1. Background
Previous studies have demonstrated that shivering, which is extremely unpleasant, occurs in the postoperative period in up to 65% of the patients following anaesthesia (1). The causes for shivering include temperature loss, decreased sympathetic tone and systemic release of exogenous pyrogen substances (2). Shivering increases metabolic rate, cardiac output, peripheral vascular resistance, carbon dioxide production, lactic acidosis and oxygen consumption up to 100% and furthermore it causes a significant increase in intraocular and intracranial pressure (1, 2). Shivering interferes with electrocardiography and oxygen saturation monitoring (2). These effects make the prevention of shivering important, especially in the patients with a low cardiopulmonary reservation (2).
Various drugs have been investigated for the prevention or treatment of post-anaesthesia shivering. Among these agents, meperidine has been shown to be one of the most effective treatments (2-7). Although its mechanism of action is not completely identified, it probably acts directly on the thermoregulatory center or via opioid receptors (2-6). However, many studies in recent years have highlighted the detrimental effects of meperidine; therefore, a trend to reduce the use of this drug is gaining ground (3, 4).
Ketamine, a competitive N-methyl-d-aspartate (NMDA) receptor antagonist, plays a role in thermoregulation at multiple levels of the process. The NMDA receptor modulates noradrenergic and serotoninergic neurons in the locus coeruleus. It is used as an antishivering agent over an intravenous dose range of 0.5 - 0.75 mg/kg; however, even at these doses, it causes side effects including drowsiness, hallucination and delirium (7-9).
Doxapram is a strong dose-dependent respiratory stimulant. Researchers were of the opinion that the respiratory stimulating effect of doxapram is a result of central nervous system stimulation; however, controversy still exists as to its principal site of action. Moreover, doxapram improves arousal and the level of consciousness following anaesthesia, but significantly reduces the shivering threshold and allows the body to reach lower temperatures before shivering occurs (10). Although this reduction explains the drug’s efficacy in treatment of post-anaesthesia shivering, the exact mechanism of doxapram on shivering action is not clarified (1).
2. Objectives
The present study was conducted to compare the efficacy of meperidine and low doses of doxapram and ketamine in the prevention of post-anaesthesia shivering.
3. Patients and Methods
In this prospective, randomized, double-blind clinical trial, 120 patients, (age range, 20 - 45 years old) with an American Society of Anesthesiologists (ASA) physical status of I and II undergoing gynecologic surgery were included. All of the patients underwent general anaesthesia for an anticipated duration of 60 - 90 min. Following approval by the ethics committee, a written informed consent was obtained preoperatively from each patient. The patients were excluded from the study if they had a history of allergy, thyroid disease, Parkinson’s disease, blood transfusion during surgery, neurological or psychological disorders and hypertension and if they were pregnant. The patients were randomly allocated into three groups to receive 0.25 mg/kg ketamine (group K), 20 mg meperidine (group M) or 0.25 mg/kg doxapram (group D) with a total volume of 4 mL, which were intravenously administered immediately before wound closure.
The doses of meperidine and ketamine were considered according to previous studies (6, 10). To facilitate the double-blinding method, all the medications were prepared and injected by an anaesthetist who was not involved in the study. Thus, the patients and the observer were blinded to the groups.
Following the preparation of intravenous line, 5 cc/Kg lactated ringer’s solution, store in the operating room, was infused through peripheral venous line. The heart rate, Noninvasive Blood Pressure (NIBP) and oxygen saturation were monitored and recorded before and during the surgery. The operating room temperature was maintained at 23 ± 1°C and a standard blanket was used to cover all the patients. Anaesthesia was induced with 1.5 μg/kg intravenous fentanyl, 2 mg/kg propofol and 0.5 mg/kg atracurium. Anaesthesia was maintained with 50% nitrous oxide in oxygen and 1% - 1.5% isoflurane. The residual neuromuscular blockade was reversed and the trachea extubated, when the respiratory effort was adequate and the patients responded to verbal commands.
Nasopharyngeal temperatures were recorded following the induction of anaesthesia, at 15-minute intervals until 60 minutes after the completion of surgery. Subsequently, the difference between the first temperature and the lowest temperature (Δt) was determined for each patient.
In the recovery room, all the patients were covered with a cotton blanket and received oxygen through a facemask. Postoperative shivering was graded (8) as 0 = no shivering, 1 = mild fasciculation of the face or neck, 2 = visible muscular activity confined to one muscle group, 3 = visible muscular activity in more than one muscle group, and 4 = gross muscular activity involving the entire body. Any patient with a shivering score of > 2 was received an intravenous dose of 20 mg meperidine. Postoperative pain was assessed with visual analogue scale (VAS; 0 = no pain and 10 = worst pain) and was treated with intravenous morphine (2 mg) for VAS of ≥ 4. Side effects such as nausea and vomiting, hallucination, hypotension and bradycardia/tachycardia were recorded during anaesthesia and later for 1 hour in the postoperative recovery room.
To obtain at least 35% reduction in expected incidence, with α error of 0.05 and a β error of 0.2, a sample size of 31 patients per group was needed. Keeping in mind the drop out, we planned to study 40 patients in each group. P < 0.05 was considered statistically significant in the analysis.
Age, blood pressure, heart rate, time of anaesthesia, temperature and postoperative analgesia were compared using one-way ANOVA and the post-hoc test. Chi square analysis was used to compare differences in sex, shivering, nausea and vomiting.
4. Results
The patients’ characteristics, including age, weight and duration of surgery, were similar among the three groups (Table 1). Three patients (7.5%) in group K, four patients (10%) in group D and one patient (2.5%) in group M experienced shivering (P = 0.39). The differences in the incidence of shivering among the three groups was not statistically significant. One patient in group K and one patient in group D presented shivering at grade 2. Shivering at grades 3 and 4 was not observed in any patient.
| Items | Ketamine | Meperidine | Doxapram | P Value |
|---|---|---|---|---|
| Age, y | 31.95 ± 9.37 | 34.33 ± 12.86 | 32.23 ± 11.52 | .59 |
| Gender (M/F) | 16/24 | 20/20 | 19/21 | .64 |
| Time of Anesthesia, min | 92.50 ± 9.8 | 94.61 ± 10.96 | 90.75 ± 4.74 | .16 |
| Heart Rate, Beats/min | 84.33 ± 7.96 | 80.10 ± 9.24 | 82.53 ± 6.92 | .06 |
| Systolic Blood Pressure, mmHg | 123.10 ± 10.64 | 127.15 ± 11.64 | 125.48 ± 17.44 | .41 |
| Diastolic Blood Pressure, mmHg | 80.68 ± 7.31 | 80.68 ± 7.82 | 83.60 ± 5.66 | .1 |
| Mean Temperature, °C | 36.28 ± 0.51 | 36.36 ± 0.31 | 36.32 ± 0.31 | .64 |
Comparison of Patient Characteristics, Hemodynamic Parameters and Duration of Surgery Among the Three Groupsa
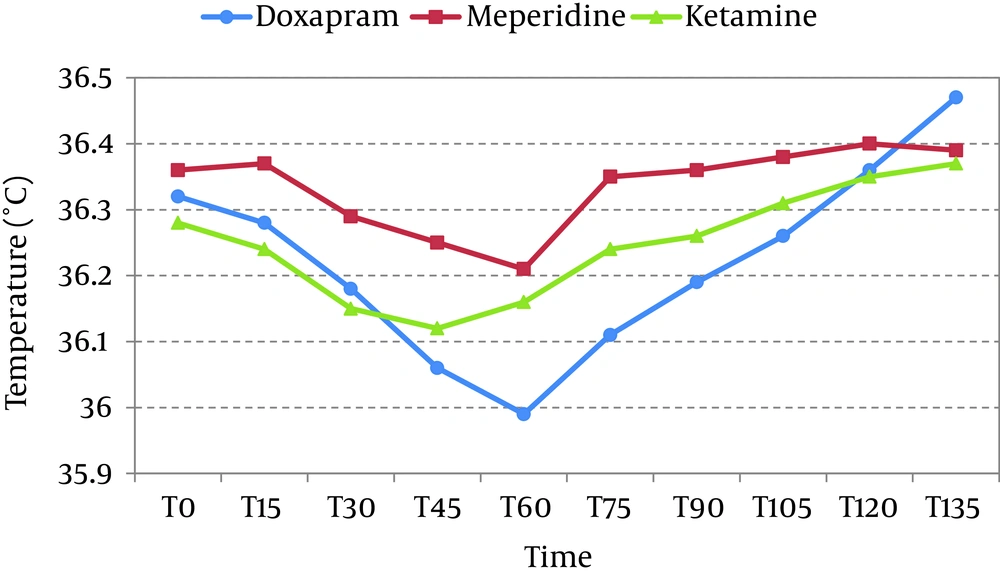
With respect to the preoperative values, the mean nasopharyngeal temperature decreased following general anaesthesia in all groups (Figure 1).The decrease in temperature in the groups K, D and M was 0.30 ± 0.26°C, 0.33 ± 0.35°C and 0.46 ± 0.33°C, respectively (P = 0.07). There was no statistically significant difference among groups in nasopharyngeal temperature during perioperative period (Figure 1).
The mean time of the first analgesic request was significantly prolonged in group K (47.37 ± 9.47 minutes) and group M (45.57 ± 7.66 minutes) compared with group D (15.7 ± 2.54 minutes) (P < 0.001).
Peripheral oxygen saturation did not decrease below 95% in any patient throughout the recovery period. Three patients (7.5%) in group M, two patients in group K and two patients in group D suffered from nausea and vomiting (P = 0.85). Hallucination, bradycardia/tachycardia and hypo or hypertension was not observed in any of the patients. No significant adverse effects were recorded during the study.
5. Discussion
In the present study, we observed that the prophylactic prescription of meperidine, ketamine and doxapram was effective in prevention of shivering during general anaesthesia without causing any adverse effects.
Various pharmacological therapies have been used to prevent postoperative shivering, of which meperidine has been shown to be one of the most effective treatments (1). Meperidine most probably, acts on the thermoregulatory center or via opioid central receptors. Ketamine is a competitive receptor antagonist of NMDA, which has a role in thermoregulation at various levels (7-9).
Perhaps, ketamine controls shivering by nonshivering thermogenesis. In the present study, a very low dose of ketamine (0.25 mg/kg) was as effective as meperidine (20 mg) in prevention of posta-anaesthesia shivering. The dosage of the drugs used in our study were selected arbitrary base on our previous observation, though previous studies demonstrated that 0.25 mg/kg ketamine and 20 mg meperidine were effective in preventing shivering during the postoperative period (7, 10). Dal et al. (7) found no significant differences between the efficacy of ketamine (0.5 mg/kg) and meperidine (20 mg) in preventing postanaesthetic shivering. Sagir et al. (8) observed that intravenous ketamine (0.5 mg/kg) effectively prevented shivering during regional anaesthesia, with minimal side effects.
In another investigation by Bhukal et al. (11) reported that the pre induction low-dose meperidine does not decrease the incidence of postoperative shivering. The prophylactic use of ketamine was effective in preventing shivering during neuraxial anaesthesia without causing any major adverse effects (12). Gangopadhyay et al. (13) concluded that ketamine (0.5 mg/kg intravenously) was effective in preventing shivering following spinal anaesthesia.
Two studies that compared the efficacy of doxapram and meperidine in the treatment of postanaesthetic shivering found that both drugs were effective (14, 15). Komatsu et al. (16) found that doxapram at a measured plasma concentration of 2.5 μg/mL considerably reduced the shivering threshold, which explains the efficacy of doxapram in the treatment of postoperative shivering.
Our study demonstrated that ketamine and meperidine have an analgesic effect, which may be suitable because since both drugs improve patient compliance and maintain cardiovascular stability. During the first hour after the surgery, all patients in the groups K and M needed analgesics. This can be explained by the short duration of action of low-dose meperidine (20 mg) and ketamine (0.25 mg/kg). Dal et al. (7) reported that in the postoperative period, the time of the first analgesic requirement in the saline group was shorter than that in the ketamine or meperidine group.
One of the drawbacks of ketamine is hallucinations, though none of our patients reported this effect. Minimal adverse effects in our study can be explained by the low dose of ketamine or perhaps, the side effects were masked by the general anaesthesia. This particular side effect of ketamine should always be kept in mind. Ayatollahi et al. (17) reported that 0.5 and 0.3 mg/kg ketamine was effective in the prevention of postanaesthetic shivering, but 0.5 mg/kg ketamine caused hallucinations in their study.
In this study, no difference in the heart rate and blood pressure was observed among the three groups. Dal et al. (7) did not observe any hemodynamic changes in the ketamine (0.5 mg/kg) and the meperidine (20 mg) groups. These results are in agreement with those of the study by Ayatollahi et al. (17) in which no hemodynamic changes were observed with ketamine. Indeed, no hemodynamic changes have been associated with doxapram in previous studies (13, 16).
Only three patients in the meperidine group and two patients in ketamine and doxapram groups in our study experienced nausea and vomiting. The favourably low incidence of nausea and vomiting was probably multifactorial. Associated factors might include the use of propofol for induction of anaesthesia, low dose of meperidine, doxapram and ketamine and use of minimal dose of opioids.
A control group was not included in our study because we believe that meperidine is the most effective treatment to prevent shivering. However, this may be considered as a limitation in our study. Besides, the absence of the postoperative discharge time can be mentioned as another defect in our study.
It can be concluded that a low prophylactic dose of ketamine (0.25 mg/kg), doxapram (0.25 mg/kg) or meperidine (20 mg) immediately before wound closure is equally effective in the prevention of postoperative shivering. Moreover, when meperidine is not ideal for prevention of postanesthesia shivering, doxapram and ketamine can be effective alternatives.