1. Background
Suprascapular nerve block (SSNB) is commonly used in pain therapy for patients with chronic shoulder pain (1). The effect of SSNB on shoulder function has, however, been investigated in a single study (2). An increased function plays a pivotal role in the further therapeutic management of shoulder patients. In a recent meta-analysis, it was shown that shoulder function is one of the main predictors for the outcome of physiotherapy (3). If shoulder function, i.e. the range of motion, is increased after application of the nerve block, it can be expected that subsequent physiotherapy, besides being less painful, is also more effective in terms of restoring shoulder mobility.
Since the first description by Wertheim and Rovenstein in 1941, numerous variations have been presented, including techniques with ultrasound guidance, computed tomography or fluoroscopy (4). In this study, we used the approach described by Feigl et al. (5) According to the authors, its main advantage is the simplicity of orientation and the omission of any measurements and markings. The anatomical landmarks are palpable even in obese or muscular patients. They can be approached in supine position and, therefore, be used at the bedside. However, as their study objects were cadavers, only limited conclusions about clinical usability could be drawn (5).
2. Objectives
The aim of our case series was to evaluate the effect of SSNB, using the modified lateral approach of Feigl, on shoulder function in patients with chronic shoulder pain.
3. Patients and Methods
The study was approved by the institutional review board. Patients were recruited at the pain clinic of the Medical University of Graz, Graz, Austria. We included patients with chronic shoulder pain above 3, on a subjective number rating scale (NRS) from 0 ‒ 10, with exhausted non-invasive therapy. Exclusion criteria were neuromuscular diseases and a body mass index < 15 kg/m2 or > 30 kg/m2. After giving written consent, patients were evaluated using the Constant-Murley-Score (CMS), which is the recommended scoring system for shoulder disorders, by the European Society for Surgery of the Shoulder and the Elbow. It incorporates pain, daily activities, motility and strength, ranging from 0 to 100 (6). Likewise, the NRS values (0 ‒ 10) for pain at rest and in motion were documented. Skin around the puncture site was disinfected and the block was performed under sterile conditions.
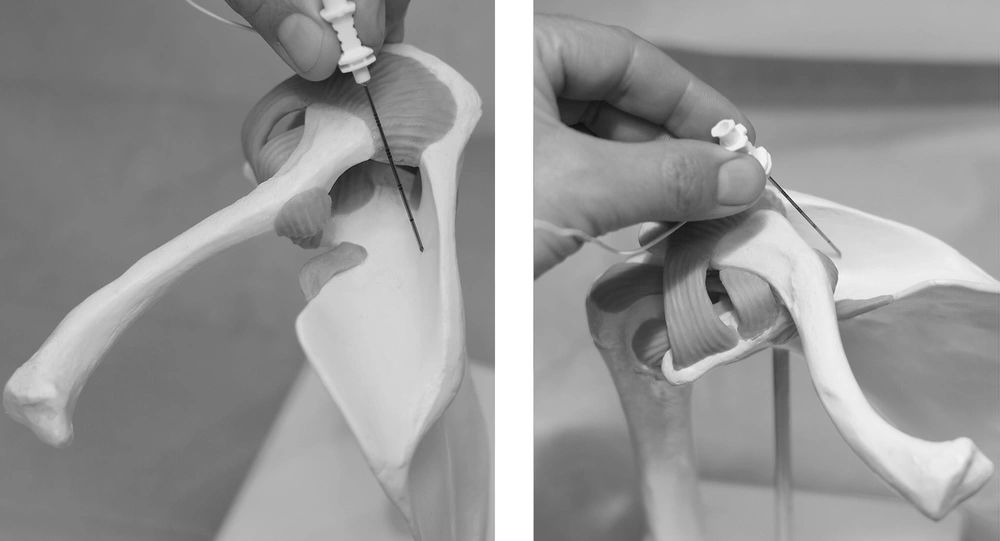
The cannula (Pajunk Uniplex 22G/50mm, Pajunk GmbH, Geisingen, Germany) was inserted, following the method described by Feigl (5). First, the puncturing site was identified as the soft spot surrounded by the following anatomical landmarks: the lateral part of the clavicle and acromioclavicular joint, anteriorly, the acromion, laterally, and the lateral part of the spine of the scapula, posteriorly. The needle was directed dorsomedially, at an angle of 70°, aiming at the spine of the scapula (Figure 1). After establishing bone contact, the needle was retracted approximately 1 mm and 5 mL of ropivacaine 0.5% (AstraZeneca, Vienna, Austria) were injected. The patients were monitored for one hour after the injection. Side-effects and complications, including aspiration of blood or electric sensations, were documented upon occurrence. Time from starting skin disinfection until end of injection was documented. The CMS and NRS were assessed 60 minutes and 24 hours after the block.
Data were tested for normality with the Kolmogorov-Smirnov test and, accordingly, further analyzed using a repeated-measurement analysis of variance. The significance level was established as P ≤ 0.05.
4. Results
As there were no data available for estimating the effect of SSNB on the CMS, at the time the study was planned, a sample size of convenience of 20 was chosen. The inclusion period lasted 18 months.
All 20 patients (11 females / nine males, 51.9 ± 12.9 years old, 168 ± 10 cm height, 75 ± 14 kg body weight) completed the study. The admission diagnoses included impingement syndrome (6x), calcific tendinitis (6x), rotator cuff injuries (6x), and omarthrosis (2x). The mean time for performing the block was 7.4 ± 2.4 min. The CMS and NRS scores decreased significantly, both after 1 and 24 hours (Table 1). No side-effects or complications were observed.
| Parameter | Before SSNB | 60 Minutes After SSNB | 24 Hours After SSNB | P |
|---|---|---|---|---|
| NRS in rest | 2.8 ± 2.1 | 0.9 ± 1.4 | 1.3 ± 1.4 | .0003 |
| NRS in movement | 7.1 ± 1.6 | 3.9 ± 2.3 | 4.9 ± 2.1 | .0023 |
| CMS | 28.8 ± 10.9 | 48.0 ± 17.5 | 47.4 ± 15.0 | .0001 |
aData are presented as mean ± SD.
5. Discussion
Our clinical data demonstrates that SSNB improves shoulder function and pain in patients with chronic shoulder pain. As expected, with a single-shot technique, the effect declines over time. However, both function and pain were still significantly improved after 24 hours, i.e. beyond the pharmacological time of action.
Furthermore, our case series approve the assumption that the modified lateral SSNB of Feigl, which was previously only investigated in cadavers, is a clinically applicable alternative approach to the suprascapular nerve. Various approaches to the suprascapular nerve have been described. The modified lateral SSNB of Feigl is outstanding, as it does not require measurements or markings. Instead, it is purely based on easily identifiable anatomical landmarks. It can therefore be assumed that the time required to perform the block is significantly reduced. Our mean time was 7.4 minutes, including time for disinfection and sterile covers. Unfortunately, literature does not provide data to compare this to other SSNB approaches.
In current literature, the recommended volume of local anesthetic varies a lot. While Wertheim and Rovenstein used 5 ml, later approaches frequently used 10 ml and more (7-10). One author even recommends volumes of up to 25 ml (11). Feigl et al. suggested that filling the suprascapular fossa results in a local spread and surrounding of the nerve (5). Our case series demonstrates the viability of this concept, as all patients experienced significant pain relief, comparable to reports in previous studies Schneider-Kolsky (4 ml): pre-block 7.5, post-block 3.5; Dangoisse (8 ml): pre-block 6, post-block 4; Wassef (10 ml): pre-block 3, post-block 0.5) (12-14).
Chan et al. identified pneumothorax, intravascular injection and local traumatization, as the major risks of the SSNB (4). In our case series, we did not encounter any complication. However, it has to be prone in mind that any conclusions about the safety of this new approach are severely limited by our sample size. However, from an anatomical point of view, both pneumothorax and intravascular injection are very unlikely, using this approach. As the needle is directed dorsally to the scapular spine, accidental intrathoracic placement is obviated. Aiming to the medial half of the suprascapular fossa prevents contact with the suprascapular vessels, which pass through the lateral part of the fossa. The question, whether “blind” approaches are outdate, in times of increased accessibility of imaging modalities, may be raised. However, considering the absence of vulnerable anatomical structures, which was extensively discussed by Feigl, in his original publication (5), this technique should, at least, be regarded as a viable option, in circumstances where imaging is not available.
Our study can be criticized for using a short acting technique, in a chronic pain state, and evaluating the effect for only 24 hours. This can be explained by the focus of our study. Our aim was to evaluate the effect of SSNB on shoulder function, which, taken the lower success rates of catheter techniques, was more meaningful, using a single shot approach. For this research question, a longer observation period was not necessarily required. Furthermore, to our experience, it would not be reasonable to recommend SSNB as a single treatment regime, prior, however, to physiotherapy. In this setting, 24 hours seemed to be reasonable.
Based on our results, further studies should investigate the effectiveness of an interdisciplinary approach, by applying SSNB prior to physiotherapy. As shoulder function is increased and pain is alleviated, we hypothesize that this could be a more effective treatment than physiotherapy alone or with conventional analgesics.
In conclusion, the injection of 5 ml ropivacaine 0.5%, using the modified lateral SSNB of Feigl, did significantly increase shoulder function and reduce pain in patients with chronic shoulder pain.