1. Background
In pregnant females, it is difficult to perform lumbar flexion due to lumbar hyperlordosis that usually occur during pregnancy. Hyperlordosis can change the relationship between surface anatomy of vertebrae and vertebral columns. During pregnancy, due to these changes, the intervertebral spaces are narrow and can make the median approach for spinal puncture more difficult (1-3).
Filho et al. mentioned that the success rate of spinal needle placement in subarachnoid space was influenced by the anatomy of vertebrae, appropriate patient position, and the experience of the anesthesiologist. Incorrect position led to multiple insertion attempts which led to patients’ inconvenience and increased complications (4). Multiple insertion attempts were also associated with postspinal back pain (2, 3, 5). Precise identification of intervertebral space and interlaminar foramen may decrease contact between spinal needle and bone. This identification may be facilitated by decreasing lumbar lordosis during the spinal anaesthesia (2, 3, 6, 7).
Shabanian et al. reported that axillary support during sitting position might increase the intervertebral spaces. This position is called pendant position. Pendant position decreases the vertical pressure due to gravitation. Hence, this position increases the intervertebral spaces and the spinal needle may reach the subarachnoid space more accurately (8).
Pendant position is a newly introduced position for spinal anesthesia. Currently, no many studies addressed this position. Therefore, the current study aimed at comparing the pendant position with traditional sitting position regarding the success rate of 1st attempt spinal puncture, the number of spinal needle-bone contact, and duration of spinal puncture between the 2 positions among patients undergoing cesarean section.
2. Methods
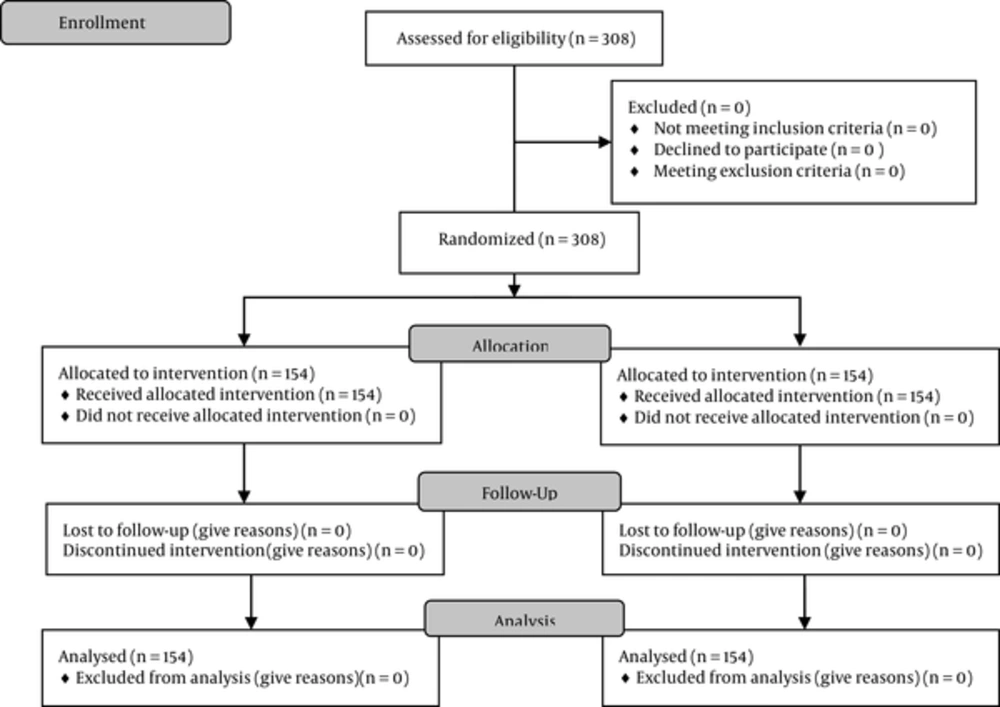
It was a non-blinded, randomized controlled trial (RCT) conducted on the patients who were the candidate for cesarean section in Budi Kemuliaan hospital, Jakarta, Indonesia, from August to October 2014. The spinal anesthesia was performed by 1 senior anesthesiology resident with more than 100 cases of spinal anesthesia experience. The protocol of the current study was approved by the ethical committee of faculty of medicine Universitas Indonesia (code number: 454/H2.F1/ETIK/2014) prior to conducting the study (Figure 1).
The current study utilized the random consecutive sampling method. Patients with pendant position were included in group A, while the ones with traditional sitting position were in group B. The inclusion criteria were the pregnant females aged 18 to 45 years, body mass index (BMI) 18 to 35 kg/m2, physical status I to III, based on American society of anesthesiologists classification (ASA). The eligible cases who were the candidate for cesarean section with spinal anesthesia were enrolled in the study after signing the informed consent form. The exclusion criteria were any contraindications for spinal anesthesia (infection on injection site, coagulation disorder, severe hypovolemia, increased intracranial pressure, aortic and/or mitral stenosis), fetal head entrapment, umbilical cord prolapse, feet presentation, eclampsia, cardiovascular disease, scoliosis, history of lumbar surgery, and impalpable intervertebral space due to thick fatty tissue or edema. The subjects were dropped out from the study if the spinal block failed or in case of partial block, then the spinal anesthesia was converted into general anesthesia.
After skin injection of local anesthetic 1 mL lidocaine 2% at L4-L5, spinal anesthesia was performed using spinal needle Quincke 27G without introducer. The needle was directed horizontally with median approach. In case of bone contact, needle was retrieved until subcutaneous tissue and put on cephalic direction (10°). The maximum bone contact was 5 times. In case of more than 5 bone contacts, the spinal needle was inserted in L3-L4. In the case of more than 5 times bone contacts, subjects were dropped out and the general anesthesia was administered.
For each case the following parameters were recorded: the number of attempts for the successful spinal puncture, the number of spinal needle-bone contacts, and the time to perform spinal puncture.
Data were analyzed by statistical package for the social sciences (SPSS) version 21.0. Numerical data were scientific in mean, with minimal and maximal values. Numerical data were analyzed by the Mann-Whitney test. Categorical data were served by relative risk (RR) with 95% confidence interval (95% CI) and analyzed by the Chi-square test.
3. Results
The current study recruited 308 subjects and divided them into Group A (n = 154) and Group B (n = 154) (Table 1).
| Group A (n = 154) | Group B (n = 154) | |
|---|---|---|
| Age, y | 31 (18 - 42) | 30 (18 - 43) |
| Body weight, kg | 58 (38 - 80) | 57 (38 - 85) |
| Body height, cm | 155 (137 - 167) | 155 (140 - 170) |
| BMI, kg/m2 | 24 (18 - 33) | 24 (18 - 33) |
| ASA physical status | ||
| II | 137 (48.9) | 143 (51.1) |
| III | 17 (60.7) | 11 (39.3) |
Demographic Data of the Study Subjects
The mean number of spinal puncture attempts in group A was 1, ranged from 1 to 3; however, the mean value was also 1 in group B, ranged from 1 to 4. Success rate of spinal puncture at 1st attempt was higher in group A than group B (92% vs. 78%). Table 2 shows that group B required longer time for the spinal puncture in comparison with group A (12 seconds vs. 9 seconds). There was a significant difference between the groups regarding the number of attempts and the time for successful spinal puncture (P value < 0.001) (Table 3).
| First Attempt, % | Non-First Attempt, % | P Value | RR | 95%CI | |
|---|---|---|---|---|---|
| Group A | 142 (92) | 12 (8) | 0.0007a | 1.17 | 1.07 - 1.29 |
| Group B | 121 (78) | 33 (22) |
The Relationship Between the Positions and Success Rate of Puncture Attempts
The number of spinal needle-bone contacts was higher in group A than group B (54% vs. 35%). Table 4 shows that group A had 1.56 higher risk of no spinal needle-bone contact in comparison with Group B (P value < 0.005).
| No Contacts, % | Spinal Needle-Bone Contacts, % | P Value | RR | 95%CI | |
|---|---|---|---|---|---|
| Group A | 84 (54) | 70 (46) | 0.0005a | 1.56 | 1.2 - 2.02 |
| Group B | 54 (35) | 100 (65) |
The Relationship Between Positions and Spinal Needle-Bone Contacts
4. Discussion
It was a pilot study on pendant position to measure the success rate of spinal puncture in Indonesian pregnant females. Indonesian population has middle-average body height, and this condition leads to narrower intervertebral spaces in comparison with the Caucasian population. Narrow intervertebral spaces and pregnancy might increase the difficulty during spinal anesthesia, especially in median approach spinal needle insertion. Grau et al. mentioned that the mean of intervertebral spaces for pregnant females was 10.7 mm, while in non-pregnant females it was 11.6 mm (P value < 0.006) (9). However, no study mentioned the size of intervertebral spaces among Indonesian population (10, 11).
The current study found that the success rate of spinal puncture in the 1st attempt in pendant position was significantly higher (P value < 0.05) in comparison with that of traditional sitting position (92% vs. 78%). Patients with pendant position had 1.17 times higher chance to achieve 1st attempt success during spinal puncture in comparison with the ones with traditional sitting position (P value < 0.05).
Patients with pendant position had significantly lower spinal needle-bone contacts in comparison with the ones with traditional sitting position (P value < 0.05). There were 54% and 35% successful punctures without bone contact in Groups A and B, respectively. Patients with pendant position had 1.56 times higher chance not to encounter bone contact in comparison with the subjects with traditional sitting position.
Spinal needle-bone contact was defined as the number of contacts between the spinal needle and hard surface (bone) during the spinal puncture, which might influence the spinal needle movement (6, 7). The current study limited the spinal needle-bone contacts to 5 times on 1 intervertebral space. The spinal needle insertion was changed to intervertebral space L3-L4; in case of more than 5 spinal needle-bone contacts in intervertebral L4-L5. In case of bone contact more than 5 times in intervertebral space L3-L4, the spinal needle insertion was changed to intervertebral L5-S1. One attempt was defined as a puncture performed from the skin surface. Withdrawing subcutaneously and redirecting the needle after unsuccessful attempts without drawing out of skin was still considered as one spinal puncture attempt. There was no maximum limitation for the number of spinal needle-bone contacts and attempts. Fewer number of spinal needle-bone contacts in the pendant position group might be influenced by widening of intervertebral spaces due to gravitation effect.
Spinal needle-bone contact during spinal anesthesia might increase the inconvenience of the patient and increase postspinal back pain incidence. The complications following frequent spinal needle-bone contact were associated with periosteal trauma (12). Unfortunately, the study did not conduct long-term follow-up to measure the pain postspinal anesthesia.
The current study showed that pendant position in pregnant patients had significantly higher success rate in the 1st attempt spinal puncture, less spinal needle-bone contact, and shorter time of spinal needle insertion puncture compared to the traditional sitting position, however, further studies are still needed to recommend the pendant position as an option in failed spinal anesthesia under traditional sitting position. Failed spinal anesthesia cases were not only caused by patient’s position. Other factors such as patient’s anatomical structure, anesthetist’s experiences, and utilization of introducer were also influential.
The current study did not utilize the introducer during the spinal puncture needle placement. Introducer might decrease the number of spinal needle contact with the bone. Brooks et al. mentioned that patients who underwent spinal anesthesia without introducer had multiple insertion attempts in comparison to the ones with introducer (13).
The current study found that the time required for spinal puncture in pendant position was significantly shorter than that of the traditional sitting position (9 seconds vs. 12 seconds, P value < 0.05). No literature mentioned the ideal time to conduct spinal needle insertion. However, both 9 and 12 seconds were considerably acceptable. The duration of spinal puncture was measured from the injection of spinal needle through the skin until reaching to the subarachnoid space, confirmed by the presence of free flow cerebrospinal fluid (CSF) in the spinal needle connector. In the current study, the preparation time needed for the patient was not measured. However, patients with pendant position might require longer preparation time, because they required adjustment for the support for optimal position.
Some studies mentioned that a successful spinal anesthesia could be assessed by the motoric block scoring. However, the current study defined that spinal anesthesia was successful if the presence of spinal needle in subarachnoid space confirmed by clear and free outflow of CSF from spinal needle, and good CSF aspiration with no blood (7). If blood was present in the spinal needle connector, the spinal needle should be withdrawn for 1 mm. This maneuver was done repeatedly if necessary, until there was no blood, and free flow CSF and good CSF aspiration were observed. The current study did not measure the success of spinal anesthesia with the local anesthetic agent factor, the block level, and the side effect of local anesthetic agents. All spinal anesthesia inductions in the 2 groups were successfully worked as single modality anesthesia for caesarean section. There was no partial block or conversion to general anesthesia in the 2 groups.
The limitation of the current study was the lumbar intervertebral space determined only by palpating the point between the right and left iliac crests (the Tuffier line). However, the point was not confirmed with ultrasound. Pregnant females might also have changes of anatomical landmark, such as shifting of the Tuffier line to the cephalic direction. Therefore, the location of spinal needle insertion might differ from the true intervertebral level. The effect of pendant position on intervertebral spaces was not proven by radiologic study. Therefore, there was no sufficient basic data.
4.1. Conclusions
The current study concluded that in pregnant females, pendant position had significantly higher success rate for the 1st attempt spinal puncture, less spinal needle-bone contact, and shorter duration of spinal needle insertion puncture compared to those of the traditional sitting position.