1. Background
Almost 8% to 28% of critically ill patients admitted to intensive care units suffer from ventilator-associated pneumonia (VAP) which increases morbidity and mortality (1). Occurrence of VAP increases health system costs; thus, any intervention to reduce VAP will result in reducing costs, morbidity and mortality (2). Suction of respiratory secretions is a necessary procedure in patients with artificial airway (endotracheal intubation or tracheostomy) to remove respiratory secretions and to maintain permeability of the airway. Critically ill patients under mechanical ventilation require frequent suctioning of airway secretion, which might result in increased hypoxemia, infections, and ICU length of stay (2). Closed tracheal suction system (CTSS) permits the health care providers to perform suctioning several times without disconnection from ventilator; thus, it might decrease hypoxemia and infection rate. Primary studies have shown that close suction (CTSS) could result in lowered pneumonia rates because of lower incidence of intervention in respiratory circuit (3).
In 2003, respiratory care society of the USA strongly recommended CS as one of the preventive strategies for VAP (4). Different studies showed that CTSS usage reduced nursing work load, dysrhythmias, intracranial pressure and hypoxemia during procedure (5-8). Other studies recommended CTSS for VAP prophylaxis and mentioned that the most important superiority of CTSS is decreasing environmental pollution (9, 10). However, there are studies suggesting low evidence for prevention of VAP with CTSS, and recommending physicians to consider the cost of the procedure prior to its use (1, 5). A study showed that there is not any significant difference between close and open suction with regard to ICU length of stay and mortality (11). Other similar studies have shown that CS should be changed every 48 hours concluding that further trials are required to include CTSS in VAP prevention guidelines (12, 13).
2. Objectives
Based on the above-mentioned facts, we performed a study comparing the efficacy of open and CTSS in reducing VAP in critically ill patients.
3. Patients and Methods
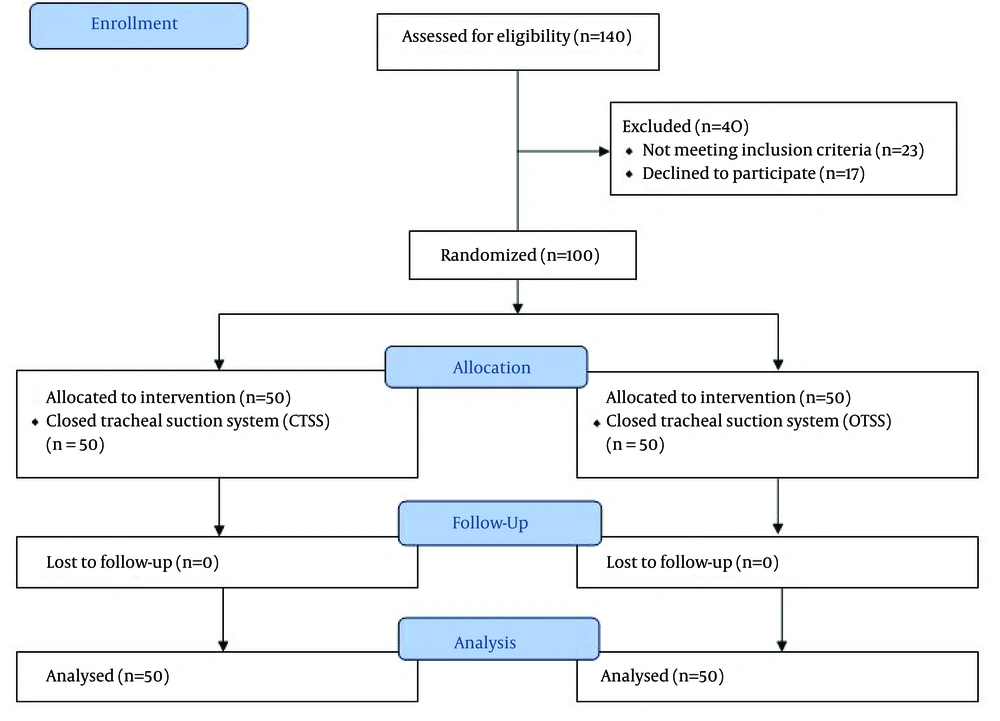
Our study was conducted after approval of Ethics Committee of Tabriz University of Medical Sciences, Tabriz, Iran. Informed written consents were obtained from patients or their legal guardians. This was a prospective randomized trial which was conducted from June 2012 until November 2013 in two ICUs with 24 beds. All patients aged more than 18 years old requiring mechanical ventilation for more than 48 consecutive hours were enrolled in this study (Figure 1). Patients unwilling to participate or those with pneumonia were excluded from the study. Hundred adult patients with the mentioned criteria were randomized into one of the study groups using internet based software.
In Open tracheal suction system (OTSS), suction was performed by single use catheters with full barrier measures (hand washing and use of gloves).Patients were preoxygenated for 2 min before suctioning. In the CTSS group, the system used for respiratory system suctioning was Ti-Cares (Covidien Company-USA) and suction catheter was changed every 48 h. Similar to other group, the patients were preoxygenated, and suction was performed without disconnection from the ventilator. VAP prophylaxis strategies were used in all patients as follows; head elevation (30-40°), heat and moisture exchanger (HME) for humidification, protocolized sedation and enteral nutrition, performing suction only when necessary, avoiding routine change of the respiratory circuit unless necessary, mouth washing with chlorhexidine in each shift, pantoprazole for prophylaxis of stress ulcer, verification of gastric residual volume in each shift, avoidance of unnecessary extubation or intubation, maintenance of cuff pressure between 20-30 mmHg and continuous aspiration of subglottic secretions.
In both groups, catheters were inserted in off position and withdrawn in a rotational status and the duration of each suctioning was less than 20 sec. Throat samples were taken on admission and two times per week in each patient. Tracheal samples were performed during endotracheal intubation, two times per week during mechanical ventilation and during extubation.
In addition, necessary clinical samples were taken. Diagnosis of VAP was performed based on clinical pulmonary infection score (CPIS) (14). Pneumonia was considered VAP only if it was not present at the time of mechanical ventilation initiation. Demographic characteristics, Acute Physiology and Chronic Health Evaluation II score (APACHE II); number of suctions per day, and duration of mechanical ventilation were noted for all patients. The percentage of VAP occurrence was calculated in each group and during predefined period.
3.1. Statistics
We estimated sample size of 100 people, with a power of 80%, and α error of 0.05 to detect 15% difference in VAP incidence between two groups. Qualitative variables were reported as percentage and quantitative variables as mean± standard deviation. We used Student t test and chi-square test for detection of differences between two groups. Fisher exact test was used for qualitative analysis when it is necessary. The Logistic regression analysis with "Enter" method was applied in order to evaluate the effects of selected independent variables on VAP incidence. In this analysis, odds ratios and their 95% confidence interval (CI) were reported. SPSS 16 program was used for statistical analysis. P value equal or less than 0.05 was considered statistically significant.
4. Results
A total of 100 patients (50 in CTSS group and 50 in OTSS group) were enrolled. Demographic characteristics of patients, including age, sex, and primary diagnosis were not significantly different between two groups (Table 1). No significant difference could be observed regarding the occurrence of sinusitis, type of humidification, and stress ulcer prophylaxis between two groups. APACHE II scores were not significantly different between two groups, and had a mean of 24 for the OTSS group and 25 for the CTSS group, implying homogeneity between the groups with regardto the illness severity.
Among the patients in OTSS and CTSS groups, 20% and 12% developed VAP, respectively (P > 0.05) (Table 1). Incidence of VAP among all patients enrolled in this study was 16%. Tracheostomy, sinusitis and type of humidification did not show significant difference between patients with or without VAP. Drainage of subglottic secretion decreased the incidence of VAP (P < 0.05). Also type of pharmacologic medicine for stress ulcer prophylaxis has a significant effect on VAP incidence (Table 2). The multivariate analysis implies that patients exposed to PPI and H2 antagonists had a higher chance of VAP development compared with sucralfate (Table 3). Due to the low number of outcome and collinearity of its follow-up, subglottic drainage as an independent variable was removed from the model. Use of CTSS comparing with OTSS did not show statistically significant effect on VAP incidence in multivariate analysis; however, OR tended to identify OTSS as an exposure factor for the development of VAP (OR = 1.92; CI = 0.45-8.30; P = 0.38) compared with the CTSS. In other words, patients undergoing open suction had a 92% higher chance of developing VAP. Higher level of APACHE II score, sinusitis and undergoing tracheostomy put the patients at the risk of VAP. However, using HME instead of humidifier would decrease this risk. We had one case of exogenous VAP in each group, with the isolation of the similar microorganism that had not been previously isolated from their throats; this might have been due to bronchoscopy procedure in these patients.
| OTSS (n = 50) | CTSS (n = 50) | P Value | |
|---|---|---|---|
| Age, y | 62.3 ± 13.7 | 63 ± 12.6 | 0.77 |
| Male | 34 (34) | 30 (30) | 0.41 |
| Diagnosis | 0.981 | ||
| Pulmonary fat or embolic syndrome | 6 (12) | 5 (10) | |
| Myocardial infarction | 2 (4) | 2 (4) | |
| Multiple trauma | 18 (36) | 15 (30) | |
| Post CPR | 2 (4) | 3 (6) | |
| Sepsis | 16 (32) | 16 (32) | |
| Respiratory failurec | 1 (2) | 2 (4) | |
| ARDS | 1 (2) | 2 (4) | |
| Cerebrovascular accident | 4 (8) | 5 (10) | |
| APACHE II | 24.9 ± 5.3 | 25 ± 5.5 | 0.93 |
| Sinusitis | 10 (20) | 8 (16) | 0.60 |
| Humidification | 0.21 | ||
| HME | 32 (64) | 30 (60) | |
| Humidifier | 18 (36) | 20 (40) | |
| Tracheostomy | 8 (16) | 8 (16) | 1 |
| Subglottic drainage | 45 (90) | 44 (88) | 0.75 |
| Stress ulcer prophylaxis | 0.24 | ||
| H2 antagonist | 21 (42) | 29 (58) | |
| PPI | 11 (22) | 10 (20) | |
| Sucralfate | 18 (36) | 11 (22) | |
| Incidence of VAP | 10 (20) | 6 (12) | 0.27 |
| Variable | VAP | P Value | |
|---|---|---|---|
| Yes (n = 16) | No (n = 84) | ||
| Age, y | 62.3 ± 13.7 | 63 ± 12.6 | 0.77 |
| Male | 11 (68.8) | 48 (57.1) | 0.39 |
| Diagnosis | 0.90 | ||
| Pulmonary fat or embolic syndrome | 2 (12.5) | 9 (10.7) | |
| Myocardial infarction | 0 | 4 (4.7) | |
| Multiple trauma | 6 (37.5) | 27 (32.1) | |
| Post CPR | 0 | 5 (6) | |
| Sepsis | 6 (37.5) | 26 (31) | |
| Respiratory failure c | 0 | 3 (3.6) | |
| ARDS | 0 | 3 (3.6) | |
| Cerebrovascular accident | 2 (12.5) | 7 (8.3) | |
| APACHE II | 24.9 ± 5.3 | 25 ± 5.5 | 0.93 |
| Sinusitis | 5 (31.2) | 13 (15.5) | 0.13 |
| Humidification | 0.13 | ||
| HME | 7 (43.8) | 55 (65.5) | |
| Humidifier | 9 (56.2) | 29 (34.5) | |
| Tracheostomy | 4 (25) | 12 (14.3) | 0.28 |
| Subglottic drainage | 8 (50) | 81 (96.4) | 0.001 |
| Stress ulcer prophylaxis | 0.001 | ||
| H2 antagonist | 5 (31.2) | 45 (53.6) | |
| PPI | 10 (62.5) | 11 (13.1) | |
| Sucralfate | 1 (6.2) | 28 (33.3) | |
| CTSS | 6 (37.5) | 44 (52.4) | 0.28 |
| OTSS | |||
| Variables | Odds Ratios | CI (95%) | P Value |
|---|---|---|---|
| OTSS c | 1.92 | 0.45-8.30 | 0.38 |
| Age, y | 0.96 | 0.91-1.02 | 0.19 |
| APACHE II | 1.13 | 0.95-1.34 | 0.15 |
| HME humidification | 0.3 | 0.07-1.37 | 0.12 |
| Sinusitis | 4.48 | 0.56-23.35 | 0.07 |
| Tracheostomy | 5.2 | 0.68-41.16 | 0.12 |
| H2 Antagonist | 4.45 | 0.28-70.0 | 0.29 |
| PPI | 33.02 | 1.32-823.78 | 0.03 |
| Sucralfate | Referent | 0.04 |
5. Discussion
VAP is a main source of concern in critically ill patients because of its high mortality and frequency (15-18). Our study results showed that incidence of VAP did not have any significant difference between OTSS and CTSS. Incidence of VAP in OTSS was 20% and in CTSS was 12%. Wide range of VAP incidence in different studies could be due to the heterogeneity of critically ill patients. For example, in a study performed on liver transplanted patients, no difference in VAP incidence was seen between open and close systems.
Some studies have shown that using CTSS could result in a higher rate of colonization without the incidence of VAP (19, 20); whereas, others have suggested that CTSS does not increase colonization of lower respiratory tract, yet it reduces the spread of infection in ICUs (21). Two studies reported the decreased incidence of VAP significantly (P = 0.037, P = 0.05 respectively) using CTSS (22, 23). In contrast, Zeitoun et al. showed that CTSS could result in decreased VAP incidence without a significant difference between OTSS and CTSS (24). As previously mentioned, these two systems have some advantageous and disadvantageous, so if we use each system correctly with aseptic precautions and based on indications, it seems that we would reach our targets.
Similar to our study, a few studies have shown that using CTSS could result in lower incidence of cardiac dysrhythmias (25), hypoxemia, alveolar derecruitment and loss of lung volume compared to CTSS6. Hence, it seems that in mechanically ventilated patients, CTSS could be considered for suction because PEEP and Fio2 are maintained constant, which reduces respiratory complications. Kollef et al. (26) did not find any significant differences in the incidence of VAP between patients with or without daily routine change of the suction system. Also Lorente et al. (27) showed that use of the closed system without routine complete daily change, while maintaining the suction catheter clean, did not increase the development of VAP compared with the open system.
We changed CTSS every 48 hours based on the mentioned results. This could explain our negative results as daily changing of CTSS should have resulted in less biofilm production which is an important mechanism in pathogenesis of VAP. Studies by Topeli et al. (19) and Deppe et al. (20) showed that CTSS could increase colonization of the respiratory system without a significant increase in VAP incidence due to higher rate of procedures that physicians could perform with CTSS. Nevertheless, Grossi and Santos observed that CTSS could avoid contamination if the catheter is washed with saline after each intervention (28). As we used this method after each procedure in CTSS group, our results showed no increase in the incidence of VAP in CTSS. Our results did not show any significant difference between two groups regarding length of ICU stay, which is similar to the results of Combes et al. (23), Topeli et al. (19). Ozcan et al. (29) showed that presence of CTSS could result in an intolerable increase in work of breathing and consequently, respiratory muscle fatigue, which is in contrast to our results.
Akerman E et al. in their study showed that no beneficial effects were seen on VAP incidence or interpatient contamination in CTSS compared to OTSS. A high frequency of circuit contamination in the CSS group paralleled with experienced secretions clearance problems seem unfavorable and in concordance with previous studies (30). Juneja et al. showed that CTSS with or without intermittent subglottic suction drainage has no significant effect on VAP incidence. Hence, intermittent subglottic drainage may be recommended for VAP prevention, but indications other than VAP prevention should determine the type of the suction system (31). Our study showed that in patients having received pantoprazole for stress ulcer prophylaxis, the incidence of VAP was significantly higher compared to sucralfate use, which seems to be due to higher pH in pantoprazole group and also increasing colonization of possible aspirated contents. Zeitoun et al. (24) showed that the cost of a closed suction system is less than an open system, which is in agreement with findings of Kollef et al. (26). Peter et al. in an analysis showed that CTSS has no superiority over CTSS with respect to VAP or mortality and decision for the use of CTSS may be based on possible benefits in patients requiring high respiratory supports, reduced cost in prolonged mechanical ventilation or safety concerns with OTSS (32). Hanada in his review showed that there are no definite advantages of CTSS over OTSS; nevertheless, there are significant differences between the clinicians' and manufacturers' indications. In fact, CTSS could reduce the loss of lung volume in mechanically ventilated patients (33).
In our study, mortality rate was not of significant difference between groups, which is similar to the previous studies (27, 34). Based on the results obtained from our study, impact of suctioning is similar between CTSS and OTSS regarding the occurrence of VAP. It seems that physicians must consider many factors such as duration of mechanical ventilation, comorbidities, oxygenation parameters, number of required suctioning, and the cost prior to using each type of tracheal suction system. However, further well-designed trials with larger sample sizes and improved demographic data are required in order to evaluate the exact effect of tracheal system types on VAP and update the guidelines.
Our study had some limitations. Firstly, this study was an RCT which was performed in 2 ICUs with an almost small sample size. Secondly, we did not perform cost analysis for each group. Low number of dependent variables has affected the strength of the study, but the method of analysis and its interpretation are appropriate.