1. Introduction
Cervical radiculopathy is a common condition affecting 83 per 100,000 persons each year (1). Presenting symptoms include cervical pain with or without radiculopathic upper extremity pain, deep tendon reflex depression, headache, weakness, or vertigo. Duration and severity of symptoms directs selection of treatment modality. Common conservative treatment consists of nonsteroidal anti-inflammatory drugs (NSAIDs), anticonvulsants, muscle relaxants, and physical therapy (2). The efficacy of cervical epidural steroid injection for patients that have not responded to conservative treatment has been demonstrated (3-5). If the patient’s symptoms continue to persist after this interventional procedure, then surgical interventions may be considered.
Derby et al. report that the overall rate of complication following cervical epidural steroid injections as 5 per 1000 injections (6). Complications described as minor include vasovagal episodes, headache, rashes, worsening pain, pain, and new paresthesia. Major complications, although rare, include direct spinal cord trauma, epidural hematoma or abscess, transection of vertebral artery, and injection of the particulate steroid into a radiculomedullary artery or vertebral artery resulting in spinal cord or posterior cerebellar embolic infarction (7, 8). Subdural injection of local anesthetic and steroid represents a rare but potentially life threatening complication (2). The incidence of subdural injection is 0.8% with lumbar epidural injection and surprisingly high 1.6% - 3.2% during diagnostic myelography (9, 10).
2. Case Presentation
A 52-year-old male presented to the ambulatory surgery center for a scheduled right sided C6 - C7 interlaminar epidural steroid injection. The patient had been dealing with neck pain for the last few years, with decreased range of motion predominantly on extension, positive Spurling’s sign on the right side, decreased sensation to light touch in the C6 - C7 nerve distribution, and normal reflexes that were elicited on physical examination. He had minimal relief with medication, including NSAIDs and tramadol, and physical therapy. MRI of the cervical spine showed a posterior disc osteophyte complex that was causing mild to moderate spinal canal stenosis with severe right and moderate to severe left neural foraminal narrowing. The radiologic findings along with the positive physical exam findings were evidence that the patient could potentially benefit from a cervical epidural block.
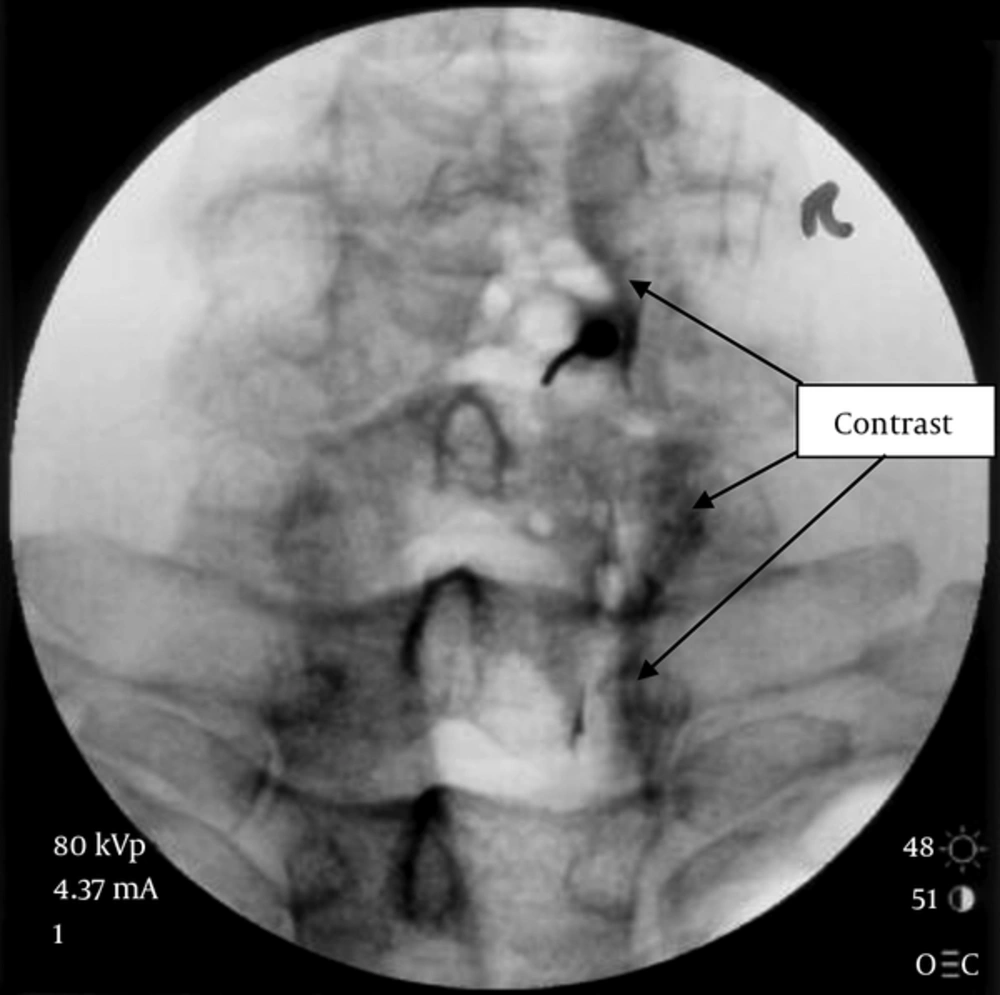
After informed consent was obtained, the patient was placed on the fluoroscopy table in the prone position with the neck in the neutral position. The right C6 - C7 epidural space was identified using fluoroscopy and a 22-gauge, 3.5 inch Tuohy was advanced to the epidural space using loss of resistance technique. Isovue contrast was used for needle localization and after confirmation of the presence of the contrast in the epidural space (Figure 1), 10 mg of dexamethasone and 2 mL of preservative free 1% lidocaine were injected.
The patient was then taken from the OR to the post anesthesia care unit (PACU) for observation. About five minutes after arrival into the PACU, the patient was noted to be anxious and hypertensive, with the systolic pressure running in the 180s mmHg and the diastolic pressure in the 100s mmHg. The patient was normotensive prior to the procedure with a blood pressure of 134/82 mmHg. In addition to the elevated blood pressure, the patient reported that he was unable to swallow and was having a subjective sensation of dizziness, and concurrent horizontal nystagmus. All other vital signs, including pulse oximetry, heart rate, respiratory rate, and temperature were all within normal limits.
The patient was reassured and after thirty minutes from the initial presentation the symptoms resolved. The patient was observed in the PACU for another thirty minutes and then was transferred to phase two of PACU and from there was discharged home with no further issues or complications. Prior to discharge, the patient did report that his neck pain felt much better at this time than before the procedure.
3. Discussion
Complications from epidural injections can present in dramatic clinical fashion. Our patient’s constellation of symptoms, including difficulty swallowing, vertigo, and horizontal nystagmus points to possible local anesthetic spread rostrally to the brainstem and lower midbrain levels. These symptoms are the likely precipitant of anxiety in our patient and the resultant hypertension, which normalized concurrently with the dissipation of those symptoms. The swallowing difficulty, horizontal nystagmus, and vertigo in our patient may be due to the effect of local anesthetic on the glossopharyngeal, abducens, and vestibulocochlear cranial nerves respectively. The glossopharyngeal cranial nerve innervates the stylopharyngeus muscle whose functions include elevating both the larynx and pharnx and dilating the pharynx which promotes swallowing (11). The vestibulocochlear cranial nerve splits into the vestibular and cochlear nerve. The vestibular nerve is responsible for innervating the vestibules and semicircular canal of the inner ear, which are structures that transmits information about balance (12). The abducens cranial nerve innervates the lateral rectus muscle which is responsible for abduction of the eyeball in the lateral direction away from the midline of the body (13). The presentation of hypertension is likely secondary to the aniety.
During the pain procedure, epidural placement of the needle is confirmed by a radiocontrast dye. However, when complications arise, the possibility of inadvertent subdural or intrathecal spread of the medication must be considered in amongst other causes in the differential diagnosis given the close geographic proximity of the anatomical structures of the spinal cord. The spinal cord and the spinal nerve proximal to the dorsal root ganglion are surrounded by a trilaminar structure that is composed of an outer layer of dense fibrous dura mater, a middle arachnoid layer of thin nonvascular tissue, and an inner pial layer of thick vascular connective tissue. As the subdural space is larger in the cervical region compared to the lumbar region, the risk for inadvertent subdural injections may also be greater in the cervical region. The subdural space typically extends from the inferior border of the second sacral vertebra into the intracranial space unlike the epidural space which typically terminates at the foramen magnum (2).
The greatest hazard of subdural injection is the small volume of local anesthetic solution required to spread cephalad leading to significant neurological and hemodynamic complications including loss of consciousness, severe hypotension, bradycardia, and cardiac arrest (14, 15).
Even with appropriate confirmation with radiocontrast dye, seemingly unrelated symptomology may potentially manifest in the patient. Although the cause may not be initially apparent, interventional pain physicians must be vigilant to the possibility of inadvertent spread of local anesthetic even after a confirmatory presence of radiographic contrast in the epidural space. Supportive treatment including hemodynamic and ventilatory support may be required.