1. Background
Despite recent advances in minimal invasive surgery, postoperative pain control remains as a challenge for both surgeons and anesthesiologists (1).
Currently, laparoscopy has an obvious favor for both diagnostic and therapeutic procedures of pelvic and abdomen; while it is minimally invasive, has less pain, and needs less postoperative analgesic use compared with open surgeries (2). Shoulder pain is a frequent problem following laparoscopic procedure (3, 4). Many patients may feel much more discomfort from their shoulder pain than incision pain (5). PLSP is caused by irritation and/or injury of the diaphragm and phrenic nerve by local acidosis and irritative effect of CO2 during pneumoperitoneum or distention forces on the diaphragm (6-9).
Gabapentin is a 3-alkylated analog of Gamma-Amino Butyric Acid (GABA). Its effects are via alpha-2 delta calcium channel subunits modulation. Gabapentin prevents the release of nociceptive neurotransmitters such as norepinephrine, substance P, glutamate, and calcitonin gene-related peptide by binding to α-2 subunit of voltage-gated calcium channels (10-12).
Recent studies focused on the efficacy and safety of gabapentin as a non-opioid analgesic to control postoperative pain in different groups of patients (13-17). However, the prophylactic use of oral pain killers remains to be described in different pain syndromes. While there are few trials on the effect of gabapentinoids in postoperative shoulder pain, none of them tried to descript their effect on shoulder pain after laparoscopic ovarian cystectomy.
2. Objectives
The current study aimed to assess the efficacy of prophylactic administration of gabapentin in prevention and/ or attenuation of PLSP after laparoscopic ovarian cystectomy.
3. Patients and Methods
Approved by Ethics and Clinical Studies Committee of Tehran University of Medical Sciences, the study was registered in the Iranian Registry of Clinical Trials (IRCT201103166076N1) and Australian-New Zealand Clinical Trial Registry (ACTRN1261000269932).
It was a double-blind randomized placebo controlled clinical trial, in which 40 pre-menopausal females, who had written consent, were participated. All patients had ASA class I-II and scheduled for elective laparoscopic cystectomy in Woman's Hospital, Tehran University of Medical Sciences, from April 2011 to March 2012.
Patients with the following characteristics were excluded from the study: Body Mass Index (BMI) ≥ 40, Consuming any pain killers routinely within 48 hours before the surgery, smoking, drug abuse, having a major psychiatric disorder, epilepsy or history of convulsion, any known kidney or hepatic disorders, history of any other pervious laparotomy, laparoscopy, or other pelvic manipulation or pathology except normal vaginal delivery, history of chest or mediastinal surgery or pathology, recent flu (six weeks before surgery), suspected to malignancy as pathology, and those who complained from shoulder pain just before surgery in the first Visual Analog Scale (VAS) assessment.
The exclusion criteria were considered as: shift from laparoscopy to laparotomy, complicated surgery (i e, bleeding), and persistent pain after scheduled pain killers or after 48 hours (that may have different pathology and needs more clinical attention). Replacing all possibly excluded cases was scheduled according the row number.
As patients were taken to the operation theater, a 10 cm (11 point) VAS, (0 = no pain and 10 = worst pain in their life) was employed to scale their pain. Based on simple randomization by balloting sequential numbers from a box in front of one of secretaries blinded to the study, patients were randomly assigned to two groups of study. As assigned by the anesthesia team, patients received uniformed capsules as an oral premedication 30 minutes before surgery, either gabapentin 600 mg (case group) or placebo (control group). Both groups took the medication with about 50 mL regular water. Both capsules were of identical color and appearance and were packed and numbered by the local pharmacy, randomly. Placebo group had glucose powder in the capsules. Anesthesia group, patients, surgeons, and other personnel remained blinded to the randomization until data processing time.
All patients were fasting at least for eight hours prior to the surgery. All patients received a balanced general anesthesia and laryngeal intubation with Macintosh laryngoscope by one attending anesthesiologist who was blinded to the groups. Following midazolam 2 mg intravenously, remifentanil 0.2 µ.kg-1min-1infusion was initiated. Anesthesia Induction was performed by propofol 2.0 - 2.5 mg.kg-1 and maintained by propofol infusion of 0.1 - 0.2 mg.kg-1min-1 during the surgery. Atracurium 0.5 mg.kg-1 and thereafter intermittent 0.15 mg.kg-1 bolus doses were used to relax the muscles. Mechanical ventilation was performed for all patients with a 100% O2. The Tidal Volume (TV) and/or respiration frequency were adjusted to maintain end tidal CO2 at the level of 32 - 35 mmHg. CO2 gas was used for abdominal Insufflations and to maintain the intra-abdominal pressure maximum at 12 mmHg. The surgical team and instruments were the same for both groups and were blinded to the study. Standard national monitoring included continuous electrocardiography, pulse oximetry intermittent noninvasive blood pressure monitoring, and capnography.
Operation time was recorded for each patient. Just after abdominal desufflation, remifentanil infusion was removed and a blouse dose of 0.075 mg fentanyl was administered and following skin closure, propofol was discontinued. Antagonization of neuromuscular block was performed by neostigmine 50 µg.kg-1 and atropine 20 µg.kg-1. After tracheal extubation, patients were transferred to the recovery room. When patients requested more analgesia in the recovery room, bolus incremental doses of fentanyl (25 - 50 µg) was titrated for the patient’s comfort. All patients received ibuprofen tablet 400 mg on the evening of operation day and on the next morning as well as acetaminophen (325 mg) plus codeine (8 mg) orally on their request for analgesics. In the case of sustained nausea or vomiting, ondansetron 4 mg was administered, intravenously.
The presence and severity of PLSP was recorded as the primary outcome, using a Visual Analog Scale (VAS, 0 = no pain and 10 = worst ever felt pain) 30 minutes before surgery and thereafter 2, 6 and 12 hours after surgery by a blinded research nurse. Patients were followed up just for 24 hours after surgery.
3.1. Statistical Analysis
By calculating mean VAS scores in the other studies that had assessed gabapentin in pain syndromes other than PLSB; the observed VAS in the gabapentin treated group was 2.1, compared with 3.6 in the placebo group. According to the significance level of 0.05 and a power of 0.8, it was calculated that the sample size of 20 cases in each group would be adequate to detect a clinically relevant reduction of the pain level. Statistical tests were performed using SPSS 13.0 (SPSS Chicago, II, USA). Continuous variables (Continues variables killed BMI, Age, duration of sUrgery, and VAS) were analyzed using student T-test. Nominal parametric data were analyzed using the Fisher exact or Mann-Whitney tests. The ANCOVA with repeated measure test was used to assess the results. Results were reported as absolute value, means, or numbers.
4. Results
One patient who had shifted from laparoscopy to laparotomy was replaced with another subject based on the row number and the same premedication was applied to her. Therefore, after assessment for eligibility, 40 patients were enrolled into the study.
All patients were females aged 16 - 44 years old with the mean age of 27.5 years. Patients weighed 50 - 78 kg and the mean BMI was 24.5 kg.m-2.
Age, BMI, pregnancy history, and surgery time were statistically similar between the two groups under study (Table 1).
| Gabapentin (n = 20) | Placebo (n = 20) | P Valueb | |
|---|---|---|---|
| Age, years | 26.5 ± 7.4 | 28.5 ± 9.2 | 0.446 |
| BMI, kg.m-2 | 25.1 ± 4.0 | 23.9 ± 5.9 | 0.280 |
| Duration of surgery, minutes | 77.3 ± 28.5 | 67.9 ± 20.2 | 0.232 |
| Positive pregnancy history | 4 (20) | 2 (10) | 0.660 |
| PLSP | 9 (45) | 15 (75) | 0.053 |
Nine patients (45%) in the gabapentin group complained about PLSP, while 15 patients (75%) in the placebo group had complained about PLSB (P = 0.053) (Table 1).
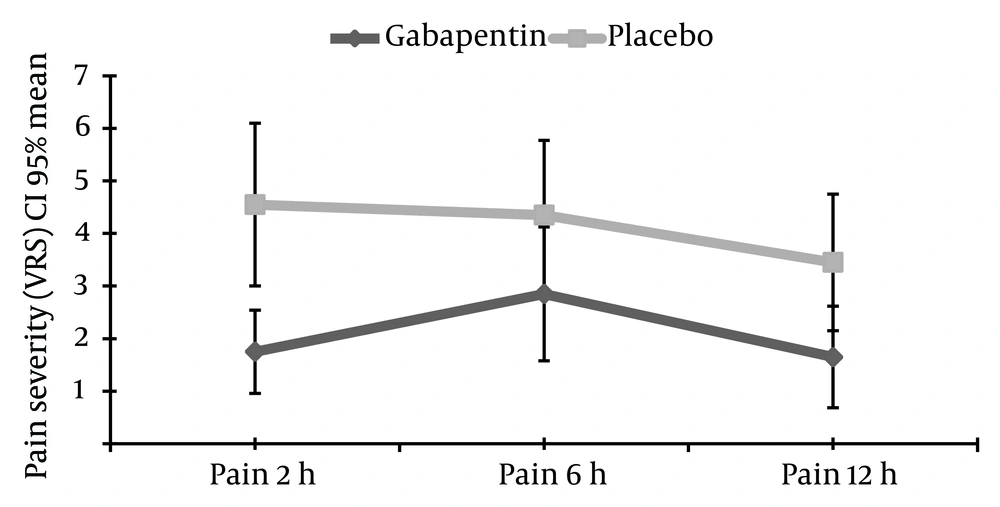
Figure 1 indicates the mean VAS scores at 2nd, 6th and 12th hours after surgery are presented and compared between the two groups. Two hours after surgery, VAS of PLSP was 1.7 ± 1.8 in the gabapentin group while 4.5 ± 3.5 in the placebo group (P = 0.004). Six hours after surgery pain severity was 2.8 ± 2.9 in the gabapentin group and 4.3 ± 3.2 in the placebo group, but the difference was not statistically prominent (P = 0.132). Thereafter, at 12 post-operative hour, the mean VAS scores were 1.6 ± 2.2, and 3.4 ± 2.9 in the gabapentin and placebo groups, respectively (P = 0.036) (Table 2 and Figure 1).
| Gabapentin | Placebo | P Valueb | |
|---|---|---|---|
| Two hours after surgery | 1.7 ± 1.8 | 4.5 ± 3.5 | 0.004 |
| Six hours after surgery | 2.8 ± 2.9 | 4.3 ± 3.2 | 0.132 |
| Twelve hours after surgery | 1.6 ± 2.2 | 3.4 ± 2.9 | 0.036 |
To eliminate the possible confounding effects of age, BMI, pregnancy history, and surgery time the differences were assessed by ANCOVA with repeated measure test. Following the elimination of the possible confounding effects, the severity of PLSP was lower in the gabapentin group compared with that of the placebo group (P = 0.05).
5. Discussion
In recent decades, postsurgical pain was a challenge in postoperative care (1); at the same time the increased favor to minimal invasive techniques added new pain syndromes to classical ones. Post laparoscopic shoulder rapidly became a frequent challenge for physicians engaged in taking care of laparoscopic-gynecologic patients (2, 18). The high frequency of PLSP in the current study as a special group of pelvic laparoscopic patients obviously presents that the PLSP pathophysiology is not related to direct injury by surgical manipulation but it could be a possibility in upper abdomen laparoscopic surgeries.
Laparoscopy pain has a different cause and pathophysiological mechanism compared with laparotomy pain. Major pain syndromes following laparotomy have somatic or parietal origins, while pain syndromes after laparoscopy surgeries are caused by visceral irritation (19).
While traditionally the majority of studies are concentrating on direct surgical pain, referral pains may be an important issue too (20, 21). Current ideas about lesser postoperative pain in laparoscopy compared with laparotomy should be reevaluate to consider mild (VAS = 1 - 3) and moderate (VAS = 4 - 7) forms of pain, especially in remote locations or referral behaviors.
As a 3-alkylated analog of GABA, gabapentin was first introduced as an antiepileptic agent (22). Later, it was found to be effective in reduction of various pain syndromes such as post-herpetic neuralgia, diabetic neuropathy, and sympathetic dystrophy. Considering, central components of pain syndromes, clinical use of gabapentin expanded to more routine situations as a pain killer for postoperative pains (23) compared with Non-Steroidal Anti-Inflammatory Drugs (NSAID’s) (24). The current study was in the favor of using gabapentin for PLSP as a special form of referral pain, too.
Gabapentin could decrease opioid need in a dose dependent manner (25). Gabapentin is especially effective in the first postoperative hours. Sen et al. found effectiveness of 1200 mg gabapentin in one hour after laparotomy hysterectomy to control pain (26). Higher doses of gabapentin were also accompanied with more sedation (27). According to the current study results the necessary dose of gabapentin could be lower and have longer duration of analgesic effect in laparoscopy compared with the ones used in pervious laparotomy focused studies. This could be the result of lower pain intensity in laparoscopy, since the mean reported pains in this study were of low or intermediate intensity. Longer lasting gabapentin is more difficult to discuss. However, along with lower intensity of the pain, the preemptive pains control mechanism, or different mechanism of gabapentin or different etiology of PLSB.
Pregabalin, another GABA analogue with similar pharmacological profile to that of gabapentin was reported to be better than diazepam 5 mg but ineffective to reduce analgesic requirements to control pain after gynecological laparoscopy (28).
Chang et al. reported that pregabalin was not effective to prevent and reduce PLSP after laparoscopic cholecystectomy compared with placebo while over-sedation increased two hours after surgery (29). While gabapentinoids are encouraged to be used in different indications for acute and chronic pain (30), the efficacy of prophylactic pregabalin to prevent shoulder pain after laparoscopic gynecology surgeries in 24 hours after the surgery and reduce co-analgesics was recently approved (31). The difference between the current study results and those of the other studies could be from the differences in the operation and pain entity or severity.
The current study assessed the prophylactic efficacy of 600 mg gabapentin 30 minutes preoperatively on frequency and intensity of PLSP after laparoscopic cystectomy and its effectiveness in the first 12 hours after surgery compared with that of placebo was approved, no significant side effects were observed. Continuation of the analgesic effect 12 hours after surgery may be discussed by possible synergism with the Ibuprofen administered thereafter or a preemptive analgesic effect.
The major limitation for this study was the tunnel vision resulted from strict inclusion and exclusion criteria that helped to perform the study with limited number of cases but at same time limits the popularity of results. The other limitations to this study included the lack of secondary outcomes including changes in co-analgesic use and sedation level. Further studies are recommended to cover PLSP along with other pain syndromes in open studies and have a more widespread insight of the possible postoperative pain shift in recent years.
Prophylactic administration of 600 mg gabapentin is effective to reduce the severity of post-laparoscopic shoulder pain after laparoscopic cystectomy.