1. Background
Using peripheral nerve block has been popularized due to reduced postoperative pain based on VAS rating, reduced the need for painkillers as well as nausea, shortness of PACU time, and increased patient satisfaction (1). Among brachial plexus blocks, axillary approach has gained more popularity because of the ease, safety, and reliability (2); and recently many efforts have been conducted to improve the results of block with various additives. For this purpose, medications such as opioids, naloxone, clonidine, dexmedetomidine, midazolam, epinephrine, dexamethasone, and ketamine along with topical anesthetics were more effective (3).
Due to the increasing use of regional anesthesia compared to general anesthesia, conducting further studies for improving it, and also substantial benefits of axillary block compared to general anesthesia in hand and forearm surgery, anesthesiologists all around the world have encouraged to try to overcome the shortcomings of this method (4, 5).
Ultrasound, for instance, is used to improve the success rate of the block or decrease the block time (6). In addition, different adjuvants (clonidine, dexamethasone, naloxone, types of drugs, etc.) are used to reduce the onset time of sensory block required for surgery and increase the durability of the block in long-time surgeries. Additive adjuvant should have properties such as immunity, availability, and low cost, so that it can be widely used (7-10).
Ketamine is a non-competitive NMDA receptor antagonist, which is used for premedication, analgesia, sedation, induction, and maintenance stage of general anesthesia (11). Ketamine has been also used as local, regional, and central analgesic (12).
Dexamethasone is a corticosteroid that is added as an adjuvant to local anesthetic to increase block duration (5).
The aim of this study was to compare the effect of ketamine and dexamethasone as adjuvants to lidocaine on duration and onset of axillary block because no study has compared the effect of these two drugs on nerve block.
2. Methods
This study was a double-blind randomized clinical trial. Subjects were selected using convenience sampling method (7, 9). Using Cohen table for comparing and considering associated response with assumptions, the duration of sensory and motor block in the control group was determined as 189.7 ± 22.4 and 206 + 25.05, respectively, with the standard deviation of 22. Therefore, the sample size was calculated to be 26. The sampling was approved by the Ethics Committee of Iran University of Medical Sciences and registered in the site of clinical trial center (IRCT2017030132837N1).
Inclusion criteria included signing the consent form to participate in the research and willingness to cooperate with axillary block. Patients with no addiction to opioids, benzodiazepines, clonidine, those without liver and kidney failure, diabetes, cardiovascular disease, pulmonary disease, and coagulation disorders, those who had no sensitivity to local anesthetics and no history of seizures affected by them, those who received no opioids during the last 48 hours, those without anatomical deformities or burns or local infection in the block location, those who were not pregnant, and finally patients who required general anesthesia due to lack of desire or lack of cooperation during the surgery were excluded from the study. ASA I patients with BMI between 22 to 27 (22 ≤ BMI ≤ 27) and age of 20 to 50 years who referred to Hazrat-e-Fatemeh Hospital for short-term surgery (60 - 90 minutes) of hand and forearm were selected.
For axillary blocking, lidocaine 1% (38cc) and normal saline (2cc) were injected to control group, lidocaine 1% (38cc) and dexamethasone 8mg (2cc) to the second group, and lidocaine 1% (38cc) and ketamine 50 mg (2cc) to the third group. Using blocked randomization method in the form of 9 blocks, patients were randomly divided into 3 groups: receiving lidocaine alone, lidocaine + ketamine 50 mg/kg, and lidocaine + dexamethasone 8 mg/kg.
Patients were randomly divided into three groups using a table of random numbers and putting together the nine blocks. Adjuvants were prepared for injection by anesthesiologists who were aware of the methods in strictly confidential procedure, and the onset and duration of sensory and motor block were recorded by the researcher and his assistant who were quite unaware of the concentration and type of drugs injected. The patients were also blinded to the process. After a routine monitoring (controlling blood pressure, heart rate, and percentage of oxygen saturation in the blood), oxygen mask was placed over the patients’ mouth, the IV Cannula 20 was inserted into the other hand, and fentanyl 2 µg and midazolam 0.02 mg/kg were injected as sedatives.
The patients were lying in the supine position while the angle between their arm and trunk was 90° and the elbow was fixed to 110° at the bedside. Following sterilization, blocks were guided by ultrasound machine with linear high frequency (8 - 13 MHZ) probe (covered with sterile dressing) and nerve stimulator. All blocks were performed by the same anesthesiologist. A 24 gauge with 5 cm long and Teflon coated needle (Echoplex Vygon, UK) was attached to nerve stimulator and then introduced in-plane relative to the probe. One needle was penetrated to plexus sheet with the frequency of 1 Hz and 0.1 ms of pulse width. The current was decreased slowly when motor responses were obtained. Needle position was considered acceptable when motor response remained visible at 0.5 mA. After negative aspiration, the local anesthetic was injected. After injection, the onset of sensory block with pinprick feeling was measured every three minutes until complete sensory block and then, compared to the other side of the body. The onset of motor block after injection was measured every three minutes to complete motor block of thumb abduction for radial nerve, thumb adduction for ulnar nerve, elbow flexion and closing the forearm to arm for musculocutaneous nerve, and matching fingers together for median nerve.
Duration of sensory block, that is the time between the onset of complete sensory bock and the onset of the organ sense, was measured every 3 minutes after surgery through a skin test by a needle. Moreover, duration of motor block, which is the time between the onset of complete motor paralysis and the onset of muscle mobility fed by the nerves, was checked every 3 minutes after the surgery.
The collected data were analyzed by SPSS 22. Quantitative data obtained from the 3 groups were analyzed using ANOVA or Kruskal–Wallis test, and those obtained from the two groups were analyzed using Tukey test or Mann–Whitney U test. In addition, due to repeated measures in each group, ANOVA or Friedman test were used. Qualitative data obtained from the three groups were analyzed using Chi-square or Fisher exact test. Significance level was considered P < 0.05.
3. Results
In this study, 79 patients were enrolled and referred to Hazrat-e-Fatemeh hospital for hand and forearm soft tissue surgery during 2015 - 2016. The patients were randomly divided into three groups (each group of 26 patients). The first group received lidocaine alone, the second group lidocaine and dexamethasone, and the third group lidocaine and ketamine. However, in the lidocaine + ketamine group, one person who was suspected to use opioids before the surgery was excluded from the study due to hallucinations. Furthermore, there was no patient with insufficient or failed block.
There was no significant difference between age, gender, smoking, site of surgery, and surgical history in the damaged area in the three groups (P > 0.05) (Table 1).
| Variable | Group | P Value | ||
|---|---|---|---|---|
| Lidocaine | Lidocaine + Dexamethason | Lidocaine + Ketamine | ||
| Age, ya | 29.46 ± 9.81 | 31.88 ± 11.98 | 31.3 ± 10.79 | 0.807 |
| Gender, No. (%) | 0.13 | |||
| Female | 4 (15.4) | 3 (11.5) | 0 (0) | |
| Male | 22 (84.6) | 23 (88.5) | 26 (100) | |
| Smoking, No. (%) | ||||
| Yes | 14 (53.8) | 16 (61.5) | 13 (50) | 0.696 |
| No | 12 (46.2) | 10 (38.5) | 13 (50) | |
| Site of surgery, No. (%) | ||||
| Hand | 12 (46.2) | 10 (38.5) | 10 (38.5) | 0.809 |
| Forearm | 14 (53.8) | 16 (61.5) | 16 (61.5) | |
| History of surgery on the damaged area, No. (%) | ||||
| Yes | 22 (84.6) | 24 (92.3) | 21 (80.8) | 0.477 |
| No | 4 (15.4) | 2 (7.7) | 5 (19.2) | |
Comparison of Descriptive Characteristics in the Three Groups
Based on the results in Table 2, there was no significant difference in the onset of sensory and motor blockade of axillary block between the three groups (P > 0.05). Nevertheless, the difference in duration of sensory and motor blockade of axillary block between the three groups was significant (P < 0.05). Intergroup comparison showed that there was also no significant difference in the onset of sensory and motor blockade of axillary block between the groups (P > 0.05); however, the difference in duration of sensory and motor blockade of axillary block between the groups was significant (P < 0.05).
| Variable | Group | P Value | ||
|---|---|---|---|---|
| Lidocaine | Lidocaine+Dexamethason | Lidocaine+Ketamine | ||
| Onset of sensory Block, min | 5 ± 1.09 | 5.65 ± 2.48 | 5.32 ± 1.06 | 0.515 |
| Onset of motor block, min | 12.69 ± 1.66 | 12.26 ± 1.34 | 12.3 ± 1.64 | 0.558 |
| Duration of sensory block, min | 106.15 ± 7.91 | 174.42 ± 13.06 | 114.8 ± 12.53 | < 0.001 |
| Duration of motor block, min | 123.26 ± 8.82 | 194.26 ± 13.68 | 138.36 ± 17.08 | < 0.001 |
Comparison of the Onset and Duration of Sensory and Motor Blockade of Axillary Block in the Three Groupsa
There was a significant difference in nystagmus between the three groups (P < 0.05) (Table 3).
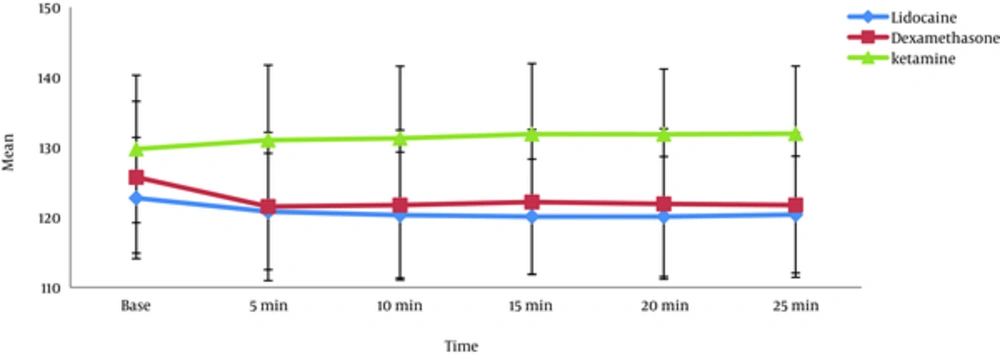
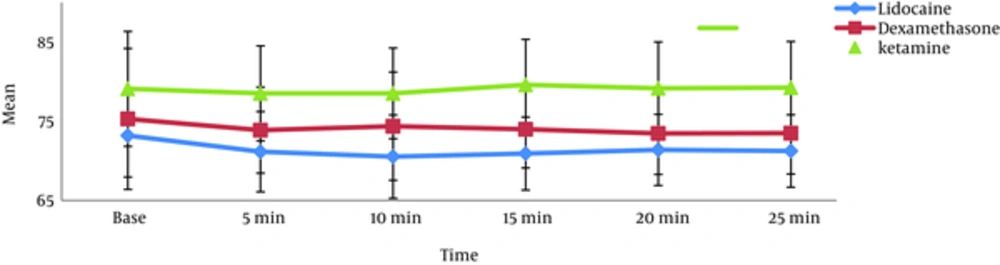
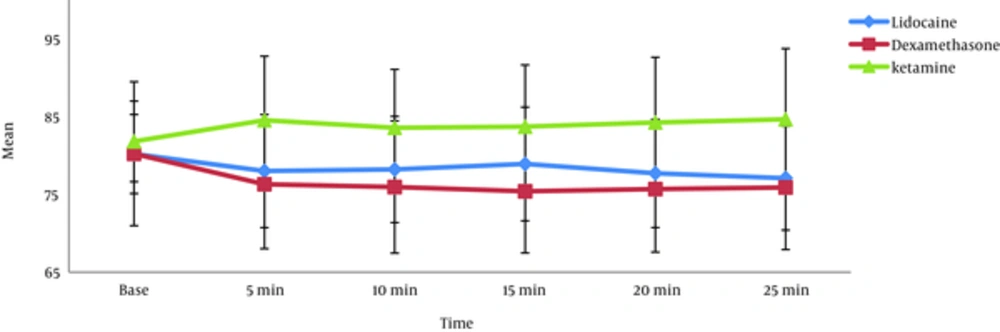
Hemodynamic changes (systolic blood pressure, diastolic blood pressure, and heart rate) at onset of the block and at 5 - 25 minutes after block axillary in Lidocaine + Ketamine group were higher than those in the other groups were (P < 0.05). This difference was observed at onset of the block and maintained until the end. There was no significant difference in hemodynamic changes between lidocaine and lidocaine + dexamethason group (P > 0.05).
Moreover, intergroup comparisons showed that systolic blood pressure, diastolic blood pressure, and heart rate in lidocaine and lidocaine + dexamethason groups decreased (P < 0.05). However, this decrease was not observed in the lidocaine + ketamine group (P > 0.05) (Figures 1-3).
4. Discussion
The present study was conducted to compare the effect of ketamine and dexamethasone as additives to lidocaine on duration and onset of axillary block action. Our results showed that duration of sensory and motor blockade of axillary block in lidocaine + dexamethasone group was significantly higher than that in lidocaine + ketamine group, and it was significantly longer in lidocaine + ketamine group than in lidocaine group. However, there was no significant difference in the onset of sensory and motor blockade of axillary block between the three groups.
According to the studies of Yaghoobi et al. (2013) (9) and Movafegh et al. (2006) (10), the duration of sensory and motor blockade of axillary block was significantly longer in lidocaine + dexamethasone group than in other groups. Similar to our study, there was no significant difference in the onset of sensory and motor blockade of axillary block between the three groups (9, 10).
In the study of Lashgarinia et al. (2014), there was no significant difference in the onset of sensory and motor block between the two groups of lidocaine + 2 mg ketamine and lidocaine. In addition, there was no significant difference in the duration of sensory and motor block of brachial plexus between the two groups, which was not consistent with the results of the present study. This inconsistency can be due to differences in the design of the studies such as ketamine dosage (7).
In another study carried out by Biradar et al. (2013), duration of sensory and motor block of the brachial plexus was higher in lidocaine 1.5% + 8 mg dexamethasone than in lidocaine 1.5% alone. However, unlike our study, adding dexamethasone shortened the onset of sensory and motor block of brachial plexus in the patients. This dissimilarity can be due to differences in lidocaine dosage in the two studies (13).
In the study of Bharti et al. (2015), duration of sensory and motor block of supraclavicular brachial plexus in the lidocaine and ropivacaine + 1 mg dexamethasone groups was longer than that in lidocaine + ropivacaine group. However, adding dexamethasone shortened the onset of sensory and motor block of supraclavicular brachial plexus, which is not consistent with the results of the present study. This can be explained due to differences in dexamethasone doses in the two studies (14).
Reddy et al. in 2015 conducted a study and proved that duration of sensory and motor block of supraclavicular brachial plexus was longer in the lidocaine 1.5% + 8 mg dexamethasone group than in lidocaine 1.5% group, but unlike our study, adding dexamethasone shortened the onset of sensory and motor block of the supraclavicular articular network of the patients (15).
In the studies of Arish et al. (2016) (16), Sabra et al. (2014) (17) and Vieira et al. (2010) (18), duration of sensory and motor block of brachial plexus was significantly longer in bupivacaine+ dexamethasone group than in bupivacaine group (16, 18) and in bupivacaine+ ketamine group (17). In addition, there was no significant difference in the onset of sensory and motor block between the two groups (16-18).
In the studies of Pathak et al. (2012) and Shaikh et al. (2013), duration of sensory and motor block of supraclavicular brachial was significantly longer in bupivacaine + dexamethasone group than in bupivacaine group. In addition, there was no significant difference in the onset of sensory and motor block between the two groups (19, 20).
In the study of Islam et al. (2011), unlike our study, adding dexamethasone to lidocaine and bupivacaine shortened the onset of sensory and motor block of supraclavicular brachial plexus in the patients. This dissimilarity could be due to differences in blocking methods used in the two studies (21).
Similar to our study, adding 50 mg ketamine to ropivacaine, in the study of Lee et al., (2002), had no effect on the onset of sensory and motor block axillary in patients. However, unlike our study, adding 50 mg ketamine to ropivacaine did not improve the duration of axillary sensory and motor block in patients (22).
In a review study conducted by Noss et al. (2014), dexamethasone, as a supplement in the nerve block, prolonged sensory and motor block of brachial plexus in patients and its effect on the sensory and motor block varied, but its clinical benefit was not clear (23). Choi et al. in their meta-analysis study (2014) reported that receiving dexamethasone along with nerve block could prolong the duration of sensory and motor block of brachial plexus without side effects (24).
According to the results of the present study, hemodynamic changes (systolic blood pressure, diastolic blood pressure, and heart rate) at the onset of block and 5 - 25 minutes after axillary block in lidocaine + ketamine group were higher than those in the other groups were. This difference was observed at the onset of the block and maintained until the end. However, there was no difference in this regard between lidocaine + dexamethasone group and lidocaine alone group. In addition, comparisons between the groups showed that systolic blood pressure, diastolic blood pressure, and heart rate decreased in lidocaine + dexamethasone and lidocaine groups, which could be due to sedation and analgesia in patients (25). However, hemodynamic changes did not decrease in lidocaine + ketamine group and even some increases were observed in this group, which can be due to ketamine systemic absorption and sympathomimetic effects of ketamine.
In the study of Arish et al. (2016), there was no significant difference in the hemodynamic changes (systolic blood pressure, diastolic blood pressure, and heart rate) between bupivacaine+ dexamethasone and bupivacaine groups every 10 minutes within 210 minutes after implantation of brachial plexus block (16).
Lashgarinia et al. (2014) showed that there was no significant difference in the hemodynamic changes (MAP and heart rate) between lidocaine + 2 mg/kg ketamine and lidocaine groups every 15 minutes within 90 minutes after the insertion of brachial plexus block, which is not consistent with the results of this study. This inconsistency can be due to differences in the study design in the two studies (7).
In the study of Yaghoobi et al. (2013), there was no significant difference in hemodynamic changes (systolic blood pressure, diastolic blood pressure, and heart rate) between three groups of lidocaine, lidocaine + dexamethasone, and lidocaine + fentanyl every 5 minutes within 20 minutes after the insertion of axillary block (9).
In the present study, nystagmus complication was also observed in 27% of lidocaine+ ketamine group; however, in lidocaine + dexamethasone and lidocaine groups, this complication was not observed.
Finally, follow-up of patients who underwent hand and forearm surgery was done accurately. Adding dexamethasone or ketamine to lidocaine could improve the duration of axillary sensory and motor block. In addition, adding ketamine to lidocaine increased hemodynamic parameters including systolic blood pressure, diastolic blood pressure, and heart rate and nystagmus complications; while, adding dexamethasone to lidocaine did not increase hemodynamic parameters and nystagmus complications.
4.1. Conclusion
According to the results of this study, adding dexamethasone or ketamine could improve the duration of sensory and motor block axillary in patients who were candidates of hand and forearm soft tissue surgery. However, the effect of dexamethasone on prolonging the duration of sensory and motor block axillary was significantly greater than the effect of ketamine. In addition, adding ketamine to lidocaine was associated with complications such as nystagmus and hemodynamic changes. In addition, adding dexamethasone or ketamine to lidocaine had no effect on the onset of sensory and motor block axillary. Therefore, it is recommended to add dexamethasone to lidocaine to prolong the duration of sensory and motor block axillary in patients undergoing the surgery of hand and forearm soft tissue.
We suggest that other researchers use different doses of ketamine and use bupivacaine combinations with other adjuvants.