1. Introduction
Nowadays in modern medicine, many practical measurements are not applicable without using devices or catheters (1, 2). In 1954, catheter emboli were reported for the first time (3). Reported embolized foreign bodies consist of catheters, ports, instruments, devices (1, 4-7), or even cotton or cellulose fibers (8). Embolization may occur during application, insertion, or even years after implantation (7, 9). It can be partial or complete (10). Catheter emboli incidence has been reported in articles from 0.1% to 25% (11, 12). Efficacious determinants affecting catheter emboli incidence are characteristic of the catheter, technique of insertion, and also, the site of embolization. Patients’ general condition and management may influence the complications (11, 13, 14). By applying modern catheters, the incidence of this complication has decreased (11). Catheter embolization may remain undetected for a long time and often diagnosed incidentally (7, 12, 15). Catheter malfunction may be the first sign of this complication (7, 12). Many embolized foreign bodies were completely asymptomatic and founded only during autopsies (1, 8).
Venous catheters or its fragments may be embolized to the various sites (7). The rate of serious complications associated with foreign body embolism is about 71% (1). Mortality rate varies from 1.8% to 60% (1, 7, 13, 14); however, all of these deaths have not been confirmed to be directly a consequence of catheter embolism (11). Particularly, patients who have devices in their cardiopulmonary system are at risk of severe complications such as arrhythmia, pulmonary embolism, myocardial injury, hemoptysis, thrombosis, or perforation (1, 6, 7, 14). In more than 52% of catheters, which are in their normal position for more than 48 hours, bacterial contamination has been reported (1, 6, 14). Based on our knowledge, there was not any report about a lost and remained Permcath for a longtime period. Regarding these data, we decided to present this patient with a remained catheter in her body for about three years.
2. Case Presentation
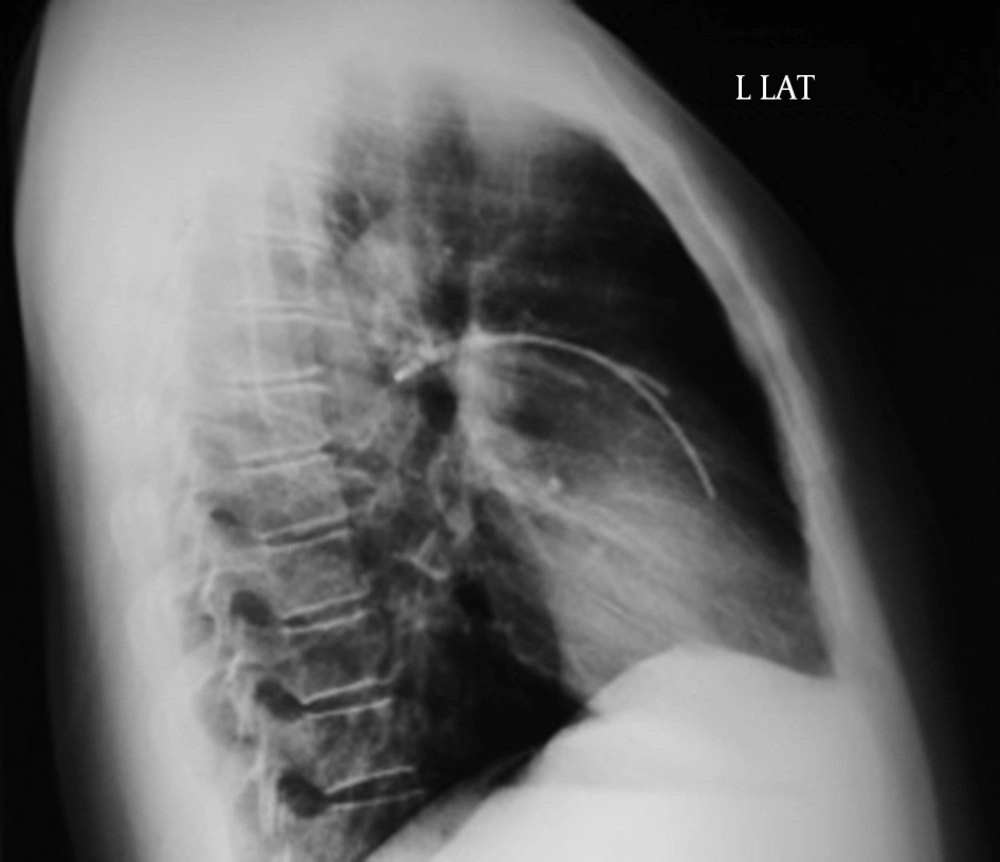
A 50-year-old woman, with a history of breast cancer and a course of radiotherapy and chemotherapy, had a Permcath emplacement in right subclavian vein in august 2008 for her chemotherapy. Permcath is a flexible double lumen cuffed plastic tube that can be put into a vein just below the neck. The tube can then be used for long term purposes. The patient was otherwise in a good health condition and did not have any other positive medical or drug history. The treatment for cancer seemed to be successful and her oncologist performed routine follow-up measurements. The Permcath had remained in its position without any complication for three years followed up by routine chest X-ray study (Figures 1 and 2). However, the Permcath was found broken totally from its base and embolized to right ventricle and the left main pulmonary artery (Figures 1 and 2) after three years of insertion.
The chest X-ray (dated a year before our evaluation) revealed that the Permcath was intact and in its normal position. Furthermore, there was no history of physical or traumatic injury or accident in the precise history review for the last three years. The patient did not report any use of her Permcath during the last investigation and did not remember any obvious complaint regarding embolization, migration, or lodging the catheter. There was not any positive chief compliant at the time of detection and physical examinations. Furthermore, electrocardiography and echocardiography investigations were normal or unchanged comparing with the previous ones.
We hypothesized that sticking the catheter between her clavicle and first rib was the probable cause of its breaking (pinch-off syndrome). In consultation with colleagues and experts, and following discussion of probable symptoms and potential complications, considering the lack of any sign or symptom and the risk of open surgery to removal of the embolized catheter, we decided to leave it in its position, and the patient was advised to perform regular consecutive follow-up studies. There was no change in the patient condition and the catheter position during a one-year follow up.
3. Discussion
The main concerns with dislocated embolization coils are local thrombogenicity and distal ischemia (1, 6). Vascular wall may be perforated by guide-wires, stents and filters. There are reports of sudden death cases at the time of embolization (11). The worst prognosis has been reported in the patients with right heart catheter embolism with a mortality rate of 53% in the non-operated group. Intravascular embolization of port catheters can be asymptomatic at the time of diagnosis (7) or induce serious cardiovascular, pulmonary and septic complications with an overall mortality rate of 1.8% (7, 13). By a large margin, retracting the catheter through the needle was the most common mechanism of catheter embolization for many years (1, 11). Entrapment of the catheter between clavicle and first rib (“pinch-off”) is another cause of embolization (7, 12, 15). To prevent pinch-off syndrome, port catheter should be implanted more laterally in the subclavian vein, or in some cases, jugular vein should be applied (12). Such preventive measurement may be impossible or too difficult in patients with history of chemotherapy and radiotherapy. Needle shearing force should be avoided by protecting the tubing, especially in flexion areas (16).
Guidelines suggest that unused ports should be removed (17). Regarding the potential dangers of retained intravascular objects, it is advised that intravascular deices should be precisely localized and taken away as soon as possible, if a piece of the device is lost in the cardiovascular system before it reaches heart (1, 4, 6, 12, 15). If a polyethylene catheter or a silicone rubber stays in cardiovascular system for about 6 - 8 weeks, their removal is complicated because of fibrous endothelial reaction around the catheter (14, 18).
Permcath is made of soft, silicone materials. These objects also may potentially act as a core for thrombosis; therefore, letting them to remain in a pathologic position is inadvisable (12, 18). Thoracotomy and its accompanied problems have made surgical device removal as a displeasing choice (14, 18). Besides, in the cases of longtime foreign bodies in vascular system, surgical techniques are too hard to be applied (7, 18). Based on long-term follow-up, there is no difference between patients in whom stents were removed percutaneously and those whose stents were removed to a secured replaced position (1). Furthermore, it is better to evaluate the risks associated with the retrieval maneuver, such as permanent vascular wall trauma, against the advantage to the patient from the percutaneous procedure, before doing any invasive therapeutic measurement (1, 6).
Considering all potential problems and disadvantages, we strongly recommend that with regarding the guidelines, all foreign bodies and devices -which were applied intravenously- should be removed safely to prevent possible complications and decrease morbidity and mortality, if they are not supposed to be utilized anymore.