1. Introduction
Spinal tumours may be classified in three groups: 1) extradural, 2) intradural extramedullary and 3) intramedullary spinal cord tumours. Intradural extramedullary tumours arise from the leptomeninges or nerve roots and include schwannomas. A schwannoma is usually a firm grey-whitish tumour growing near a nerve trunk or ramus. It can be separated from the nerve without damaging neural tissue. Schwannomas are usually solitary tumours (1).
2. Case Presentation
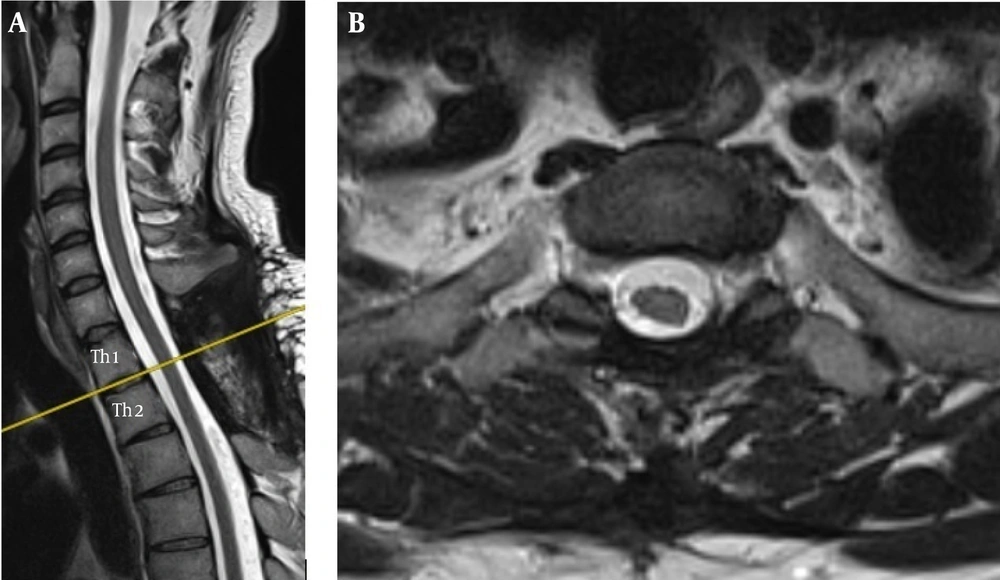
A 37-year-old male patient presented for a neurosurgical consultation complaining of intermittent non-specific pain in the thoracic spine. A neurological examination revealed no neurological deficits. The patient ambulated smoothly and unassisted, there was no weakness of lower limb muscles and no signs of compression of the spinal cord such as spastic paresis, pronounced lower limb reflexes, clonuses at the ankle or patella, extensor plantar response, left-right reflex asymmetry or sensory loss. The back pain had initially prompted the patient to contact his rehabilitation specialist and attend several sessions of rehabilitation and manual therapy. However, as the symptoms persisted, he came for a consultation with a neurosurgeon “just in case”, as he said. The patient reported back pain localized in upper thoracic level of the spine with a slight left-sided laterality of symptoms. Despite the finding of no neurological deficits, the patient was referred for an MRI examination of the thoracic spine. Two weeks later, the patient came back with his MRI report revealing a lesion consistent with a spinal canal tumour at Th1-Th2. The tumour was extramedullary, partly extra- and partly intradural. It was noted that the tumour filled the spinal canal almost entirely, causing critical compression and right displacement of the spinal canal (Figure 1).
Radiologically, the tumour could be classified as a meningioma, neuroma or neurofibroma. The patient was qualified for urgent surgery and referred to the Neurosurgery Department, where the tumour was surgically excised two days later. The tumour was removed by laminectomy of Th1 and Th2. It was located at the level of the Th1/Th2 intervertebral foramen. Following an incision of the dura mater, the tumour mass was exposed which had the gross appearance of a neuroma. The tumour arose from a spinal nerve at the Th1/Th2 level on the left. It was found both intradurally and protruded through the intervertebral foramen outside of the spinal canal, where a part of it could be seen extradurally. In order to completely separate the tumour from the nerve with a view to removing it, the dura mater incision had to be extended towards the point of departure of the spinal nerve and the external sheath of the spinal nerve had to be dissected. A macroscopically radical resection was performed and the tumour was sent for histology. The tumour was accessed by laminectomy and it was not necessary to remove the intervertebral joints. Thus, the spinal column was not destabilised and did not need to be instrumented internally to ensure stability. Following removal of the tumour, dural sac plasty was performed (suturing + additional sealants). No neurological deficits were noted post-operatively. After the surgery, preoperative pain symptoms subsided. The patient was ambulated after another three days and has been able to ambulate smoothly and unassisted. He was discharged home on the 5th postoperative day, with sutures removed on the 8th post-operative day and good healing of the surgical wound. The histological examination revealed a schwannoma (WHO G1) (Figure 2).
A follow-up MRI scan of the spine revealed normal status post surgery with the tumour removed completely (Figure 3).
3. Discussion
Spinal tumours may be classified in three groups: 1) extradural, 2) intradural extramedullary and 3) intramedullary spinal cord tumours. Intradural extramedullary tumours arise from the leptomeninges or nerve roots and include schwannomas. Schwannomas are benign tumours arising from elements of peripheral nerve sheaths. In the skull, they most often originate from the vestibulo-cochlear nerve, less often from the trigeminal nerve. Schwannomas of spinal nerve roots are also quite common. Peripheral schwannomas develop in large and medium-sized nerves, particularly in the limbs and neck. They may also grow subcutaneously in the upper mediastinum and retroperitoneally. Neuromas of parenchymal organs are very rare (2-4).
A spinal canal tumour filling the spinal canal almost entirely and displacing the spinal cord could cause spinal cord damage at any time. The tumour was benign and its complete resection is equivalent to a cure. If the tumour had not been operated on in time, however, the patient would have developed spinal cord damage, paraplegia, loss of the ability to ambulate and would be wheelchair-bound. The case of our patient also illustrates the adaptability of the nervous system. The tumour must have been growing for quite a long time, gradually compressing/displacing the spinal cord, which had adapted to the new situation and was still functionally normal. If a lesion of such dimensions in the spinal canal had developed suddenly, the spinal cord would certainly have been damaged.
The differential diagnosis options, apart from a schwannoma, also included a neurofibroma and a meningioma. Neurofibromas arise from the connective tissue component of the nerve sheaths (perineurium). Unlike schwannomas, neurofibromas grow inside a nerve to overgrow it, thus dissecting the nerve fibres which become trapped amongst the tumour tissue. Unlike schwannomas, neurofibromas have no capsule and grow by infiltration. The removal of a neurofibroma is associated with disruption of the continuity of the nerve the tumour is growing within. Neurofibromas also usually present as multiple tumours, unlike schwannomas (5, 6). The pre-operative MRI appearance could also suggest a meningioma. The vast majority of meningiomas of the spinal canal are found in the thoracic spine (82%), with 15% found in the cervical segment and 2% in the lumbar segment. They are more common in women and are most often diagnosed between the ages of 40 and 70 years. They are most often situated wholly intradurally (90%), with 5% located wholly extradurally, and the remaining 5% of spinal canal meningiomas situated both intra- and extradurally (1). Meningiomas are very rarely diagnosed in patients without neurological deficits. Solero et al. analysed 174 patients undergoing surgery. Only one of those did not present neurological symptoms before the surgery (7).
In our patient, there was a considerable risk of intra-and perioperative damage to the spinal cord. With a tumour of such size causing prolonged compression and displacement of the spinal cord, surgery and the associated sudden decompression of the spinal cord can also induce damage even if the surgery is performed appropriately surgery and the post-operative MRI findings are normal. In our patient, the general and neurological status post-operatively was normal.
The question whether doctors are keen to order more diagnostic investigations (including both laboratory and imaging studies) than are necessary is often asked in clinical practice. The cost factor is also important. Spine tumours are often diagnosed late, sometimes after the occurence of irreversible neurological deficits Not every patient with back pain is referred for an MRI study in the absence of characteristic neurological signs. The case of our patient, however, speaks in favour of early referral for such diagnostic modalities.
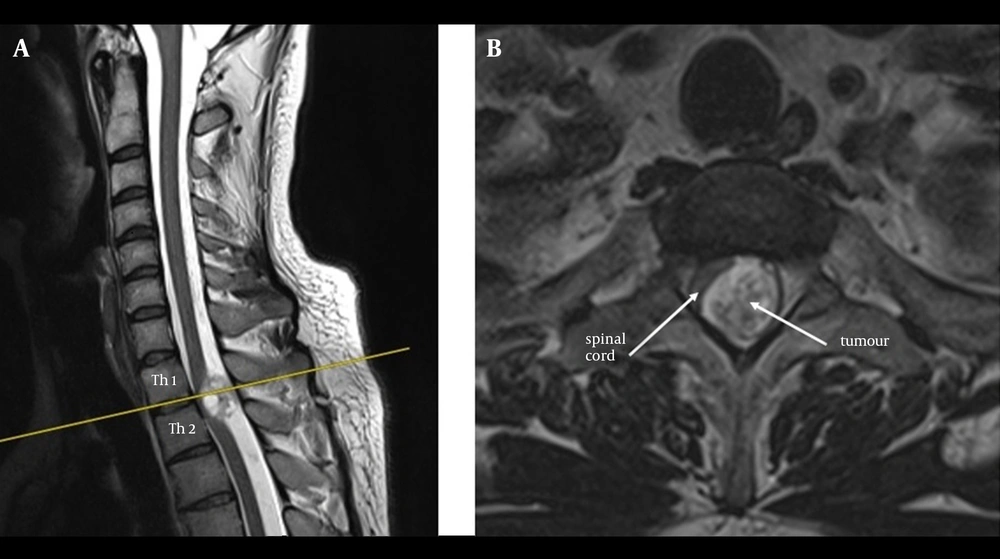
![A histology slide of the resected tumour (schwannoma, WHO G1) showing spindle-shaped cells with band-like nuclei The cells tend to form palisade patterns where the nuclei are seen on the same level in the palisade. This microscopic feature is significant for these tumours (haematoxylin and eosin [H & E], original magnification x40).](https://services.brieflands.com/cdn/serve/3170b/29179f933da7501e8f0ad0b7e7ff9d1288384978/aapm-06-01-33886-g002-preview.webp)