1. Background
Laryngoscopy and tracheal intubation, as a painful procedure, is commonly used for airway management during general anesthesia. This procedure is frequently associated with hemodynamic disturbances including tachycardia, hypertension, arrhythmia or other undesirable hemodynamic changes (1, 2). These hemodynamic changes are among the hazardous complications of general anesthesia (3, 4). Numerous studies have been performed to evaluate many induction agents such as etomidate, thiopental, propofol, ketamine, midazolam and fentanyl for attenuating hemodynamic responses to laryngoscopy. All these pharmacologic agents have their own pros and cons and no single agent is the most appropriate for this purpose (1, 2, 5-7).
Etomidate is an IV anesthetic induction agent used prior to laryngoscopy and endotracheal intubation. It possesses unique desirable properties such as rapid onset and short duration of action, relative cardiovascular and respiratory stability, as well as neuroprotective effects, making it as an attractive induction agent to facilitate intubation (8, 9). Despite these benefits, one area of concern exists regarding etomidate use in anesthesia. It is believed that etomidate may cause profound and persistent adrenocortical suppression by inhibiting mitochondrial 11 β hydroxylase enzyme of the adrenal steroid synthesis pathway (1, 10-12). Cortisol is essential for general adaptation to stress and plays a decisive role in cellular and organ homeostasis maintenance. It has been shown that in patients undergoing elective surgery, cortisol response to surgery was absent 48 hours after the administration of a single bolus of etomidate (13, 14).
Ketamine is a short-acting general anesthetic with distinct cardiovascular effect. Unlike many anesthetics, it stimulates the cardiovascular system. This is characterized by increase in HR, BP and cardiac output (CO) (8). Thiopental is an ultra-short-acting barbiturate commonly used for the induction of anesthesia. It may cause dose-dependent decrease in systemic vascular resistance, stroke volume and CO, leading to compensatory tachycardia (1, 8). Propofol (2, 6 di-isopropylphenol) is an ultra-short-acting sedative-hypnotic agent, widely used for induction during general anesthesia. It causes a dose-dependent hypotension and respiratory depression greater than thiopental (15). It theoretically seems that combined use of such drugs may balance the opposing hemodynamic effects. Lately, administration of simultaneous use of several anesthetic agents (co-induction) to promote induction of anesthesia has been better credited, particularly when its advantages over mono-therapy are established. This technique is applied to produce more appropriate desired outcomes with fewer adverse effects compared to single drug use (16, 17).
2. Objectives
Considering the importance of attenuating hemodynamic responses to laryngoscopy and endotracheal intubation and paucity of information comparing etomidate, combination of propofol-ketamine and thiopental-ketamine effects as induction agents, we aimed to compare the effects of these induction agents on hemodynamic response to laryngoscopy and intubation.
3. Patients and Methods
After obtaining an approval from the ethics committee of Mazandaran University of medical sciences and informed consents from patients, a total of 120 patients of both sexes, aged between 18 - 45 years, with the American society of anesthesiologists (ASA) class I and II, scheduled for elective surgery under general anesthesia in Imam Khomeini hospital (Sari, Iran) were enrolled in this prospective, double blind randomized clinical trial. The G*Power Version 3.1 (Heinrich Heine, Universitat Dusseldorf) was used for sample size calculation and the followings were used for the calculation; Test family = F test, Statistical test = ANOVA (Repeated measures between factors), Effect size f = 0.20, alpha error probability = 0.05, 1-beta error probability = 0.80, Number of groups = 3, number of measurements = 4, correlation among repeated measures = 0.3. The total sample size was calculated as 120 (40 in each group). The study was performed between December 2011 and January 2013 and registered in the Iranian clinical trials database (IRCT201103114365N7; http://www.irct.ir).
Patients with history of adrenal insufficiency, asthma, hypertension, suspected difficult airway, receiving general anesthesia during the previous week, receiving steroid during the past 6 months, sensitivity to etomidate, propofol or thiopental, sensitivity to egg and soya, pregnancy, chronic inflammatory diseases and serious psychiatric, endocrine or neurological illnesses were excluded from the study. Participants who met the inclusion criteria were randomly allocated to three groups (groups A, B and C) using the random number tables, by an anesthetic nurse who was unaware of the study groups.
After establishing a venous access on the forearm of nondominant hand, all patients received an infusion of 5 ml/kg lactated Ringer’s solution. After completion of infusion, systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial blood pressure (MAP) and heart rate (HR) were measured and recorded as baseline values. For premedication, all patients received midazolam (0.02 mg/kg) and fentanyl (3 µ/kg). One minute later, the hypnotic drugs were administered to each group for anesthesia induction. Patients in group A received etomidate (0.3 mg/kg) plus normal saline as placebo. Patients in groups B and C received propofol (1.5 mg/kg) plus ketamine (0.5 mg/kg) and thiopental sodium (3 mg/kg) plus ketamine (0.5 mg/kg), respectively. All medications were provided at the same volume and the syringes were covered with masking tape to conceal any details of product. Loss of eyelash reflex was used as the induction end point.
After hypnotic drug administration, succinylcholine (1.5 mg/kg) was administered as a muscle relaxant to facilitate intubation. One minute later, laryngoscopy was performed by an anesthesiologist blinded to the study groups. Immediately after laryngoscopy and tracheal intubation and one and three minutes after the procedures, the hemodynamic values (SBP, DBP, MAP and HR) were measured. If SBP decreased to less than 20% of the baseline, 10 mg ephedrine was administered and recorded in questionnaire.
Moreover, a nurse who was unaware of the study groups recorded the occurrence of muscle twitching after hypnotic drug administration, as well as the incidence of nausea and vomiting during recovery from anesthesia. The primary outcome of this study was hemodynamic changes (SBP, DBP, MAP and HR) after laryngoscopy and intubation and the secondary outcome was the incidence of muscle twitching and postoperative nausea and vomiting (PONV) in the three study groups.
3.1. Statistical Analysis
Data was analyzed using SPSS 16 statistical software (SPSS Inc., Chicago, IL). Qualitative data was analyzed using chi-squared test and quantitative data was analyzed by a mixed-design analysis of variance model. P-value below 0.05 was considered statistically significant.
4. Results
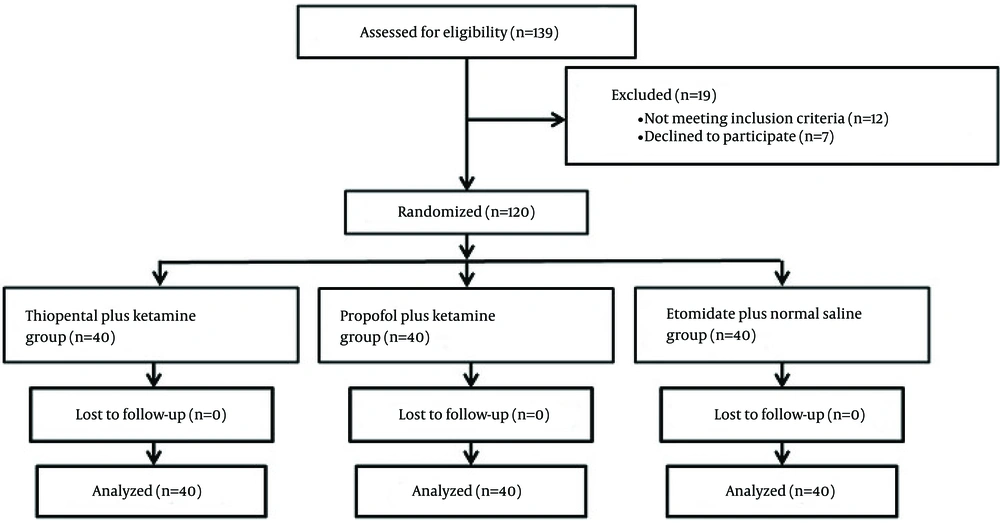
A total of 139 consecutive patients were screened during the study period. Of these, 12 patients did not meet the inclusion criteria and 7 declined to participate in the study. The remaining 120 patients were randomly allocated to three groups. All of these patients completed the study and their data analyzed (Figure 1).
Basic demographic and clinical characteristics of patients in the three groups are presented in Table 1. As shown in Table 1, there were no statistically significant differences between the groups.
| Variables | Group A (Etomidate/Normal Saline) | Group B (Propofol/Ketamine) | Group C (Thiopental/Ketamine) | P-Value |
|---|---|---|---|---|
| Gender | .64 | |||
| Male | 21 (34.4) | 22 (36.1) | 18 (29.5) | |
| Female | 19 (32.2) | 18 (30.5) | 22 (37.3) | |
| Age, y | 31.30 ± 8.52 | 29.75 ± 6.92 | 32.27 ± 7.05 | .23 |
| Body mass index, kg/m2 | 26.15 ± 3.58 | 25.24 ± 3.16 | 26.49 ± 5.94 | .42 |
aData are expressed as the mean ± standard deviation or number (%).
Distribution of all variables was check by Kolmogorov-Smirnov Z test, which were normally distributed (P-value > 0.05). Table 2 shows mean and 95% CI of hemodynamic variables in different treatment groups in baseline measurements and three time intervals after the intervention.
| Measurement Time/ Hemodynamic Variable | Etomidate | Thiopental-Ketamine | Propofol-Ketamine | P-Value |
|---|---|---|---|---|
| Baseline Measurement | ||||
| Systolic BP | 128.65 (124.80 - 132.49) | 132.42 (128.48 - 136.3) | 130 (125.59 - 134.40) | .408 |
| Diastolic BP | 79.35 (79.27-82.42) | 81.35 (78.05 -84.64) | 77.60 (74.87-80.32) | .215 |
| Mean Arterial BP | 93.20 (89.34-97.05) | 95.25 (93.75-98.74) | 91.27 (86.72-93.22) | .125 |
| Heart Rate | 89.45 (83.51 - 93.38) | 85.65 (80.04 - 91.25) | 97.62 (93.10 - 102.14) | .021 |
| First Measurement (Immediately after intervention) | ||||
| Systolic BP | 125.17 (120.86 - 129.48) | 122.47 (117.56 - 127.38) | 127.75 (122.18 - 133.31) | .317 |
| Diastolic BP | 78.27 (74.55 - 81.99) | 75.1 (71.85 - 78.34) | 74.35 (71.33 - 77.26) | .207 |
| Mean Arterial BP | 92.60 (88.979 - 96.40) | 89.17 (85.91 - 92.43) | 87.17 (83.62 - 90.72) | .91 |
| Heart Rate | 84.55 (80.16 - 88.93) | 86.55 (81.62 - 91.47) | 96.42 (92.35 - 100.49) | > .0001 |
| Second Measurement (One minute after intervention) | ||||
| Systolic BP | 145.10 (137.12 - 153.07) | 139.92 (134.03 - 145.81) | 123.82 (117.09 - 130.55) | > .0001 |
| Diastolic BP | 92.90 (86.71 - 99.02) | 91.40 (86.48 - 96.31) | 77.37 (73 - 81.74) | > 0.0001 |
| Mean Arterial BP | 107.17 (100.98 - 113.38) | 107.80 (102.50 - 113.09) | 88.22 (82.50 - 93.94) | > .0001 |
| Heart Rate | 94.67 (88.41 - 100.93) | 92.05 (86.80 - 97.29) | 97.62 (94.69 - 100.55) | .285 |
| Third Measurement (Three minute after intervention) | ||||
| Systolic BP | 138.45 (130.60 - 146.20) | 138.12 (133.30 - 142.94) | 119.67 (114.16 - 125.18) | > .0001 |
| Diastolic BP | 84.55 (78.37 - 90.72) | 86.90 (83.04 - 90.75) | 76.30 (73.45 - 79.14) | 0.003 |
| Mean Arterial BP | 99.07 (92.45 - 105.09) | 104.05 (100.95 - 107.14) | 86.32 (83.07 - 89.57) | > .0001 |
| Heart Rate | 89.25 (83.03 - 95.40) | 89.12 (83.33 - 94.91) | 95.17 (92.05 - 98.29) | .171 |
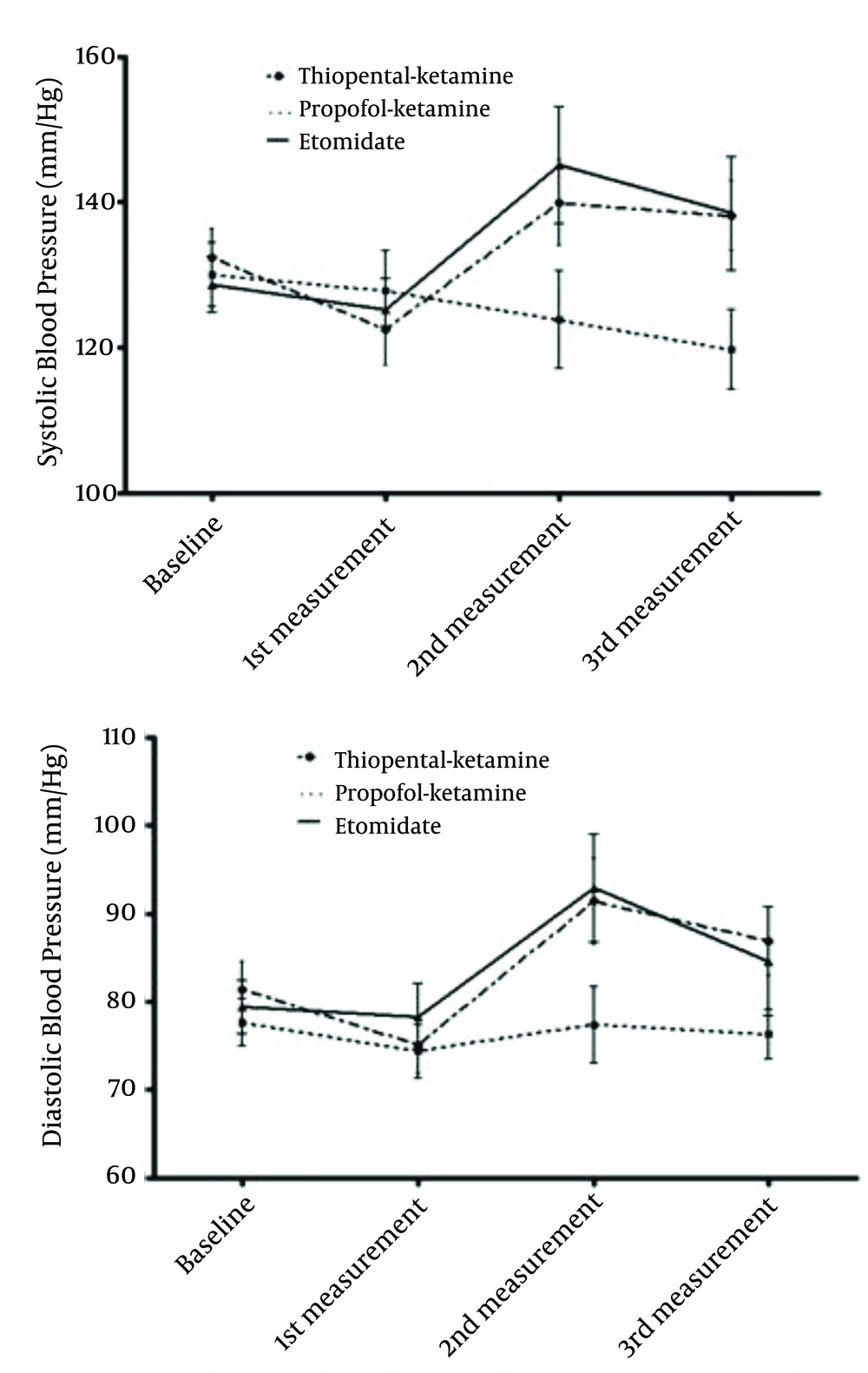
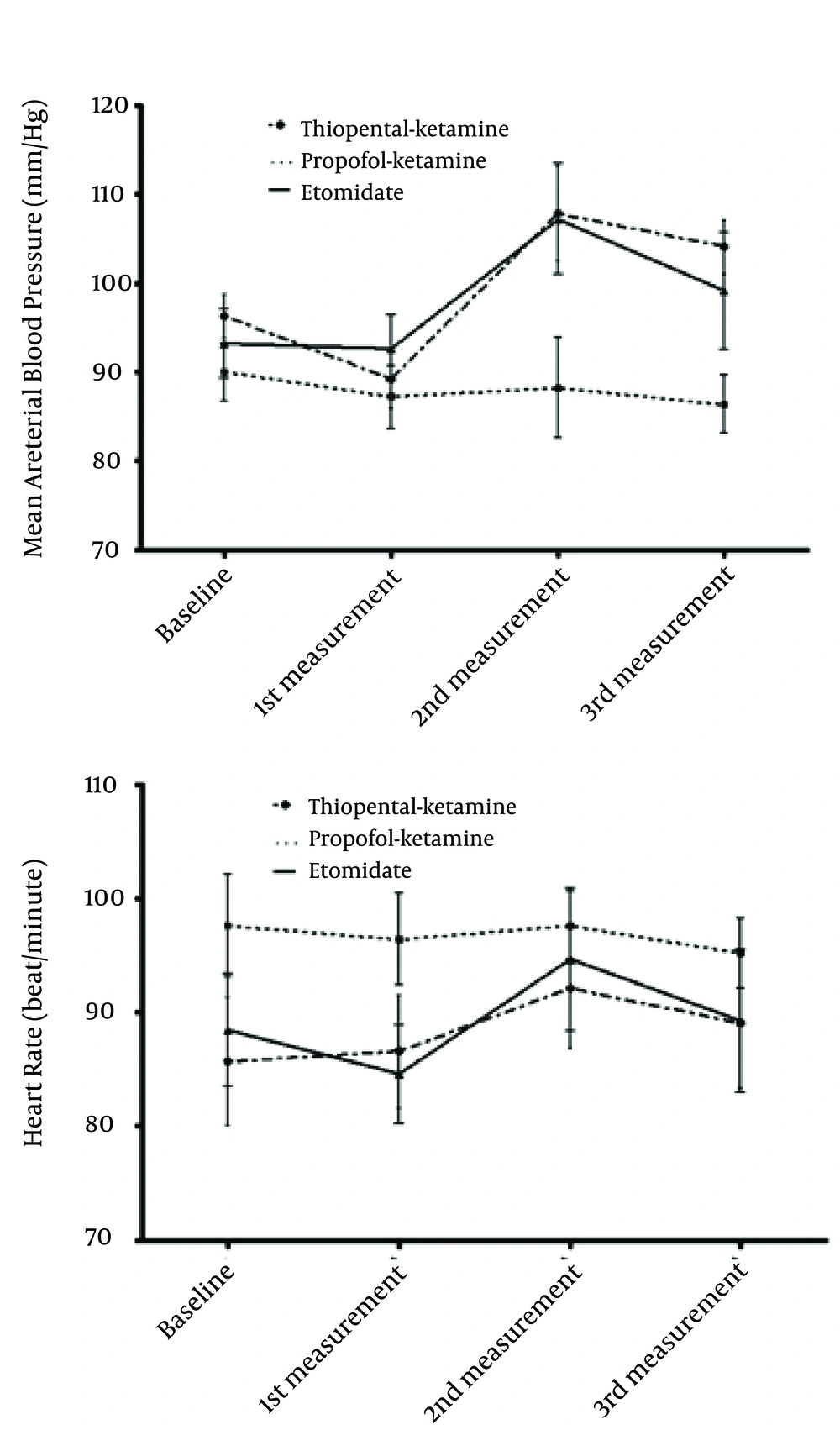
Figures 2 and 3 show changes in SBP, DBP and MAP as well as HR during the study period in different treatment groups. A repeated measurement ANOVA with a Huynh-Feldt correction test showed significant changes in mean SBP and DBP between the time points, (F (2.541, 297.354) = 15.228, P-value < 0.0001) and (F (2.539, 297.054) = 27.654, P-value < 0.0005), respectively. In addition, the main effect of MAP and HR, corrected by Huynh-Feldt, were statistically significant during the course of study, (F (2.586, 302.611) = 27.894, P-value < 0.0005) and (F (2.770, 324.069) = 7.36, P-value < 0.0005), respectively. Furthermore, after induction of anesthesia, the three study groups had significant different SBP, DBP and MAP changes overtime, (F (5.083, 297.354) = 12.085, P-value < 0.0005), (F (5.078, 297.054) = 5.413, P-value < 0.0005) and (F (5.173, 302.611) = 9.057, P-value < 0.0005), respectively. However, HR changes overtime were not statistically significant (F (5.540, 324.069) = 21.13, P-value = 0.065).
Muscle twitching, as well as PONV was more prevalent among patients who received etomidate than the other two groups (Table 3). No adverse effects were reported in the propofol-ketamine group.
In addition, a series of Post Hoc analysis were conducted to compare systolic and diastolic blood pressure, mean arterial pressure and heart rate of the propofol-ketamine group with the other two groups (Table 4).
| Group | SBP | DBP | MAP | HR |
|---|---|---|---|---|
| Etomidate | ||||
| Difference of estimated marginal mean | -9.03 | -7.36 | -10.09 | 7.48 |
| P-value | .011 | .002 | < .0001 | .034 |
| Thiopental Na-ketamine | ||||
| Difference of estimated marginal mean | -7.93 | -7.28 | -11.39 | 8.37 |
| P-value | .031 | .003 | < .0001 | .014 |
5. Discussion
We compared the effects of etomidate, combination of propofol-ketamine and combined thiopental-ketamine as induction agents on hemodynamic response to laryngoscopy and intubation. One of the major findings of this study was that the patients receiving propofol-ketamine combination had better hemodynamic stability compared with the other groups. The other main finding was that none of patients in propofol-ketamine combination group had muscle twitching as well as PONV; whereas, 14 patients in thiopental-ketamine and etomidate groups developed muscle twitching and PONV.
In a study by Garg et al. aimed to evaluate hemodynamic effects of different doses of propofol, ketamine and their combination as induction agents in ambulatory gynecological surgeries, combination of 1 mg/kg Propofol and 1 mg/kg Ketamine produced better hemodynamic stability (18). Saleem et al. showed that ketamine-propofol combination provides superior hemodynamic stability compared to propofol-thiopental combination during anesthesia induction, laryngoscopy and tracheal intubation (19). A study by Furuya et al. showed that administration of ketamine before induction with propofol preserved hemodynamic stability compared with induction with propofol alone (20). Another study by Ghatak et al. showed that addition of ketamine with propofol provides hemodynamic stability in children premedicated using clonidine for insertion of laryngeal mask airway (LMA) (21). However, Ozgul et al. showed that ketamine-propofol combination provided minimal hemodynamic changes during insertion of laryngeal tube-suction (22).
Anesthesia-induced hemodynamic fluctuations are a matter of concern for anesthesiologists. Research evidence indicates that these hemodynamics alterations are independently associated with postoperative complications in patients undergoing surgery. Therefore, many induction agents have been used by anesthesiologists to minimize these hemodynamic alterations (1, 23). Etomidate is a unique induction agent with minimal hemodynamic effects, which has wide safety margins. In spite of its potential benefits, etomidate can suppress adrenocortical steroid synthesis and also increase PONV (8, 24). Lundy et al. reported one case of adrenal Insufficiency after administration of a single dose of etomidate for anesthesia induction (25). A study conducted by O’Leary et al. showed that after administration of a single bolus dose of etomidate in patients undergoing gynaecological surgery, the cortisol response to surgery was absent for 48 hours; whereas, in the thiopental group, circulating cortisol increased significantly after the operation (14).
Unfavorable effects of etomidate and importance of co-induction to promote induction of anesthesia in patients undergoing surgery encouraged us to evaluate combinations of some anesthetic agents with opposing hemodynamic effects, on hemodynamic responses to laryngoscopy and intubation in patients undergoing surgery. Considering the opposing effects of propofol and ketamine on hemodynamic parameters, it seems that combination of them at a lower dose can decrease overall side effects and summates the advantages of each agent (26). This assumption has been confirmed by our study. Theoretically, it seems that concurrent administration of thiopental and ketamine with opposing hemodynamic effects, like propofol-ketamine combination, might be complementary and minimize overall adverse effects of each drug. The results of our study showed that thiopental-ketamine combination produced somewhat better hemodynamic stability compared to etomidate, but propofol-ketamine combination resulted in significantly better hemodynamic stability compared to these two induction regimens. Habibi et al. showed that hemodynamics changes induced by ketamine-thiopental combination versus etomidate for anesthetic induction in patients with impaired ventricular function were not statistically different (1). Another study by Firoozabadi et al. to compare the effect of thiopental-ketamine combination with thiopental alone on hemodynamic changes by laryngoscopy and intubation in patients undergoing cesarean section, showed no significant differences between the two groups regarding hemodynamic parameters after laryngoscopy and intubation (27). The results of a recently published study by Aghdaii et al. to investigate hemodynamic effects of propofol-ketamine combination compared with etomidate-midazolam mixture during anesthesia induction in patients with left ventricular dysfunction undergoing coronary artery bypass graft (CABG) surgery, showed that both anesthetic regimens were acceptable for induction in these patients (28).
The results of our study showed that none of patients in propofol-ketamine group had PONV, whereas approximately 30% and 10% of patients in etomidate and ketamine-thiopental groups had PONV, respectively. This finding was anticipated because propofol has antiemetic property. Sumer et al. showed that etomidate causes more PONV compared to propofol (29). The antiemetic mechanism of propofol is not completely elucidated. This property may be due to either its sedative effect or modulation of subcortical pathway and probably its weak serotonin antagonist effect (30).
A limitation of this study was that while all groups were given the same premedication with fentanyl 3 µ/kg and midazolam 0.02 mg/kg, the dosages per kg body weight of these drugs may be unequally distributed between groups, and thus the dosing of these premedication drugs may be a confounding variable.
In conclusion, propofol-ketamine combination may be recommended as an effective and safe induction agent for attenuating hemodynamic responses to laryngoscopy and intubation, with superior hemodynamic stability compared to etomidate and combination of thiopental-ketamine in patients undergoing surgery in general anesthesia. Although, further well-designed randomized clinical trials to confirm the safety and efficacy of this combination, especially in patients with cardiovascular disease or critically ill patients undergoing surgery, are warranted.