1. Background
Carpal tunnel syndrome (CTS) is a common nerve entrapment syndrome at wrist (1). It is a debilitating condition occurring in 3.8% of the population, with a reported incidence rate of up to 276:100000 per year and up to 9.2% and 6% prevalence in women and men, respectively. It is more common in women and usually occurs bilaterally, while the peak age of involvement is 40 - 60 years (2). This syndrome can cause pain and paresthesia with regional loss of sense in the area innervated by the median nerve. Long-term involvement may lead to permanent damage of the nerve together with atrophy of the thenar musculature, leading to limited strength in hand grip (3-5). The entire various medical, surgical, or other interventional CTS treatment modalities mainly focus on reduction of nerve compression in the carpal tunnel. The most important non-surgical methods are splinting, steroid injections, and laser therapy (6, 7). Since these methods have relative success and transient effects in mild and moderate cases, we are facing with growing variety of physical and medical treatments in this issue. Employing ultrasound, bioptron, acupuncture, shockwave, diathermy as well as injection of insulin and progesterone are some of the newer approaches to treatment of this syndrome; while the effectiveness of some of these modalities is still a matter of debate (8-12). A number of researchers have turned their attention to manage CTS through manual therapy (13, 14), which results in less tissue adhesion and increased wrist mobility, while improving the CTS signs and symptoms (15). A study by Rincon et al., in 2012, demonstrated that manual therapy leads to significant reduction in pain (16). Butler et al., suggested a hypothesis, which may explain the improvement seen after treating the patients with different methods of manual therapy (17). The limited researches on manual therapy techniques, which include soft tissue mobilization (STM), carpal bone mobilization, or median nerve mobilization, indicated a tendency toward clinical improvements of the signs and symptoms of CTS (18). A few other studies have assessed the effect of wrist mobilization on CTS. One of the carpal mobilization techniques is intermittent dorsal (posterior ) and volar (anterior) glide. It may be more effective than others techniques. This procedure, which mobilizes the components of carpal tunnel (hamate and scaphoid bones as border and flexor retinaculum as roof of this tunnel), can cause changes in the pressure on the nerve and subsequently reduction of any intra-neural edema (18). Therefore, we decided to study the effectiveness of this mobilization technique (scaphoid and hamate) on the pain, symptoms, functionality, and electrophysiologic findings in patients with CTS.
2. Methods
Female patients who had been visited at physical medicine and rehabilitation clinic of Shahid Modarres hospital and diagnosed with mild or moderate CTS by a specialist using electro-diagnosis were incorporated in the study. The severity of CTS was determined using history, physical examination, and nerve conduction studies.
Patients were included if they were women, between 35 to 60 years of age, diagnosed CTS by electro-diagnosis, and who had persistence of symptoms for at least 6 months. Mild CTS was defined as having a history of nocturnal numbness and paresthesia as well as a sensory peak latency more than 3.6 ms with a normal motor onset latency (≤ 4.2 ms). Moderate CTS was defined as diurnal and nocturnal paresthesia together with a sensory peak latency of more than 3.6 ms and prolonged motor onset latency (4.3 - 6 ms) with no evidence of atrophy and weakness in the thenar muscles.
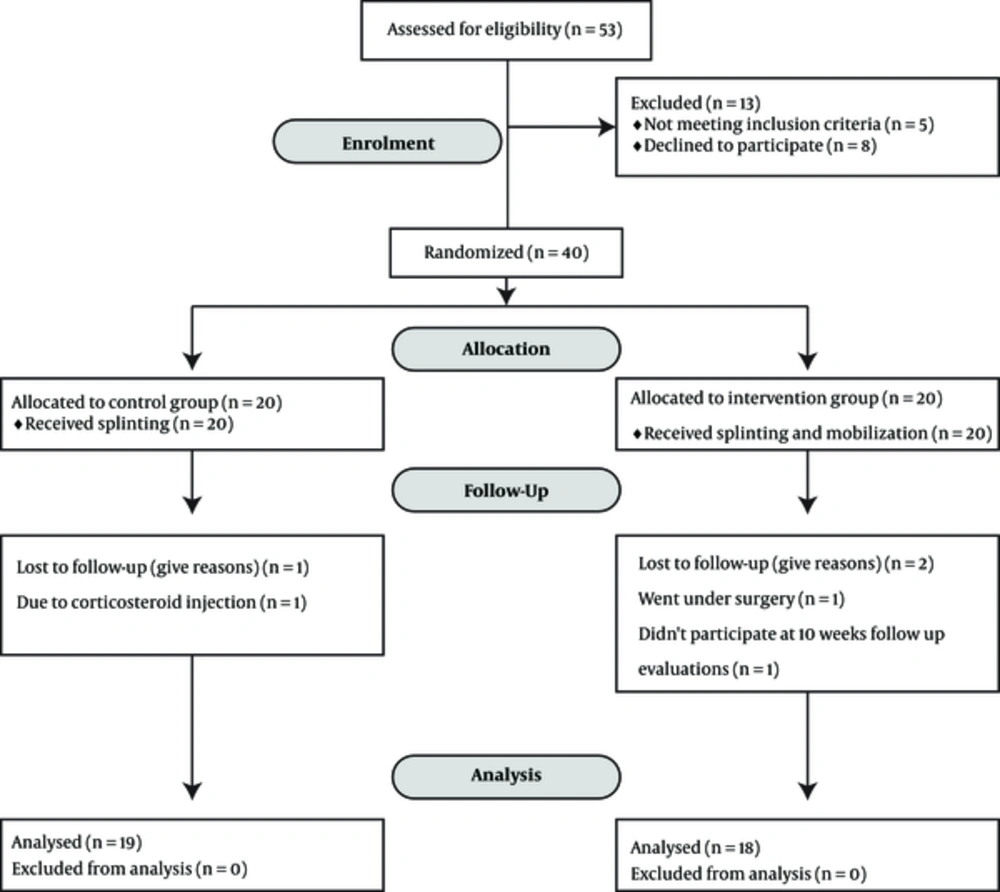
The following were reasons for exclusion: pregnancy, underlying metabolic diseases such as diabetes and thyroid diseases, rheumatoid arthritis, thenar muscles atrophy, evidence of concurrent neuropathy or radiculopathy, patients who requested to leave the study and history of other treatments including local corticosteroid injection or using of physical modalities or physiotherapy and splint in 3 months ago (Figure 1). The ethics committee of the University of Social Welfare and Rehabilitation Sciences approved this research study. It was also registered in the Iranian registry of clinical trials (IRCT:2015120125317N1).
Patients were provided with a written description of the study as well as a personal information questionnaire by a physiotherapist, with a consent form, which was signed by them if they were willing to participate in the study. The patients were afterwards randomly assigned to either an intervention or a control group. Numbers were generated randomly and patients assigned in a manner where none of the patients were aware of the subgroup they had been assigned to (19).
After assignment to intervention group, physiotherapist and physician who were assessing the outcomes were blinded. None of the patients received oral or topical medication during their treatment and follow up.
For all patients, splinting was performed at neutral position (0 - 5 degrees of wrist extension) for 8 weeks and it should be worn at night as well as in daily strenuous activities. In the intervention group, in addition to splinting, mobilization was also performed.
For all participants, variables of pain were measured based on the visual analog scale (VAS); symptom severity and functional status were evaluated based on the Boston questionnaire. In addition, sensory and motor distal latencies (using nerve conduction study) were evaluated before and 10 weeks after treatment. The Boston/Levine symptom severity scale (SSS) was used to evaluate the severity of symptoms including pain, paresthesia, and weakness. It contains 11 questions which the more severe symptoms gained the higher scores (20). Boston/Levine functional status scale (FSS) is used to evaluate the patient’s functional status. It contains 8 questions where the higher scores indicate more inappropriate functional status (20). Boston/Levine scales have been validated and are reliable for Iranian patients (18, 19, 21, 22). Electro-diagnostic study is a valid and reliable means of confirming the diagnosis of CTS (23). In electro-diagnostic studies, median sensory peak latency (SNAP) and motor onset latency were evaluated (22, 24).
A physiotherapist performed the scaphoid and hamate bone mobilization treatment 3 times a week for 8 weeks. Every session took 10 minutes. The mobilization techniques were anterior/posterior or posterior/anterior glide. In addition, the intensity of treatment, amplitude of mobilization, and treatment progress was depended on severity of symptoms and the patients’ irritability. The positioning and techniques used for manual therapy were as follows:
Positioning for scaphoid:
1. The patient was placed in a sitting position with the ventral aspect of the forearm on the table and the hand off the table.
2. If conservative techniques were indicated, the radiocarpal and ulnocarpal joints were in the resting position. If more aggressive techniques were indicated, they were approximating the restricted range.
3. The clinician was facing the radiocarpal and ulnocarpal joints.
4. The stabilizing hand griped the distal radius with the thumb on the dorsal surface and the index finger on the ventral surface.
5. Additional stabilization could be achieved by holding the patient’s hand against the clinician’s trunk.
6. The manipulating hand griped the proximal and distal carpal bone with the thumb on the dorsal surface and the index finger on the volar surface.
Procedures:
1. The stabilizing hand held the radius in position.
2. The manipulating hand glided the scaphoid in a volar and dorsal direction on the radius.
Positioning for hamate:
1. The patient was sitting with the ventral aspect of the forearm on the table and the hand off the table.
2. The midcarpal joints were in the resting position if conservative techniques were indicated or approximating the restricted range if more aggressive techniques were indicated.
3. The clinician was facing the midcarpal joint.
4. The stabilizing hand griped the proximal carpal bone with the thumb on the dorsal surface and the index finger on the ventral surface.
5. Additional stabilization could be achieved by holding the patient’s hand against the clinician’s trunk.
6. The manipulating hand griped the distal carpal bone with the thumb on the dorsal surface and the index finger on the volar surface.
Procedure:
1. The stabilizing hand held the proximal carpal bone in position.
2. The manipulating hand glided the hamate in a volar and dorsal direction on the triquetrum.
2.1. Statistical Analysis
In order to assess the changes in amount of pain, severity of symptoms, function of patients, the median nerve’s sensory, and motor latency before and after the intervention in both groups, the paired t-test was used. Comparing of carpal tunnel syndrome severity (according to electro-diagnosis) is assessed by Chi-square method. A P value of < 0.05 was considered statistically significant.
3. Results
In this present study, 37 female patients were studied in 2 groups. The mean of symptom duration was 14.3 ± 7.1 months. The mobilization group consisted of 18 CTS patients with mild to moderate disease severity, while the control group contained 19 similar patients (Figure 1). The mean age of the control and intervention groups were 46.36 and 49.22 years, respectively. The two treatment groups are homogeneous for all the parameters evaluated (Table 1).
Functional status (Boston questionnaire) as well as symptom severity (Boston questionnaire) and pain (VAS), were improved in both groups after 10 weeks follow up (P value < 0.05) (Table 2). Both groups showed improvement after intervention in the median sensory peak latency and the median motor onset latency (Table 3).
| Groups | Variables | Before ( mean ± SD) | After ( mean ± SD) | P Value |
|---|---|---|---|---|
| Mobilization | Pain severity | 5.44 ± 2.35 | 1.94 ± 1.34 | < 0.001 |
| Mobilization | Functional status | 2.33 ± 0.81 | 1.40 ± 0.35 | < 0.001 |
| Mobilization | Symptom severity | 2.58 ± 0.57 | 1.46 ± 0.37 | < 0.001 |
| Control | Pain severity | 6.36 ± 1.16 | 3.52 ± 2.06 | < 0.001 |
| Control | Functional status | 2.61 ± 0.57 | 1.76 ± 0.45 | < 0.001 |
| Control | Symptom severity | 2.52 ± 0.4 | 1.81 ± 0.44 | < 0.001 |
Comparison of Mean and Standard Deviation of Pain and Symptom Severity and Functional Status, Sensory, and Motor Distal Latencies in Each Group Before and After Treatmenta
| Groups | Variables | Before | After | P Value |
|---|---|---|---|---|
| Mobilization | Motor onset latency | 4.02 ± 0.57 | 3.88 ± 0.53 | 0.01 |
| Mobilization | Sensory peak latency | 3.97 ± 0.52 | 3.76 ± 0.5 | < 0.001 |
| Control | Motor onset latency | 4 ± 0.53 | 3.91 ± 0.51 | 0.003 |
| Control | Sensory peak latency | 3.87 ± 0.25 | 3.72 ± 0.25 | 0.001 |
Comparison of Mean and Standard Deviation of Median Nerve Motor and Sensory Distal Latency Before And After Treatment in Both Intervention and Control Groups
There was no significant difference between the 2 groups in the electrophysiological variables (median sensory peak latency and median motor onset latency). On the other hand, although treatment did have an effect on median nerve sensory peak latency and motor onset latency, the amount of change was not significant. However, a significant difference between the control and mobilization groups was found in functional status (Boston questionnaire) as well as symptom severity (Boston questionnaire) and pain (VAS) after intervention at 10 weeks follow up (P = 0.01) (Table 4).
| Variable | Intervention Group | Control Group | P Value Between Groups |
|---|---|---|---|
| Motor onset latency | 3.88±0.53 | 3.91±0.51 | P=0.85 |
| Sensory peak latency | 3.76± 0.50 | 3.72±0.25 | P=0.76 |
| Pain scale | 1.94±1.34 | 3.52±2.06 | P=0.01 |
| Functional status | 0.35±1.40 | 0.45±1.76 | P=0.01 |
| Symptom severity measure | 0.37±1.46 | 0.44±1.81 | P=0.01 |
Comparison of Mean and Standard Deviation of Pain and Symptom Severity, Functional Status, Sensory and Motor Distal Latencies Between Groups After Treatment
Patients were evaluated for disease severity based on electrodiagnostic studies at baseline and 10 weeks after treatment. The NCS findings returned to normal range in 36.8% and 38.9% of the patients in the control and the mobilization groups, respectively (Table 5).
| Group | CTS Severity Before Treatment (%) | CTS Severity After Treatment (%) | P Value (Chi-Square Test) | |||
|---|---|---|---|---|---|---|
| Mild | Moderate | Normal | Mild | Moderate | ||
| Control | 78.9 | 21.1 | 36.8 | 47.4 | 15.8 | 0.001 |
| mobilization | 77.8 | 22.2 | 38.9 | 44.4 | 16.7 | 0.002 |
Severity of Carpal Tunnel Syndrome According to Electro-Diagnosis Before and After Intervention (using Chi-Square method)a
4. Discussion
In our study, pain, symptom severity and functional status as well as median nerve conduction study improved in both mobilization and control groups after 8 weeks treatment. Although there was no statistically significant difference between the groups regarding median nerve sensory and motor distal latency, the improvement was statistically higher for pain and symptom severity as well as functional status in mobilization group.
The conservative management of CTS with manual therapy is an often-overlooked treatment approach, despite anecdotal clinical evidence from physiotherapists and preliminary research evidence from the chiropractic and osteopathic literature (18, 25, 26). The limited researches on manual therapy techniques, to include soft tissue mobilization (STM), carpal bone mobilization, or median nerve mobilization, myofacial release and others, indicated a tendency toward clinical improvements of the signs and symptoms of CTS and positive results were reported (16, 18, 27-30).
In 2006, George et al. studied the effectiveness of the active release technique on 5 CTS patients. The results of the study showed a statistically meaningful improvement in symptoms and function based on the Boston questionnaire (29). Burke et al. performed a study in 2007, the goal of which was assessing the role of manual therapy in improvement of the signs and symptoms of CTS (27). After manual therapy in both of the mentioned studies, improvement was seen in nerve conduction, wrist strength, and range of movement, which lasted for 3 months. Furthermore, in other studies, manual therapy has demonstrated the ability to improve pain, signs, symptoms, and function of those with CTS (16, 18, 28-30). In our study, similar results were reported although in our study these findings didn’t show any significant difference in nerve conduction study between the two groups. Explanation for this difference may be related to the small sample size in these pilot studies and different techniques for manual therapy. In addition, the majority of the previous studies haven't had a control group while in the current study, a control group is present.
While reviewing the previous studies, only one study (Tal-Akabi et al.) was found to evaluate the mobilization of wrist bones similar to our study. In 2000, Tal-Akabi et al. showed that there was no statistically significant difference in pain and nerve conduction velocity between a group of CTS patients who had received nerve mobilization and those who had received wrist bone mobilization (18). The results may have been influenced by the small sample size. In addition, in the aforementioned study, the entire wrist bones were mobilized, which had led to reduced pressure on the median nerve and therefore, reduction of the edema in the nerve space. This is while in the present study, the mobilization was performed more locally on the hamate and scaphoid bones, which lead to direct reduction of pressure in the carpal tunnel and increased blood supply, which may be the reason why this method has seen a meaningful difference in pain and symptom reduction (31-33).
In the current study, there was no meaningful difference between nerve conduction studies of the 2 groups. This could be attributed to the low number of patients. However, the statistically significant difference in the results of pain, symptoms, and function between the 2 groups has clinical value, since pain, symptoms, and function are what make the patient seek treatment in the first place. Improvements in these parameters will lead to the patients’ satisfaction with treatment, which will in turn make them more willing to receive it. Therefore, hamate and scaphoid mobilization is envisaged to have a better future for manual therapy in mild to moderate CTS.
The most positive points of our study were the presence of control group, new manual therapy technique, and concurrent evaluation of symptoms severity, patient function, and electro diagnosis study. This study does have some limitations, one of which is inclusion of only female patients aged 35 - 60 years; therefore, the effect of treatment on male CTS patients has not been studied. The sample size was relatively small. Finally, further follow up in order to observe the long-term effects of treatment was not possible.
A total of 8 weeks of hamate and scaphoid mobilization alongside splinting had a significantly better effect in the reduction of pain and severity of symptoms as well as functional improvement compared to splinting alone. Improvement of median nerve conduction studies was also observed, although there was no statistically meaningful difference in sensory and motor latencies between the 2 groups. This study suggest that scaphoid and hamate mobilization is an effective treatment for mild to moderate carpal tunnel syndrome; although future studies would be needed to study the long-term effects of this intervention on patient with mild to moderate carpal tunnel syndrome.