1. Background
Preemptive analgesia is the blocking of pain perception afferent pathways before noxious painful stimuli. As a result, perceived pain will be prevented or reduced. For this purpose, an ideal drug should be able to prevent nociceptive input and spinal pain processing sufficiently. Sedation via regional anesthesia and peripheral nerve blocks is the mainstay of improving the quality of these blocks.
Clonidine is an alpha agonist drug that is partially selective for α-2 adrenoreceptors. This drug is lipid-soluble and penetrates the blood-brain barrier. Clonidine uses different routes as adjuncts to local anesthetics and opioids or lonely to reduce pain perception. Clonidine has analgesic, sedative-hypnotic, and sympatholytic properties and an opioid-sparing effect that reduces opioid requirements without perturbing hemodynamic values.
Another benefit of using clonidine in the pre-operative period is its ability to provide excellent anxiolysis comparable to midazolam (1). Reduction in pre-operative anxiety is associated with decreased post-operative pain per se, independent of drug effects. Blockades of the nociceptive stimulus using the centrally acting α-2 adrenergic agonist clonidine before the onset of pain results in reduced pain scores, better sedation, and lower analgesic requirements after abdominal surgery (2). Even the preemptive administration of epidural clonidine was associated with a significantly lower analgesic use, lower cumulative analgesic consumption, and greater hemodynamic stability, in comparison with other groups (3). Clonidine added to local anesthetics’ results as an increased duration of anesthesia or analgesia after brachial plexus block (4).
2. Objectives
This study is designed to compare the effect of preemptive clonidine with midazolam on intraoperative sedation, duration of block, and postoperative pain scale.
3. Patients and Methods
3.1. Study Design
In a randomized clinical trial, 80 patients with orthopedic fractures of the upper extremity who underwent supraclavicular nerve block were randomly assigned to receive 0.2 mg oral Clonidine or 2 mg oral midazolam. According to one of our inclusion criteria, patients’ ages were between 20 and 60 so the recommended doses of both drugs are in the acceptable range. Randomization was performed based on accidental number and concealed allocation. Intraoperative sedation was measured at these time points: one hour after the start of surgery and then in the PACU (30 minutes after entrance to the PACU). The sensory block’s duration was measured in definite intervals after the start of the block and then at the end of surgery in the PACU, to determine the exact duration of the sensory block. Post-operative pain scores were measured after entrance to the PACU up to two hours. If the VAS was more than four, an analgesic drug (fentanyl 50 - 100 mcg) was administered to patients.
In the PACU, patients were conscious, and pinprick skin testing to evaluate the sensory blockade was readily performed, as outlines: 1, Posterior aspect of the shoulders (C4); 2, Lateral aspect of the upper arms (C5); 3, Medial aspect of the lower arms (T1); 4, Tip of the thumb (C6); 5, Tip of the middle finger (C7); 6, Tip of the pinky finger (C8); 7, Thorax, nipple level (T5); 8, Thorax, umbilical level (T10); 9, Upper part of the upper leg (L2); 10, Lower-medial part of the upper leg (L3); 11, Medial lower leg (L4); 12, Lateral lower leg (L5); 13, Sole of foot (S1).
3.2. Primary and Secondary Outcomes
The primary outcome of this study was to assess the intra- and post-operative sedation scale. The secondary outcome of this study was to assess the duration of the block and post-operative pain scores.
3.3. Sample and Setting
The University Review Board and hospital ethics committee reviewed and approved the study. All patients gave their written informed consents prior to their inclusion in the study, in accordance with University Hospital Ethics Board Committee provisions. After receiving ethical approval, 80 patients who were candidates for upper extremity orthopedic surgery and supraclavicular nerve block were enrolled in the study. Inclusion criteria were patients’ age between 20 to 60-years-old and upper extremity fractures appropriate for a nerve blockade. Exclusion criteria were any contraindication for peripheral nerve block, addiction to any drug, coagulopathy disorders, any advanced underlying disease, and psychiatric disorders.
3.4. Data Collection
After performing a supraclavicular nerve block, sedation was evaluated during surgery and in the post-operative period using the Ramsay Sedation Scale (5). The duration of the sensory block was measured by using the surgical incision during surgery, and then using with pinprick tests in the post-operative period. For this purpose, visual analogue scale (VAS) was measured every ten minutes for one hour in PACU and then every two hours in a normal ward for 24 hours. Data were extracted from completed data sheets. Pain scores were measured using VAS from 1 to 10, with “1” indicating the least amount of pain and “10” for the worst pain the subject has ever felt. To evaluate the sensory block in the PACU, patients were kept in recovery for one hour after the block regressed, and VAS scores were then measured. All demographic data were extracted from the patient profiles in their files, and all collected data were recorded in patient-specified data sheets.
3.5. Clonidine and Midazolam Administration
Patients who were randomly assigned to the clonidine group, received 0.2 mg of clonidine (Razak Laboratories Co., Iran) two hours prior to admission to the operating room (OR). If they were assigned to the midazolam group, they received 2 mg of midazolam (Exir-Iran) two minutes prior to the nerve block. The patient group and administered drug were concealed from the anesthesiologist or physician who visited patient in the post-operative period.
In cases of severe agitation or deep sedation, we routinely use haloperidol and supportive measures, respectively.
3.6. Supraclavicular Nerve Block
The brachial plexus were detected using an ultrasonography technique in both groups (by Sono Site S-Nerve ultrasound system; Linear Probe (10 - 15 MHz). Onsets of motor and sensory blocks were measured objectively by clinical testing. The qualities of the blocks were determined by lack of sensation in the hand and lack of any movement in the upper extremity muscles. Heart rate, mean arterial pressure, sedation, and the patient’s and surgeon’s satisfaction were also determined. We measured surgeon satisfaction based on a questionnaire extracted from the paper: “Clinimetric scale to measure surgeons’ satisfaction with anesthesia services,” by LeMay S, et al. Can J Anaesth.
Supraclavicular nerve blocks were performed according to Mosaffa et al. manuscript’s (6). The site of injection was sterilized, and the skin was locally anesthetized with 1.0 mL of 1% lidocaine (Caspian Tamin Pharmaceutical Co., Iran). Subsequently, a needle (Pajunk, 50 mm, 22-gauge) attached to the nerve stimulator and the syringe containing local anesthetic (40 mL of 1.5% lidocaine) penetrated the skin vertically. Initially, the nerve stimulator (Richard’s Medical Equipment, Inc., Wheeling, IL, USA) was set at 1.0 mA, 2.0 Hz, and 100 μs. Once the optimal motor response (i.e., flexion of fingers and wrist in the range of 0.3 - 0.5 mA) was achieved, local anesthetic was administered as a single injection, proceeded by aspiration.
3.7. Statistical Analysis
The data were analyzed with the Software Package for the Social Sciences (SPSS, software version 19). Data distribution and skewness were checked by histogram. Repeated measures ANOVA tests were used to compare Within-Subjects and Between-Subjects effects. Two-tailed P < 0.05 was considered as significant.
4. Results
In a randomized clinical, trial 80 patients enrolled in the study, 40 in the clonidine group and 40 in the midazolam group. All demographic variables, including age, gender, and BMI (body mass index) were not significantly different between the clonidine and midazolam groups (Table 1).
| Variables | Clonidine | Midazolam | P value |
|---|---|---|---|
| Age | 35.6 (14.5) | 37.4 (18.3) | 0.33 |
| Gender | 0.25 | ||
| Female | 13 (33) | 15 (38) | |
| Male | 27 (67) | 25 (62) | |
| BMI, kg/m2 | 22.1 (4.8) | 22.9 (3.4) | 0.65 |
| Onset of block | 5.8 (3.9) | 5.5 (4.8) | 0.41 |
| Duration of block | 176.5 (77.3) | 158.5 (72.6) | 0.059 |
| Duration of surgery | 152.7 (55.8) | 158.3 (59.6) | 0.28 |
Demographic and Block Characteristicsa
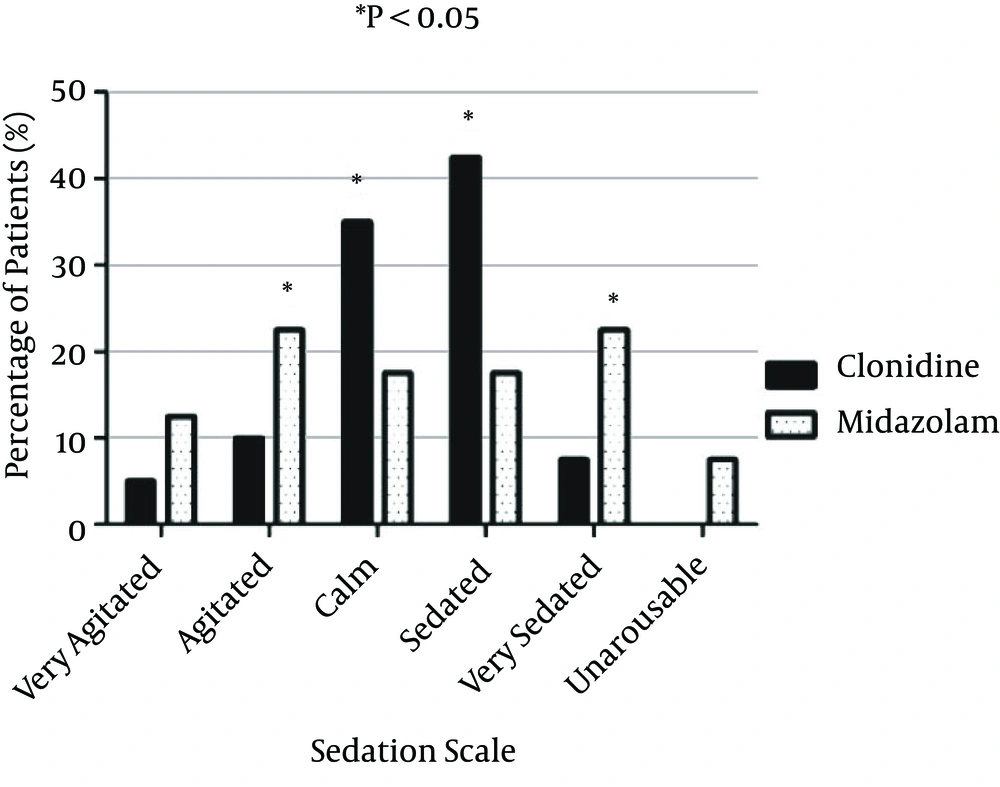
Patients’ sedation scales, as measured by the Ramsay sedation scale, were compared during surgery (right 60 minutes after the initiation of surgery). Patients in the clonidine group had significantly better sedation scale ratings than the other group. The percentages of patients in the calm and sedated scale were significantly higher in the clonidine group (35 and 42.5%, respectively), compared to the midazolam group (17.5 and 17.5%, respectively) (P = 0.042, 0.029; respectively). In addition, the percentages of patients in the agitated and heavily sedated group were significantly higher in the midazolam group, compared to this in the clonidine group (P = 0.002 and 0.014; respectively) (Figure 1).
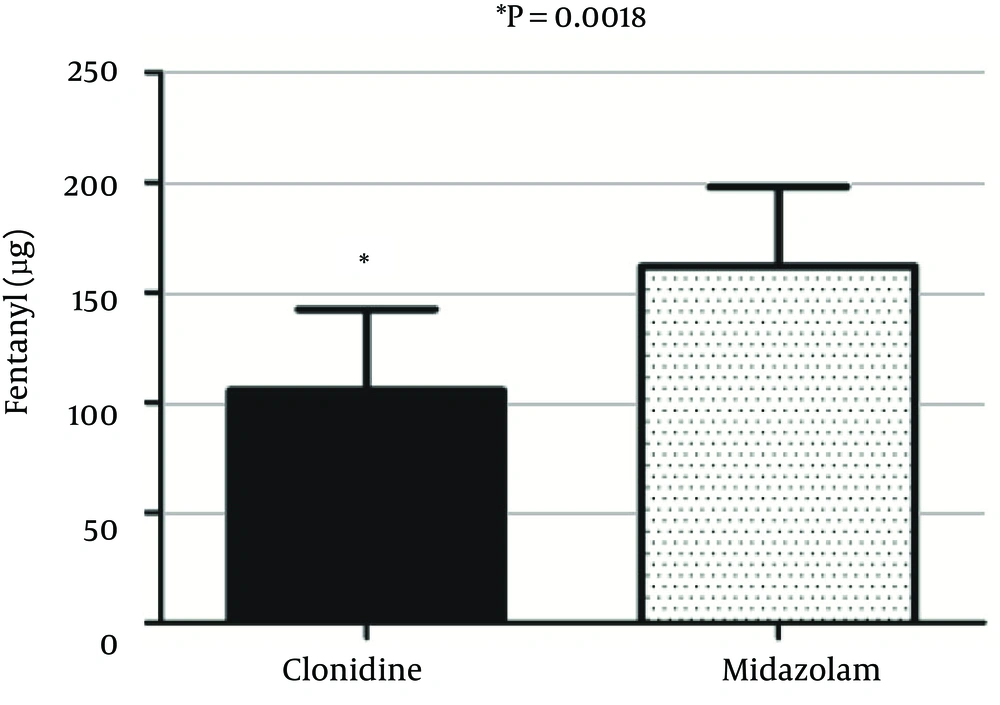
Total intraoperative fentanyl requirements were compared between the two groups of the study. The mean ± SD of intraoperatively administered fentanyl in the clonidine group (105 ± 30.8) was significantly lower than in the midazolam group (165 ± 34.5) (P = 0.0018) (Figure 2).
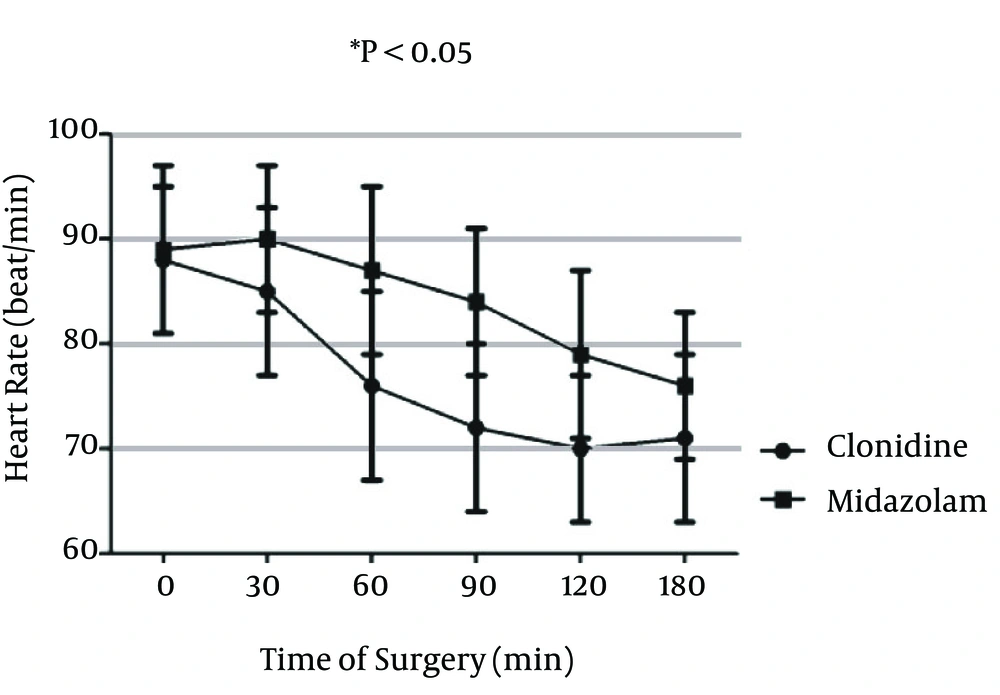
Heart rates during the operations were compared between the two groups of the study. Mean ± SD of heart rate in the clonidine group was lower than that for the midazolam group, at 0 (P = 0.51), 30 (P = 0.24), 60 (P = 0.32), 90 (P = 0.088), 120 (P = 0.072), and 180 (P = 0.095) minutes, but it was not significant at these time points (Figure 3).
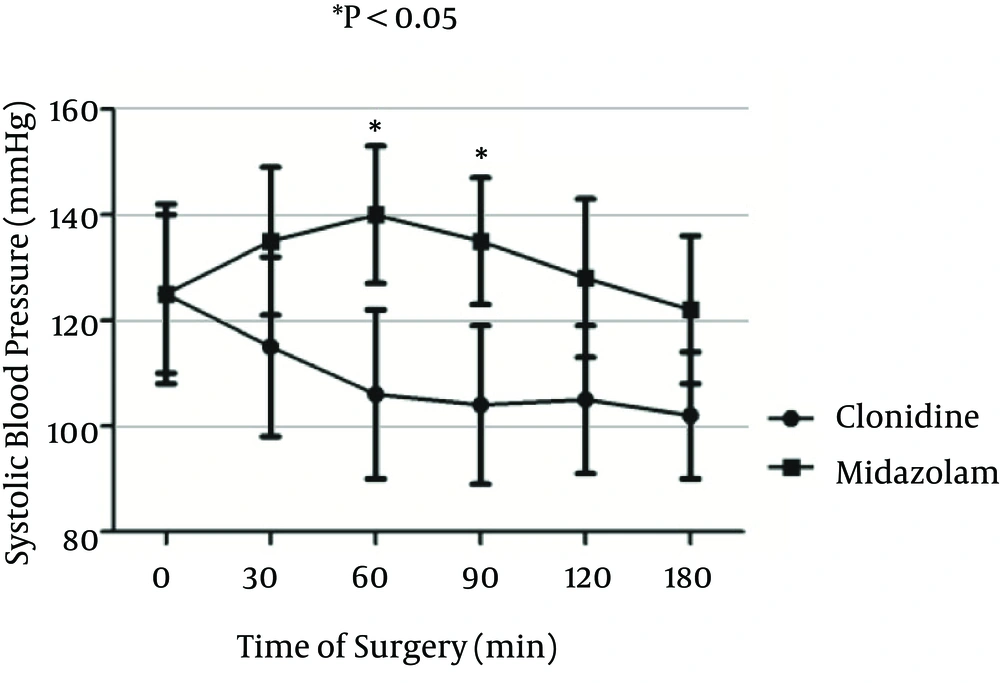
Systolic blood pressures during operation were compared between the two groups of the study. mean ± SD of systolic blood pressure in the clonidine group were was not significantly lower than that for the midazolam group, at 0 (P = 0.73), 30 (P = 0.064), 120 (P = 0.33), and 180 (P = 0.17) minutes, but it was significantly lower at 60 (P = 0.011) and 90 (P = 0.008) minutes in the clonidine group, compared to the midazolam group (Figure 4).
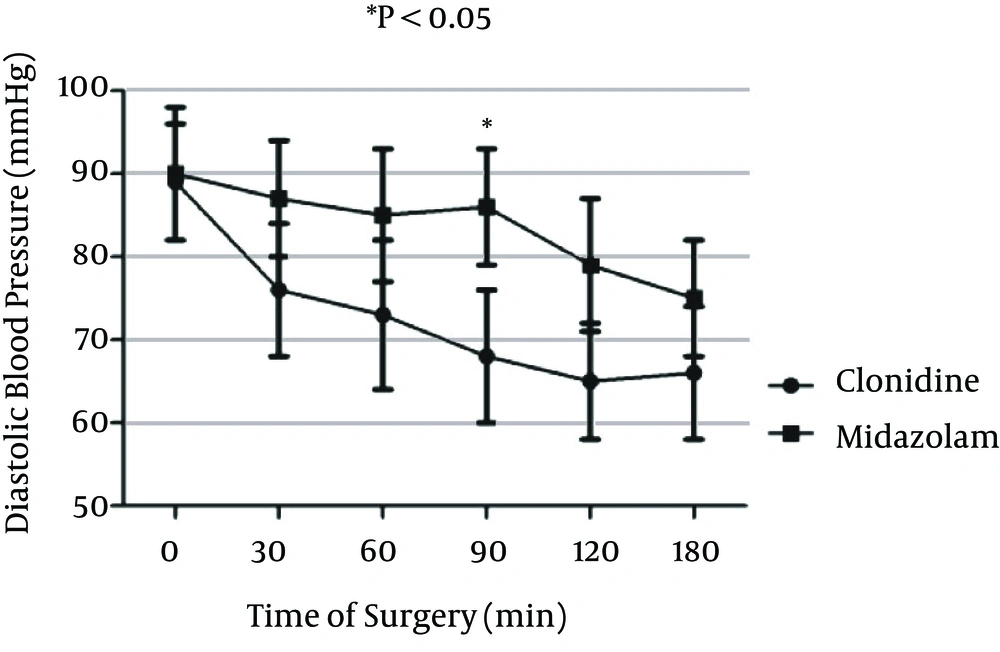
Diastolic blood pressures during operation were compared between the two groups of the study. Mean ± SD of diastolic blood pressure in the clonidine group was not significantly lower than that for the midazolam group at 0 (P = 0.60), 30 (P = 0.46), 60 (P = 0.41), 120 (P = 0.065), and 180 (P = 0.068) minutes, but it was significantly lower at 90 (P = 0.019) minutes in the clonidine group, compared to the midazolam group (Figure 5).
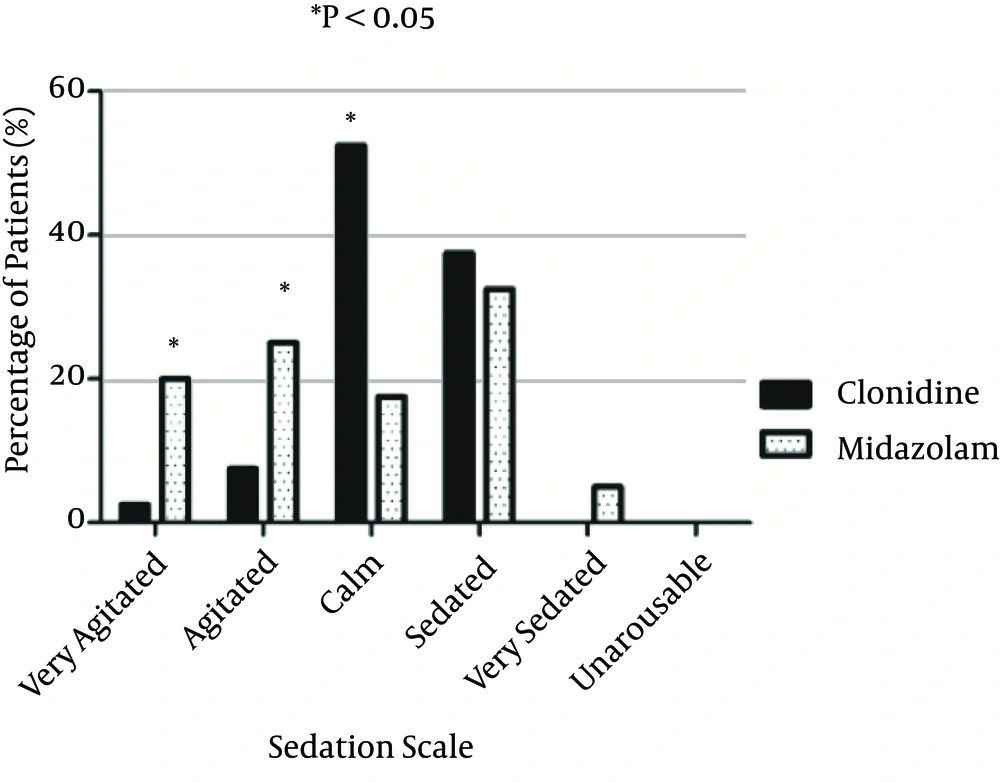
Patients’ sedation scales were measured again using the Ramsay sedation scale at the end of surgery in the PACU (30 minute after entrance to recovery). The percentages of patients in calm scale were significantly higher in the clonidine group (52.5), compared to the midazolam group (17.5) (P = 0.001) in the post-operative period. Further, the percentages of patients in the agitated and very agitated group were significantly higher in the midazolam group (20 and 25%, respectively), compared to the clonidine group (2.5 and 7.5%, respectively) (P = 0.02 and P = 0.006, respectively) (Figure 6).
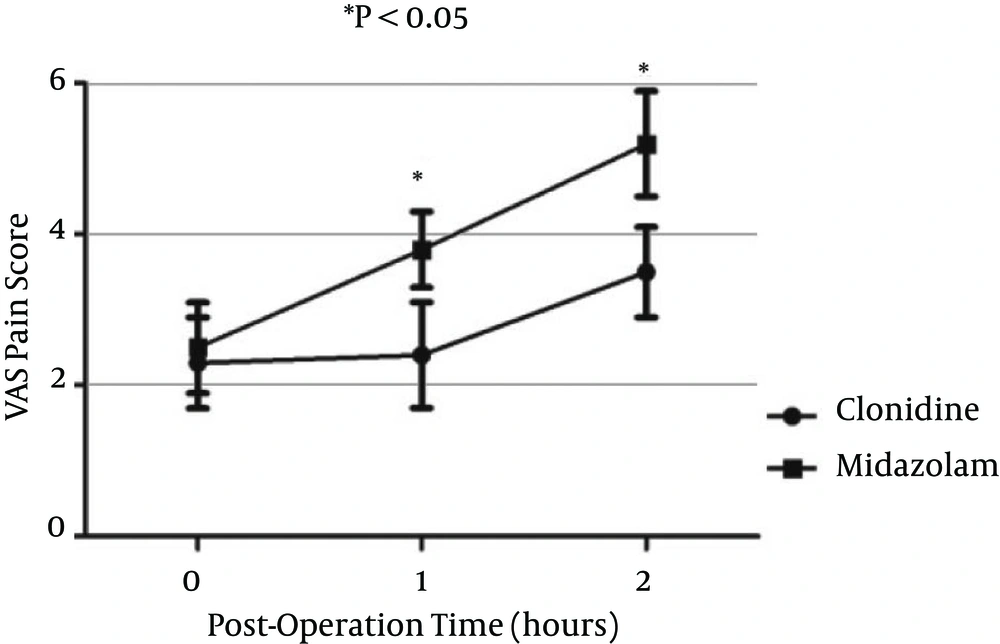
Pain scores measured by VAS during two hours post operation were compared between the two groups. VAS scores at 0 hour (entrance to recovery) were not significantly different between the two groups; however, VAS scores were significantly lower at one (P = 0.01) and two hours (P = 0.001) after operation in the clonidine group, compared to the midazolam group (Figure 7).
The total dose of administered morphine (mg) was measured during the 24 hours after surgery. Total morphine requirements were not significantly different between the clonidine (8.5 ± 5.3) and midazolam (9.3 ± 7.2) groups (P = 0.077).
5. Discussion
In this study, we compared the use of preemptive clonidine with midazolam and its effects in regional anesthesia. Variables measured were intra- and post-operative sedation, narcotic requirements during surgery, the post-operative pain scale, and other effects in patients undergoing peripheral nerve blocks.
In our patients, preemptive oral clonidine provided more appropriate sedation scale results, compared to midazolam, during surgery and in the PACU. Sedation is commonly used in patients with peripheral nerve block; however, the exact modules, dosage, or drug for sedation is always a matter of controversy. Midazolam is one of the most commonly used drugs for this purpose, but, in many instances control of the depth of sedation becomes an ordeal in these patients. In fact, under sedation and over sedation mostly happens with the use of midazolam, due to blood levels’ variability, its short duration of action, patients’ metabolisms, and body temperatures. Using clonidine overcomes many of these obstacles by providing a constant sedation during surgery and in the post-operative period. Bergendahl et al. (7) showed that premedication with clonidine was associated with a significant reduction of pain in the early post-operative period, compared to midazolam, and was also associated with moderately increased sedation during the first 24 post-operative hours.
Postoperative pain scores (VAS) were significantly lower in patients who had taken oral clonidine, compared to patients who were sedated using midazolam. Clonidine has partly alpha 2 agonist effects, which, through central nervous system (locus cereleus (8) and spinothalamic pathways (9), provides some sort of analgesic effects. The alpha 2 adrenoceptor is highly enriched in the spinal dorsal horn and involved in descending noradrenergic pain modification (10). Midazolam, on the other hand, does not show significant analgesic effects, and patients experience severe pain when the block’s effects gradually fade. In part, when patients received clonidine, they showed a significantly lower pain score, and at the same time better results on the sedation scale, which together could be seen as an attractive effect for anesthesiologists who use regional blocks in their routine practice. Oral clonidine premedication also reduces the requirement for post-operative analgesia (11).
Vital signs were more stable in patients who received clonidine, compared to midazolam, which also could be a significant advantage recommending the use of preemptive clonidine. Inside the operating room (OR), anxiety grows in patients who undergo a regional block unless appropriate sedation is provided to these patients. Although midazolam is a strong, short-acting anxiolytic drug, but previous reports on clonidine (12) offer a its potentially strong anti-anxiety effect inside the OR alongside the other benefits of clonidine mentioned above. One the other hand, the prospects of sedation and analgesia provided by clonidine in a single oral dose and excellent oral bioavailability of this drug could prompt anesthesiologists to use it for sedation in regionalanesthesia (13).
Clonidine has a long elimination half-life, and this long half-life may be partly responsible for continuation of the analgesic effects of this drug in the post-operative period, despite its preinduction use. Previous studies have shown that premedication with clonidine is superior to midazolam in producing sedation, and in decreasing post-operative pain and emergence agitation (14). Studies have demonstrated the effectiveness of oral clonidine premedication as a sedative-anxiolytic drug that helps to provide perioperative hemodynamic stability during laryngoscopy or surgery (15, 16).
In our study, the amount of narcotics required inside the OR (fentanyl) was significantly lower compared to the midazolam group. In fact, the synergistic effects of fentanyl and midazolam provide appropriate sedation and analgesia for patients in many situations. However, using fentanyl in these patients increases the risk of apnea (it requires more caution in patients with unprotected airways). Our fascinating results showed the superior effect of clonidine in decreasing fentanyl dose requirements inside the OR, compares to the midazolam group. Others have shown that preanesthetic oral clonidine consumption reduced the total requirement of propofol while stabilizing hemodynamic parameters (17).
The duration of the block was also increased in the clonidine group, compared to the midazolam group. Clonidine (18) has been used as an adjunct to local anesthetic agents in regional techniques to prolong the duration and increase the density of a block, and, ultimately, to decrease the dose of local anesthetics required. The addition of clonidine to bupivacaine and ropivacaine can extend the duration of a sensory block by a few hours, and increase the incidence of motor blocks (19). Clonidine in peripheral nerve blocks prolongs the duration of the sensorimotor blockade and post-operative analgesia without significant hemodynamic perturbations (20). Although oral clonidine has a different route of administration, compared to local injection, its receptors and route of action could be the same.
Altogether, it seems that preemptive clonidine has many marvelous advantages over midazolam, including better sedation inside the OR and then in the PACU, lower fentanyl dose requirements during surgery, more stable heart rate and blood pressure rates during the procedure, and less post-operative pain. Further studies comparing clonidine with other preemptive modalities for sedation could increase our understanding of its beneficial effects in regional anesthesia.