1. Background
Proper airway management is the most important task for an anesthesiologist during general anesthesia. Endotracheal intubation is the gold standard for airway management; however, this maneuver requires expertise and lots of clinical experience (1, 2). Laryngoscopy and endotracheal intubation trigger the sympathetic reflex response, increase the plasma level of catecholamines, and cause hypertension, tachycardia, myocardial infarction, decreased myocardial contractility, and ventricular arrhythmia, all of which can be life-threatening (3, 4). Attempts to prevent complications related to endotracheal intubation and laryngoscopy led to the introduction of new airway devices, namely, laryngeal mask airway (LMA) and I-Gel. LMA has been successfully used for more than a decade. It has an airway tube that connects to a mask with a cuff that is inflated. It has been used in managing difficult airways and in different kinds of surgeries with minimal changes in hemodynamic responses (5-7). Incorrect positioning of the LMA leads to aspiration, pneumonia, air leakage, and partial airway obstruction with an overinflated or malpositioned cuff, and might even trigger the sympathetic reflex responses (8-12). I-Gel is a supraglottic airway device, renowned for its easy application and simplicity, particularly for the resuscitation procedures (13). I-Gel works in accordance with human anatomy with lesser trauma to the pharynx, larynx, and supraglottic areas due to its minimal displacement. This device is capable of separating the gastrointestinal and the respiratory systems and possesses a tube to suction the stomach contents. Its rapid placement, possession of a noninflatable cuff, and disposability are among the other advantages of this device, which have led to the extensive use of I-Gel as a supraglottic airway device for anesthesia and cardiopulmonary resuscitation since 2007. Its recognized complications include laryngeal spasm, laryngeal trauma, sore throat, regurgitation of stomach contents, vomiting, neural injury, vocal cord paralysis, trauma to the tongue or sublingual nerves, and dysesthesia or cyanosis of the tongue (14-17).
2. Objectives
This study was designed to compare the success rate of airway management using LMA and I-Gel in patients undergoing elective orthopedic surgeries. The insertion time, failure rate, and incidence of complications including sore throat, bleeding, and hoarseness were compared between study groups.
3. Patients and Methods
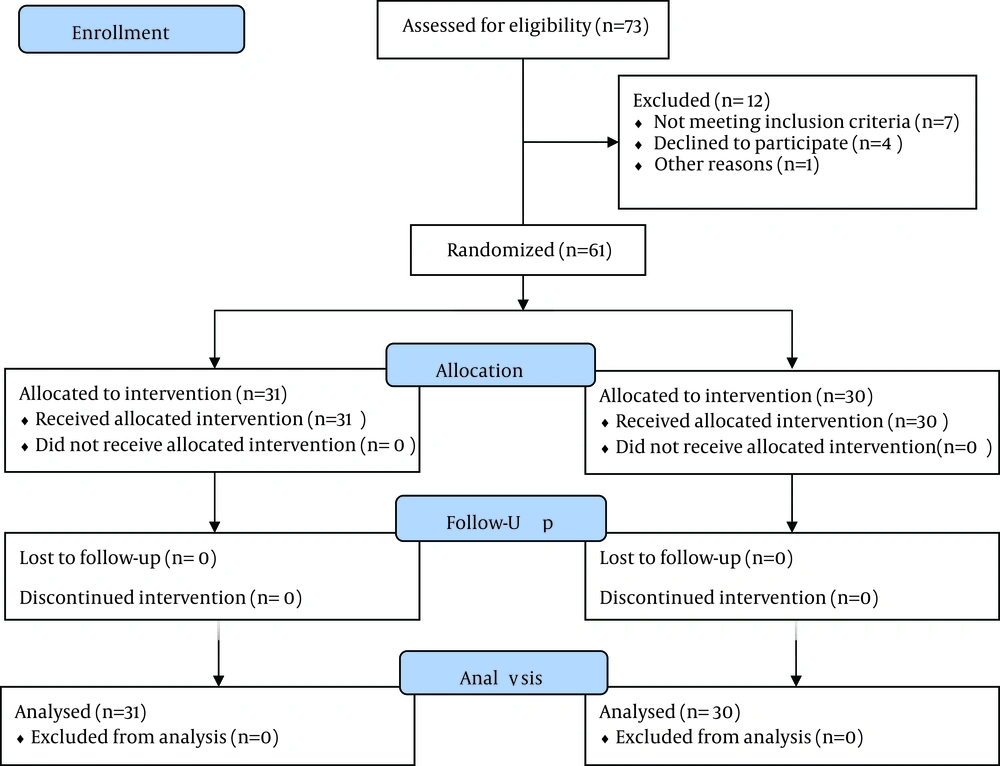
The study was approved by Research Ethics Committee of Iran University of Medical Sciences, registered at Iranian registry of clinical trials site (ID: IRCT201307284969N7) and written informed consent was obtained from all subjects. This single-blinded randomized clinical trial was performed on patients requiring minor orthopedic surgeries (with shorter than one hour duration) such as knee arthroscopy and malleolus fracture in Firoozgar Hospital, Iran University of medical Sciences, Tehran, Iran. Sample size was calculated at 26 in each group based on statistical significance level of α = 0.05 and B = 0.90 to detect 40% differences in success rate of insertion (18). After excluding 12 patients (due to different reasons) (Figure 1), the remained 61 patients were randomly allocated to two groups of LMA (n = 31) and I-Gel (n = 30) using block randomization. The inclusion criteria were age range of 18 to 70 years, complete NPO time (empty stomach), ASA Class 1 and 2, requiring minor orthopedic surgeries (estimated duration < 1 hour), airway characteristics of thyromental distance (TMD) > 60 mm, Mallampati score of one and two, mouth opening > two finger, absence of reflux gastroesophageal reflux disease, body mass index < 30 kg/m2, no contraindication for the anesthetic or the muscle relaxant agents, and no history of difficult airway in previous operations. After transferring the patients to the operating table, an intravenous catheter was placed in their hand and the subjects received standard monitoring of ECG, heart rate, oxygen saturation, and blood pressure. Anesthesia was induced as follows:
First, 5 mL/kg crystalloid IV fluids were administered and then the patients were preoxygenated for three minutes. The patients received 0.02 mg/kg midazolam and 2 μg/kg fentanyl for premedication. Anesthesia was induced by the administration of 5 mg/kg thiopental and 0.5 mg/kg atracurium. After three minutes of ventilation, the respective mask LMA (Haiyan kangyuan Co., China) (Figure 2) or I-Gel (Intersurgical Co., United Kingdom) (Figure 3) was placed by an anesthesiology resident (third year) who was expert in using these devices and used to insert both of them for general anesthesia for more than one year. The following LMA devices were placed for patients in LMA group:
LMA #3 for patients weighing 30 to 50 kg; LMA #4 for patients weighing 50 to 70 kg; and LMA #5 for patients weighing 70 to 100 kg.
The following I-Gel airways were inserted for patients in I-Gel group:
I-Gel #3 for patients weighing 30 to 60 kg; I-Gel #4 for patients weighing 60 to 90 kg; and I-Gel #5 for patients weighing > 90 kg.
The patients were then ventilated using a bag-valve device. Airway insertion would be considered successful if there was no air leak during ventilation and the patient had an airway pressure of ≤ 20 cm H2O,chest movement during ventilation, and normal pulmonary auscultation. Then the patients were ventilated by anesthesia machine (Fabius Plus, Drager, Germany) in the following settings: tidal volume, 7 cc/kg; respiratory rate, 12/min; and exhaled tidal volume (difference between the exhaled and inhaled volumes), < 10% (monitored by anesthesia machine). To maintain a PCO2 of 30 to 35 mmHg on the capnograph, respiratory rate was adjusted again. The time interval between the insertions of device through the lips to the first leak-free ventilation with 20 cm H2O airway pressure was considered as the insertion time and measured in seconds. If the first attempt was not successful, the device would be extracted and attempted again. No delay or ventilation would be made between insertion attempts. Up to three attempts were allowed. Number of attempts to establish adequate ventilation was recorded. If the third attempt was not successful, endotracheal tube would be used. For maintenance, 100 mcg/kg/min propofol along with N2O and O2 combination (50:50) was administered. If the patient’s respiration returned, 10 mg of atracurium was re-administered. At the end of the operation, gentle circulatory oropharyngeal suctioning was performed using soft Nelaton #12 catheter. After resumption of respiration, 0.04 mg/kg of neostigmine and 0.02 mg/kg of atropine were administered to reverse the effects of the muscle relaxant. As the patient regained adequate respiratory parameters, i.e. respiratory volume, respiratory rate, and consciousness, the device would be removed and evaluated for presence of blood on device. Moreover, the patient was evaluated for hoarseness and sore throat until discharge from the recovery room. Presence of any complication would be recorded.
Data were collected and analyzed using SPSS 11 (SPSS Inc., Chicago, IL, USA). The frequency and percentage for qualitative variables and the mean and standard deviation (SD) for quantitative variables were calculated. The quantitative data were analyzed using Student's ttest.
4. Results
A total of 61 subjects were evaluated including 31 patients (50.8%) in the LMA and 30 (49.2%) in the I-Gel groups. Among demographic variables, sex (P = 0.001) (Table 1) and weight (P = 0.006) (Table 2) were significantly different between two groups. Age was not significantly different between study groups (Table 2). Placement of LMA and I-Gel was divided into three categories regarding placement on the first, second, or third attempts. Unsuccessful placement on the third attempt was considered failure and endotracheal tube was used in such cases. Results of comparison of the success rate of airway management are listed in Table 3.The difference between the two groups in regards of insertion time and attempts were not significant. Regarding complications following airway management, bleeding was seen in none of the study groups. The frequencies of sore throat and hoarseness were not significantly different between two groups (Table 3).
| Airway | Number | Minimum | Maximum | Mean ± SD | P Value |
|---|---|---|---|---|---|
| Age, y | 0.54 | ||||
| I-GEL | 30 | 21 | 70 | 40.73 ± 14.08 | |
| LMA | 31 | 22 | 56 | 42.61 ± 9.16 | |
| Weight, kg | 0.006 | ||||
| I-GEL | 30 | 48 | 80 | 64.10 ± 6.98 | |
| LMA | 31 | 45 | 87 | 70.41 ± 9.89 |
Comparison of the Mean age and Mean Weight of Patients Between the Two Groups
| Attempts, % | LMA | IGEL | P Value |
|---|---|---|---|
| LMA | 0 | ||
| Once | 80.6 | ||
| Twice | 12.9 | ||
| IGEL | 0 | ||
| Once | 66.7 | ||
| Twice | 16.7 | ||
| Thrice | 3.33 | ||
| Mean Number of Attempts | 1.25 | 1.50 | 0.17 |
| Insertion Time, s, Mean | 21.35 | 27.96 | 0.16 |
| Hoarseness, % | 0.96 | ||
| Yes | 12.9 | 13.3 | |
| No | 87.1 | 86.7 | |
| Bleeding, % | 0.8 | ||
| Yes | 0 | 0 | |
| No | 100 | 100 | |
| Sore Throat, % | 0.13 | ||
| Yes | 19.4 | 36.7 | |
| No | 80.6 | 63.3 | |
| Failure Rate, % | 0.36 | ||
| Yes | 6.5 | 13.3 | |
| No | 93.5 | 86.7 |
Comparison of the Success Rate and Complications of Airway Management by Laryngeal Mask Airway and I-GEL
5. Discussion
According to our study, I-Gel can be inserted as fast as LMA with adequate ventilation and has no major airway complications. Therefore, it could be a good alternative to LMA in emergency airway management or general anesthesia. LMA and other supraglottic airway devices have an inflatable cuff. These cuffs can cause problems during insertion, fixation, or function of the airway. Cuff over inflation causes mechanical compression, less adaptation to the larynx, and lower airway pressure. Mechanically, cuff inflation leads to airway movement in some cases. Moreover, inflatable-cuffed laryngeal mask devices might compress the veins and cause neural injury. I-Gel is different from other supraglottic airway devices due to having an acceptable stiffness and a noninflatable cuff. To have a success rate similar to that of LMA, I-Gel can be a good alternative to LMA for airway management in emergency cases or when there is a lack of expertise or absence of a laryngoscope. This study aimed to compare the success rate of LMA and I-Gel for airway management in patients undergoing elective orthopedic surgery. Among demographic variables, sex and weight were significantly different between two groups; however, these differences had no effect in our study. The insertion time, failure rate, and incidence of complications such as sore throat, bleeding, and hoarseness were compared as well. The results revealed that in the majority of patients, one attempt sufficed for airway placement. Turan et al. studied on 90 patients with ASA 1 and 2, awaiting short surgical procedures, and found no significant difference in terms of hemodynamic disturbances or time between LMA and Cobra PLA (an uncuffed airway device resembling I-Gel); however, the success rate was lower for LMA (57% versus 97% for PLA, P < 0.05). The success rates reported for LMA in their study were lower than ours, which might be attributed to the use of Cobra PLA in their study (18). In a clinical trial by Singh et al. 48 patients aged 16 to 50 years with mouth opening and neck movement limitations, who were candidate for surgery, were managed by LMA or I-Gel devices. The ventilation time and success rate were compared between the two groups. Considering the easier insertion and higher success rate of I-Gel (91.7%) in comparison to LMA (79.2%) (P = 0.000), they recommended the use of I-Gel for emergency situations and management of difficult airways (19). In a study by Siddiqui et al. 100 ASA class 1 and 2 surgical patients, aging15 to 75 years, were allocated to two groups of LMA and I-Gel and the compared in terms of easy placement of the airway and postoperative complications. They showed that the placement of both devices was easy (P = 0.65) and both were considered to be suitable alternatives for each other (20). In a study by Francksen et al. (21) no failure occurred in the I-Gel group and only one case of failure was reported in the LMA (5%). They reported similar efficacy of both devices, which was in agreement with our findings. In our study, the mean insertion time of devices was not significantly different between two groups (P = 0.1). Uppal et al. (22) reported a mean insertion time of 12.2seconds (range, 9.7-14.3) for the I-Gel and 15.2seconds (range, 13.2-17.3) for the LMA, which were significantly different (P = 0.007). They concluded that despite the significant difference in the insertion time, placement of both devices was easy and they had similar efficacy. In the study by Atef et al. (23), the mean insertion time in the I-Gel group was significantly shorter than was in LMA (P = 0.0023). In our study, no significant difference was seen between two groups in the incidence of bleeding (P = 0.8), sore throat (P = 0.13), and hoarseness (P = 0.96). In a study by Turan et al. (18), 50% of patients in the PLA group had sore throat, which was significantly different from the rate in LMA group (P < 0.05). Azarsina et al. reported that patients with LMA had higher incidence of dysphagia in comparison to patients with I-Gel (24). Independent-samples t test revealed a significant difference in this respect (P = 0.001). They reported a significant difference in the prevalence of dysphagia in compared to insignificant difference in this respect in ours, which might be attributed to the higher number of patients in their work.
Limitations of the study. Only low-risk patients (ASA class 1 and 2) with normal airways were studied, power of 40% was selected because of 35% difference in insertion success rate in previous studies. Our study reported no significant postoperative complication following the use of LMA or I-Gel. I-Gel can be used for airway management in emergency setting or when there is a lack of expertise or absence of a laryngoscope, the same as and as quick as LMA; however, its use in major surgeries or high-risk patients requires further investigations.