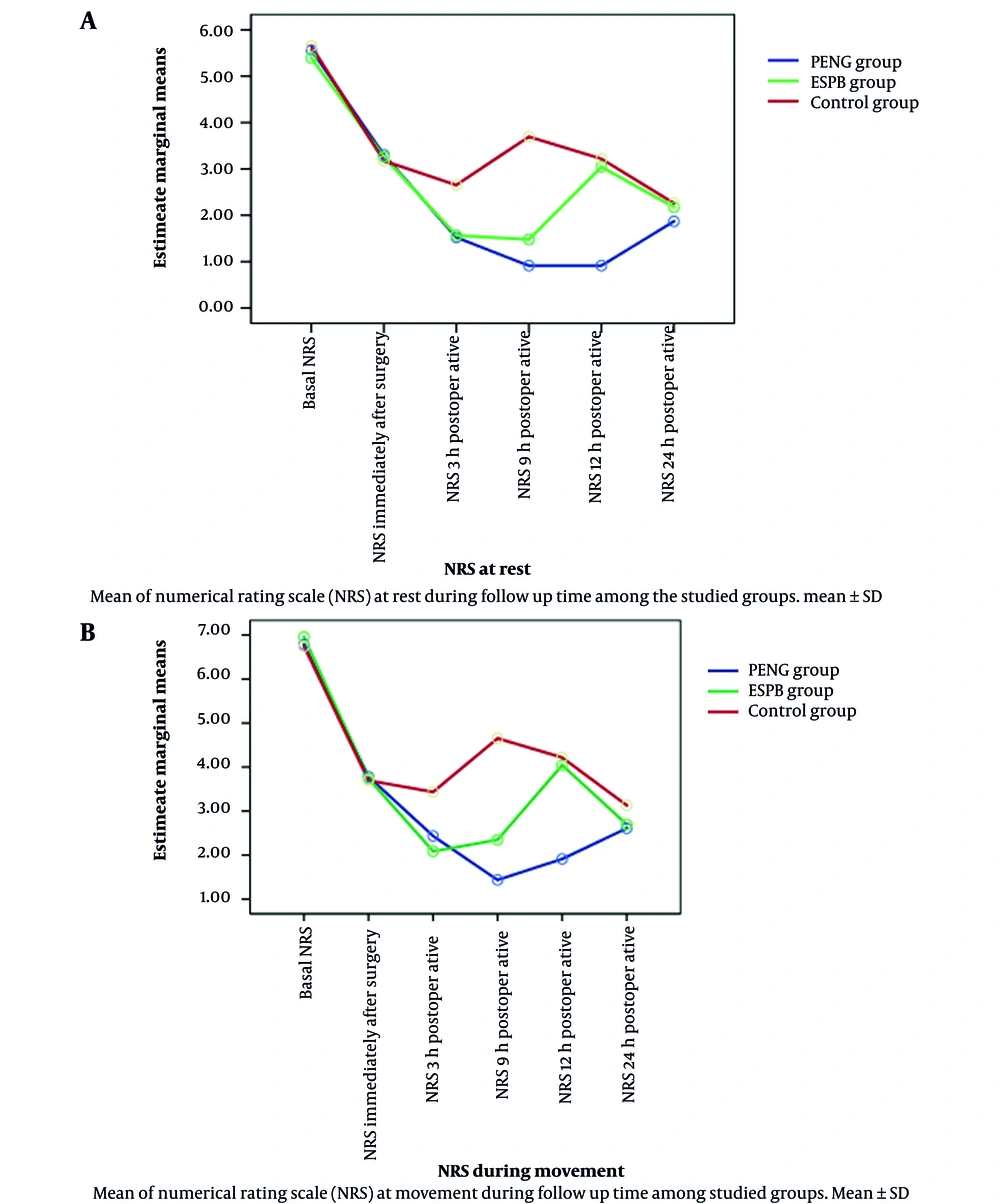
The NRS scores at rest and during movement at 3, 6, and 12 hours postoperatively were significantly lower in the PENG group compared to the L-ESPB group (P = 0.001). Moreover, NRS scores were significantly higher in the control group compared to the interventional groups at all measurement points except immediately after the surgery and at 24 hours postoperatively, when the three studied groups were comparable (P > 0.500) (Figure 4).
The median patient satisfaction score was significantly higher in the PENG group compared to the L-ESPB group; however, the patient satisfaction score was significantly lower in the control group compared to both interventional groups (Table 2).
With regard to block placement or signs suggesting local anesthetic toxicity, no complications were observed in the interventional groups. Only two patients in the control group complained of nausea & vomiting.
5. Discussion
The present study demonstrated that preemptive PENG block significantly prolonged the duration of analgesia and allowed easier spinal positioning compared to L-ESPB in elderly patients undergoing hip arthroplasty. Elderly patients scheduled for hip arthroplasty under spinal anesthesia are anticipated to withstand the majority of pain resulting from positional changes needed for spinal anesthesia (16); however, they need effective and safe preemptive analgesia as they usually suffer from comorbidities such as hypertension and respiratory and heart diseases (17).
Neuraxial anesthesia is a well-accepted and recommended option to decrease perioperative adverse effects in the elderly (18), but its insufficient duration is one of the drawbacks limiting its use in hip arthroplasty surgeries (19). The current study is the first prospective trial to investigate the ability of two different recently recommended peripheral nerve block techniques (PENG block and LESPB) in combination with spinal anesthesia to prolong anesthesia duration in elderly patients undergoing hip arthroplasty. Our results revealed that the time to the first rescue analgesic was significantly longer in the PENG group (13.3 ± 3.5 h) compared to the L-ESPB (9.5 ± 2.3 h) and control (2.6 ± 0.4 h) groups.
In agreement with the present study’s results, Pascarella et al. (15) reported that in the PENG group, the mean time to the first opioid use was 12 hours compared to six hours in the control group in patients undergoing total hip arthroplasty. Also, Ince and Kilicaslan (20) specified that PENG block could produce effective postoperative analgesia in elderly patients undergoing hip arthroplasty and underlined that the combination of erector spinae plane block and PENG prolonged the duration of erector spinae plane block.
In the present study, the mean EOSP score was significantly higher in the PENG group compared to the L-ESPB and control groups. This was in accordance with Alrefaey and Abouelela (13), reporting that preoperative PENG block was effective in alleviating positioning-related pain during spinal anesthesia and improving the satisfaction of both anesthesiologists and patients. In a case study by Acharya and Lamsal (21), it was concluded that PENG block provided excellent analgesic effects during patient placement throughout the procedures, mentioning that patients could sit up without any difficulty and need no assistance during the subarachnoid block. Moreover, Jadon et al. (22) noticed no difficulty during sitting of the patients with hip fractures undergoing hip surgery under spinal anesthesia and preoperative PENG block; the median EOSP score was three, and these findings were in agreement with the results of the current study.
In the current study, the block performance time was significantly shorter in the PENG group compared to the L-ESPB group. In agreement, Luftig et al. (23) reported that the PENG block was highly effective for pain relief in trauma patients with acute pelvic fractures in the emergency department because of its fast action and high analgesic capacity while preserving motor function.
We also observed that the time to the onset of sensory block was significantly shorter in the PENG group (7.2 ± 1.8 min) compared to the L-ESPB group (26.3 ± 3.2 min). Ahiskalioglu et al. (24) reported that the median onset of sensory block in the L-ESPB group was nearly 30 minutes, which was in accordance with our observation.
In the present study, PENG block significantly reduced the NRS pain score at 3, 6, and 12 hours after the procedure, evidenced by less need for analgesics compared to the L‑ESPB block and control groups. In fact, the hip joint is innervated by both the lumbar (L1-L4) and sacral (L4-S4) plexuses, while its sensory innervation comes from femoral, obturator, and sciatic nerves, as well as the neurons of the quadratus femoris and superior gluteal nerve (25). The hip joint is also supplied by the articular branches of the femoral, obturator, and accessory obturator nerves (AON). During the PENG block, these articular branches supplying the hip are suppressed.
Short et al. (26) confirmed that the anterior hip capsule was innervated by the high branches of both femoral and obturator nerves, suggesting that the anterior hip capsule, but not posterior and inferior capsules, could receive the majority of sensory innervation (27). Furthermore, earlier histological research has discovered that the anterior capsule is mostly comprised of nociceptive fibers, whereas the posterior capsule is mostly made up of mechanoreceptors (28). In accordance with these facts, PENG block was a more effective and advantageous analgesic technique during hip surgery over L-ESPB in terms of wider and more complete coverage of sensory nerves innervating the hip without motor blockage, allowing early patient mobilization and participation in rehabilitation.
Some case reports case series, and small clinical trials have recently demonstrated the effectiveness of LESP block analgesia in hip surgery (24, 29). The clinical mechanism of the analgesic effects of ESP block was explained by Bonvicini et al. (30), who reported that the wide spread of the local anesthetic during ESP block resembled that in the paravertebral block, evidenced by tracking the distribution of a dye injected at the site of local anesthetic administration during ESP block in corpses. The dye was observed to diffuse into the dorsal rami of spinal nerves and blood vessels, reaching the paravertebral space through the costotransverse foramen.
The present study revealed that the highest level of patient satisfaction was related to the PENG group compared to the L-ESPB and control groups, which was in accordance with the significantly highest EOSP in the PENG group compared to the L-ESPB and control groups. Moreover, the easily identifiable sonographic landmarks of the PENG block during supine positioning could facilitate its technical performance.
5.1. Limitations
A few studies have been conducted in this field, which hindered us from drawing more robust conclusions. Although the PENG block delivers analgesia with regard to the anterior hip capsule, which receives most of the sensory innervation, we could not be certain about the role of the posterior capsule, which is innervated by quadratus femoris and superior gluteal nerves originating in the sacral plexus (22). It is advisable for future studies to examine the outcomes of combining PENG block with other blocks, such as sciatic block or local infiltration analgesia techniques, to ensure complete hip capsule analgesia. Moreover, we recommend investigating the effectiveness of dual ESPB + PENG as an analgesic technique.
5.2. Conclusions
Preemptive pericapsular nerve group block delivered a longer duration of postoperative analgesia and easier spinal positioning compared to L-ESPB in elderly patients undergoing hip arthroplasty.