1. Background
To prime the cardiopulmonary bypass (CPB) circuit, a number of colloids are used in addition to crystalloids to preserve the oncotic pressure and decrease the fluid retention after CPB (1, 2). Among them, human albumin may be beneficial as it conserves the coagulation system and decreases inflammatory reaction. However, its cost and possibility to transfer infections limit general use of albumin (1).
Six percent hydroxyethyl starch (HES) 130/0.4 (6% Voluven Inj., Fresenius Kabi, Germany) is an artificial colloid with a stronger plasma-expanding effect than crystalloids, less occurrence of allergic reaction and less cost compared to albumin (3, 4). Like other colloids, HES can cause dilutional coagulopathy and reduction of factor VIII and von Willebrand factor levels. HES can also decrease the availability of glycoprotein IIb/IIIa on the surface of platelets. However, because of a lower molecular weight and molar replacement percentage than other starches, Voluven has been shown to keep plasma-expanding effects with a small effect on coagulation and greater plasma clearance (5-8). In several meta-analyses, the use of human albumin in cardiac surgery was compared to HES and was shown to better decrease postoperative hemorrhage and reserve the coagulation system (7, 9-14).
Furthermore, postoperative acute kidney injury (AKI) is one of the most frequent and severe complications after coronary artery bypass grafting (15, 16). In previous studies, acute kidney injury has been occurred in up to 30% of patients on coronary artery bypass grafting. Progression of kidney injury is related to high short-term and long-term mortality (17, 18). Even slight alterations in serum creatinine that can happen in the postoperative period are associated with a generous decrease in survival (19). Additionally, preoperative renal dysfunction, diabetes, peripheral artery disease, age and the technique and length of cardiopulmonary bypass are considered as risk factors for AKI (20).
2. Objectives
Thus, we aimed to investigate the effects of 5% albumin and 6% HES 130/0.4 as priming solutions for cardiopulmonary bypass grafting heart surgery on renal function of patients and to study the association between each priming solution with coagulation, postoperative blood loss and renal function.
3. Patients and Methods
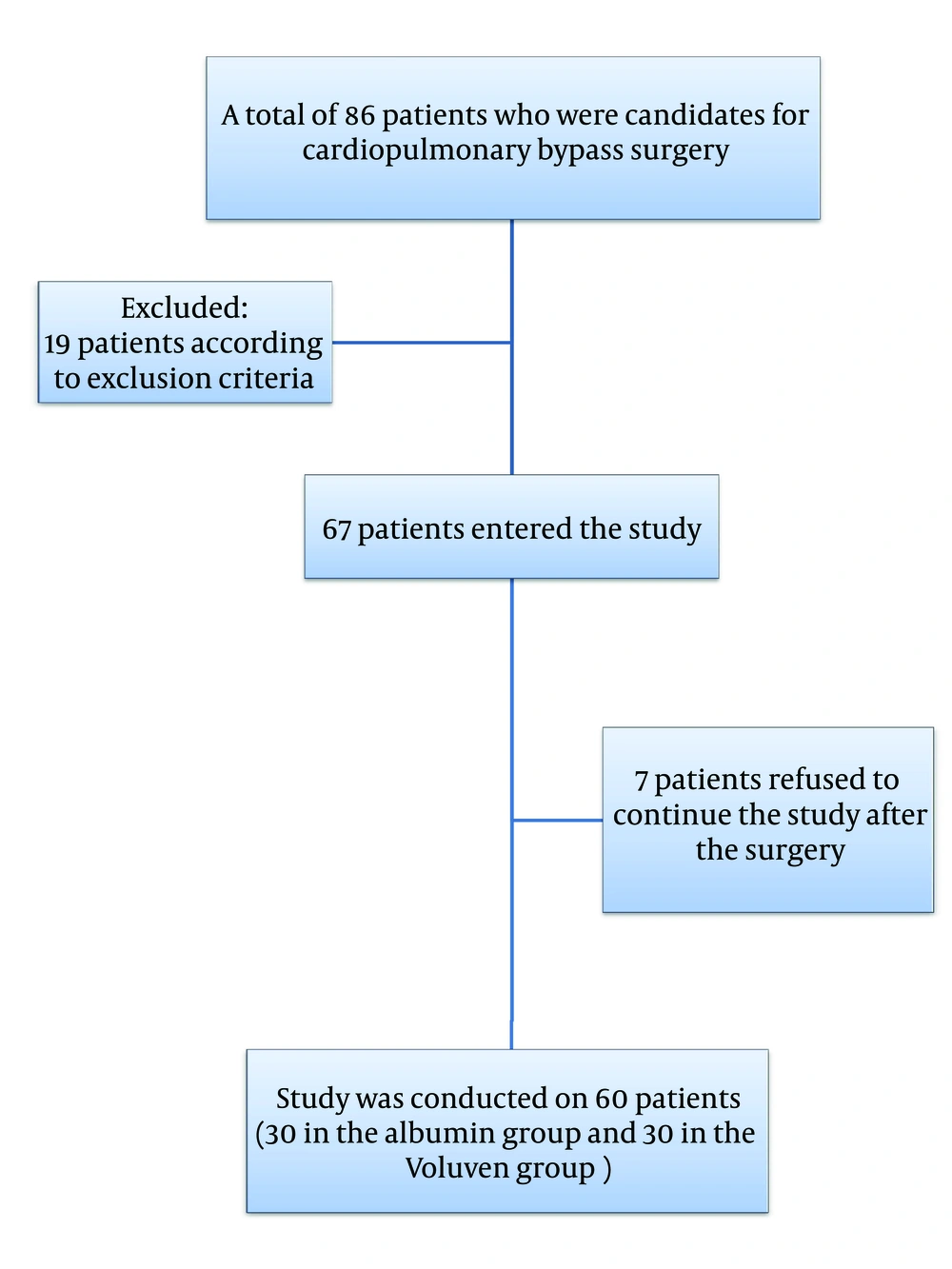
Sixty patients scheduled for elective coronary artery bypass grafting (CABG) surgery between January 2012 and November 2013 were involved in this double blind clinical trial study. These patients were classified by the American Society of Anesthesiology (ASA) as classes II and III. The study was approved by “Birjand university of medical sciences ethics committee” (institutional review board of Birjand university of medical sciences) and all patients gave their informed consent before surgery. The study was registered in the Iranian registry of clinical trials (IRCT) by number IRCT2015011620112N4. The exclusion criteria were emergency surgery, history of cardiac surgery, history of receiving medication with antiplatelet agents except ASA 80 (mg/day) within the previous five days, preoperative coagulation disorder, left ventricular ejection fraction less than 50%, preoperative renal dysfunction (serum creatinine > 1.4 mg/dL), preoperative hepatic dysfunction (serum aspartate/alanine amino transferase > 60 U/l), preoperative electrolyte imbalance, known hypersensitivity to HES and chronic diuretic therapy. Preoperative ASA 80 (mg/day) and Atorvastatin 20 (mg/day) were continued in all patients. Angiotensin II receptor antagonist and angiotensin converting enzyme inhibitors were discontinued 24 hours before the operation in all patients. By considering inclusion and exclusion criteria, 60 isolated CABG cases were studied (Figure 1). Based on the study of Tiryakioglu et al. (21) considering α = 0.05, β = 0.01, 99% power, allowable difference (µ2 - µ1) = 0.26 and population variance = 0.0361 postoperative INR at the 24th hour, the sample size was calculated from the below formula:

Thus, n1 and n2 were calculated as 20, which gave us a total sample size of 40. To be more precise, the final sample size considered as 60 (30 in each case and control group) (22).
A computerized randomization table was used to allocate patients to two groups. Patients received 500 mL of either 5% human albumin dissolved in 0.9% normal saline (Na+ 154 mmol/L, Cl- 154 mmol/L) (Albumin group, n = 30) or 6% HES 130/0.4 in 0.9% sodium chloride (VoluvenW %, Fresenius Kabi, Bad Homburg, Germany) (HES group, n = 30) as priming solution as part of the 1500 mL total priming solution used for the CPB circuit. Finally, the priming solution included NaHCO3 7.5% (45 mEq), 20% mannitol (5 mL/kg), heparin (10 mg/L) and normal saline for both groups. During the operation and in intensive care unit, colloid solutions were not used.
All patients were pre-medicated with 5 mg of intramuscular morphine two hours before the operation. Anesthesia was induced with Etomidate (2 mg/kg), Midazolam (0.01 mg/kg), Sufentanil (1.5 μg/kg) and Cisatracurium (0.2 mg/kg). Anesthesia was maintained with a continuous infusion of Sufentanil (0.2 - 0.3 μg/kg/h), Cisatracurium (2 μg/kg/min) and Isoflurane (0.6 - 1.5%) in 100% oxygen and Propofol (25 - 100 μg/kg/min) during CPB based on patients bispectral index (BIS), which was kept between 40 and 60.
Heparin (primary bolus 3 mg/kg) was administered before establishment of CPB. After inducing anticoagulation with heparin, activated clotting time (ACT) was kept over 380 seconds. CPB was established with a membrane oxygenator (Terumo System 1TM, Terumo, Leuven, Belgium) with target flow rates of 2.4 to 2.8 L/min/m2 for all patients. Leukocyte-depleted packed red blood cells (PRBCs) were given when hemoglobin was below 7 g/dL. Moderate hypothermia to 32°C and cold (4 - 8°C) cardioplegia concentrations were the same (K+ 20 mmol/L for arrest induction and 10 mmol/L for maintenance) in all patients. Furthermore, α-stat acid-base gas managing was used and the goal range for PaO2 was 200 - 300 mmHg. Throughout CPB, norepinephrine or nitroglycerin was used to maintain arterial pressure between 60 - 80 mmHg. Heparin was reversed with protamine sulfate (1 mg per 1 mg of heparin). Before weaning out from CPB, All patients were rewarmed to 36°C. There was no difference in surgical technique between patients.
After the operation, all patients were transferred to the intensive care unit (ICU) and mechanically ventilated. Tracheal extubation was performed when hemodynamics were stable, axillary temperature was > 36°C and there was a satisfactory spontaneous breathing (PaO2 > 70 mmHg with Fio2 0.4, breathing frequency < 15/min) with blood gas parameters being in a normal rang. Postoperatively, fluid therapy was used to keep the central venous pressure between 7 and 10 mmHg and urine output above 1 mL/kg/h. Fresh frozen plasma (FFP) was transfused when the INR was more than 1.5 and platelet concentrates were transfused in case of platelet count less than 50,000 μL/L after the operation. An exploratory surgery was designated when bleeding was more than 400 mL during the first hour postoperatively or more than 200 mL/h during 6 hours after the operation, regardless of a normal active clotting time (ACT) and all other coagulation parameters. A hematocrit of less than 21% was the cut point for transfusion of PRBCs.
The following data were recorded for all patients; demographic data (sex, age), baseline serum creatinine level (mg/dL) with isotope dilution mass spectrometry (IDMS), glomerular filtration rate (GFR) calculated with Creatinine Clearance formula (CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration):

where Scr is serum creatinine (mg/dL), κ is 0.7 for females and 0.9 for males, α is -0.329 for females and -0.411 for males, min indicates the minimum of Scr/κ or 1, and max indicates the maximum of Scr/κ or 1. Left ventricular ejection fraction with transthoracic echocardiography (%), comorbidities (diabetes, dyslipidemia, hypertension, chronic obstructive pulmonary disease, cerebellar vascular accident, smokers, recent myocardial infarction) and preoperative hemoglobin value (g/dL) were assessed. The following data were registered during the operation; graft count, CPB duration and cross clamp time. The postoperative collected data included serum creatinine level (mg/dL) at 24, 48 and 72 hours postoperation, GFR at 24, 48 and 72 hours postoperation, peak postoperative change in creatinine level (change from baseline) and peak postoperative change in GFR (change from baseline). Blood loss was carefully measured in the perioperative period for up to 24 hours after the operation. All the units of PRBCs, FFP and platelets transfused were also recorded for up to 24 hours.
3.1. Statistical Analysis
Data was analyzed by SPSS 14.0 (SPSS Inc., USA) and expressed as mean ± SD or the number of patients. Data between the groups compared using a chi-squared test, Fisher’s exact test, independent t-test or Mann-Whitney U test, as appropriate. For intragroup comparisons of variables to baseline values, repeated measures analyses of variance followed by a post hoc Dunnett’s test were used. P value < 0.05 considered as statistically significant.
4. Results
No significant difference was observed between the characteristics of two groups including age, sex, cardiovascular risk factors and preoperative renal function (GFR (P = 0.51), Cr (P = 0.056)). In addition, there was no significant difference between the coagulation status of the two groups; PT (P = 0.48), PTT (P = 0.73) and INR (P = 0.24) (Table 1).
| Variables | Albumin | Starch | P Values |
|---|---|---|---|
| Gender, m/f | 21/9 | 17/13 | .36 |
| Age | 66.07 ± 8.82 | 61.85 ± 9.10 | .75 |
| EF | 38.51 ± 10.81 | 36.5 ± 10.99 | .49 |
| Cr-start | 0.96 ± 0.18 | 0.88 ± 0.15 | .56 |
| Hb-start | 13.16 ± 2.00 | 13.52 ± 1.28 | .83 |
| Graft count | 4.15 ± 0.60 | 4.33 ± 0.763 | .29 |
| Pomp time | 109.33 ± 16.28 | 112.39 ± 13.25 | .42 |
| Clamp time | 67.89 ± 12.68 | 70.61 ± 10.60 | .37 |
| Trans-PC | 2.89 ± 1.64 | 3.24 ± 1.52 | .392 |
| Trans-FFP | 0.7 ± 1.38 | 0.91 ± 1.75 | .623 |
| Trans-Plt | 3.52 ± 4.09 | 2.36 ± 4.18 | .288 |
| RISK factors | |||
| T2D | 15 | 12 | .137 |
| HLP | 10 | 8 | .282 |
| HTN | 17 | 16 | .262 |
| COPD | 1 | 1 | .885 |
| CVA | 1 | 0 | .265 |
| Recent MI | 9 | 13 | .628 |
| smoker | 6 | 3 | .156 |
aP values were calculated using Chi-squared test, Fisher’s exact test, independent t-test or Mann-Whitney U test, as appropriate.
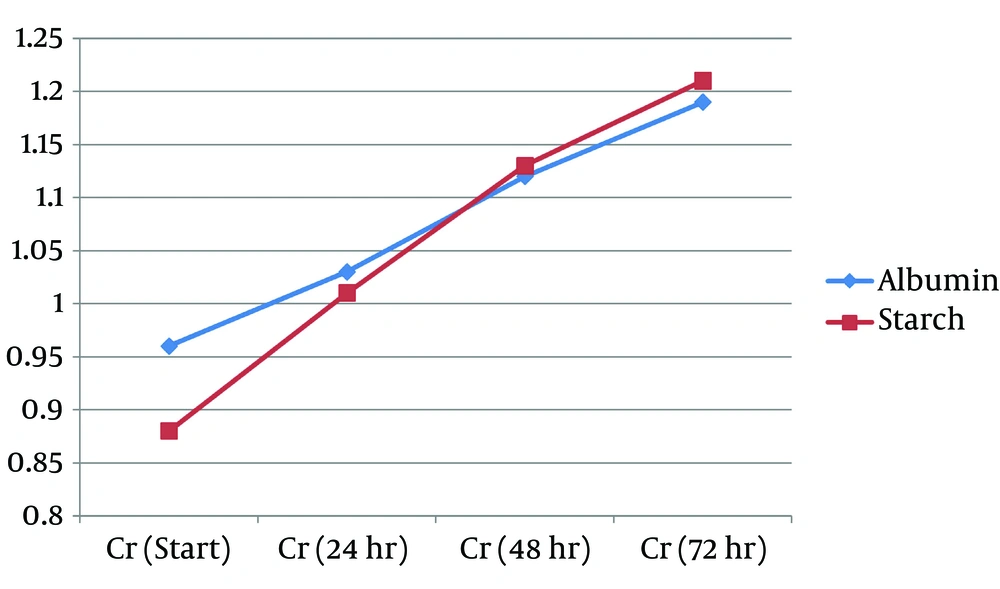
GFR in the Albumin group was higher at 24, 48 and 72 hours postoperatively, but it was not statistically significant (Table 2). GFR differences were statistically lower in Albumin group compared to HES (Voluven) group at 24 hours (-4.82 ± 8.04 vs. -12.14 ± 6.06, P < 0.0001), 48 hours (-12.69 ± 8.01 vs. -20.20 ± 9.47, p=0.002) and 72 hours (-16.39 ± 10.12 vs. -24.71 ± 12.44, P = 0.007) postoperatively (Table 3 and Figure 2). Figure 3 shows changes in creatinine levels of the two groups during postoperative period.
| Variable | Albumin | Starch | P Values |
|---|---|---|---|
| Serume Cr | |||
| 24th hour | 1.03 ± 0.2 | 1.01 ± 0.16 | .70 |
| 48th hour | 1.12 ± 0.2 | 1.13 ± 0.18 | .89 |
| 72nd hour | 1.19 ± 0.2 | 1.21 ± 0.2 | .59 |
| GFR | |||
| 24th hour | 71.37 ± 20.71 | 67.34 ± 16.3 | .40 |
| 48th hour | 63.5 ± 14.57 | 59.27 ± 14.32 | .26 |
| 72nd hour | 59.8 ± 14.45 | 54.76 ± 13.07 | .16 |
aP values were calculated using Students’ T-Test.
| Variable2 | Albumin | Starch | P Values |
|---|---|---|---|
| Cr-difference | |||
| 24th hour | 0.06 ± 0.08 | 0.13 ± 0.05 | .001 |
| 48th hour | 0.16 ± 0.08 | 0.25 ± 0.09 | .000 |
| 72nd hour | 0.22 ± 0.10 | 0.33 ± 0.13 | .001 |
| GFR-difference | |||
| 24th hour | -4.82 ± 8.04 | -12.14 ± 6.06 | .000 |
| 48th hour | -12.69 ± 8.01 | -20.20 ± 9.47 | .002 |
| 72nd hour | -16.39 ± 10.12 | -24.71 ± 12.44 | .007 |
| PT-diffrence | 15.97 ± 41.53 | -1.29 ± 26.27 | .15 |
| PTT-diffrence | 8.2 ± 21.50 | 2.1 ± 6.4 | .25 |
| INR-diffrence | 0.58 ± 0.32 | 0.50 ± 0.29 | .46 |
| Plt-diffrence | -48.28 ± 65.56 | -142.36 ± 107.21 | .007 |
| Bleeding | 799.84 ± 382.75 | 1121.00 ± 584.58 | .017 |
aP values were calculated using Students’ T-Test.
The coagulation tests changes (PT difference, PTT difference and INR difference) were not statistically different between the two groups (P = 0.154, P = 0.254 and P = 0.465, respectively); however, platelet count was significantly lower in Albumin group compared to the HES (Voluven) group. Early postoperative bleeding was statistically lower in Albumin group compared with HES (Voluven) group (799.81 ± 382.75 vs. 1121 ± 584.58, P = 0.017) (Table 3).
5. Discussion
In this study, we found that using human albumin compared with HES (Voluven) in CBP prime solution in patients with normal renal function can result in lower amounts of bleeding, lower reduction in platelet count, lower increase in serum creatinine level and lower decrease in GFR after elective CABGs (up to 72 hours). Coagulation laboratory data like PT, PTT and INR did not show any significant changes between the two groups, but platelet count was lower in the first 24 hours in HES (Voluven) group. The amount of bleeding was higher in HES (Voluven) group; however, usage of FFP, packed red blood cells, and platelet concentration were not different between the two groups.
Increased bleeding after cardiac surgery is always a problem in CPB (23, 24). Artificial extracorporeal circulation results in activation of coagulation system, fibrinolysis, platelet consumption, and hemodilutional decrease in coagulation factors (1, 7, 10). We know that the priming solution used for CPB may affect coagulation status. We added HES to priming solution to decrease fluid retention after cardiopulmonary bypass; however, use of albumin was better because of the lower reduction in coagulation factors. Moreover, use of albumin in priming CPB can result in the formation of a non-thrombogenic layer on the surface of CPB circuit and this can reduce the affinity of platelets to the artificial surface. Mimicking the endothelial surface by using human albumin can cause this phenomenon (25, 26). In contrast, many studies showed that HES can compromise the coagulation system when used as a volume expander and priming CPB pump (13, 27-30). The effect size of HES on the coagulation system is closely related to its in vivo molecular weight, molar substitution ratio and C2/C6 ratio. It has been shown that because of lower molecular weight of HES (Voluven), it can cause lower effect on homeostasis than the other older starches (4). Although, in other clinical studies use of Voluven as a part of priming solution is restricted (31). However, in another study in congenital cardiac surgery, use of Voluven as a volume expander compared with human albumin decreased the need for transfusion and had better effect on fluid balance (32). In those studies, use of Voluven did not have any effects on routine coagulation tests like PT, PTT and platelet count in contrast to our study. Choi et al. (1) studied the effects of HES when used as a priming solution compared with human albumin and they did not determine any difference on coagulation tests, transfusion amounts and blood loss, which is in contrast to our result. In a meta-analysis published in 2001, Wilkes and coworkers (25) compared the risk of postoperative bleeding after administration of older HES formulas (with either high or medium molecular weight and a high degree of substitution) in cardiac surgeries. Albumin and HES were administered as volume replacement prior to and after cardiopulmonary bypass (CPB), respectively, and also as constituents of the priming fluid of the extracorporeal circuit (heart-and-lung machine). Results of nine trials involving 354 patients showing the effects of a first-generation starch and albumin were compared. Postoperative blood loss was significantly lower in patients who received albumin than those who received HES. However, no significant difference was observed between a more modern synthetic colloid solution compared to albumin.
In this study, we compared changes in renal function by serum creatinine and GFR in two groups and found that in human albumin group renal dysfunction was lower than HES (Voluven) group. In a cohort study by Frenette et al. (16), Albumin had a dose-response association with the risk of AKI, which was also equivalent to have a higher prevalence of related risk factors for AKI. The positive association was also observed in patients without postoperative hemodynamic instability. The findings of this cohort about the effects of human albumin on renal function were opposite to our results, but usage of human albumin in this cohort study was during the 96-hour postoperative period and not as a priming solution for CPB.
This study had some limitations. First, clearance of creatinine and rise in serum creatinine are delayed indicators of developing AKI and use of biomarkers for early detection of AKI might be a better method. Secondly, we did not have any data on long-term post operation morbidity and mortality of patients. Finally, our significant results were only observed comparing changes of Cr and GFR between the two groups, while the level of CR and GFR were not different. Moreover, the differences cannot reflect a clinical importance.
In this randomize clinical trial study, we found that using human albumin 5% versus HES had advantages such as a lower reduction in platelet count and an increase in postoperative bleeding. Additionally, patients undergoing CPB with HA 5% had lower decrease in renal function levels. Further studies should be conducted to better evaluate different priming solutions for CPB pump.