1. Background
Hemodynamic responses to laryngoscopy and tracheal intubation, and their potential hazards, have been well-documented, especially in hypertensive patients. Endotracheal intubation stimulates the laryngeal and tracheal sensory receptors, resulting an increase of sympathetic amines. This sympathetic stimulation results in tachycardia and elevation of blood pressure that may produce an exaggerated hypertensive response, especially in hypertensive patients, and which may lead to cardiac arrest or cerebral stroke (1, 2).
Many drugs have been used to attenuate these adverse responses, including intravenous local anesthetics, opioids, calcium channel blockers, clonidine, gabapentin, and β - adrenergic blockers (esmolol and metoprolol). Combinations of these agents (e.g. lidocaine and esmolol) have been shown to be more effective than either agent alone at attenuating the hemodynamic response, but none of the combinations were very effective (3-12). Lidocaine has a suppressive effect on the circulatory responses in patients undergoing laryngoscopy and tracheal intubation. Clonidine, as a premedicant, has also been used to prevent stress responses to laryngoscopy and intubation (13-20).
There was just one previous study that compared the attenuation of hemodynamic stress responses to laryngoscopy and tracheal intubation between intravenous lidocaine and clonidine (21). In that study, by Routray et al. (21) the efficacy of the intravenous fentanyl-clonidine (FC group) was compared to the fentanyl-lidocaine (FL group) on attenuating the stress responses to laryngoscopy and endotracheal intubation, in 40 patients with controlled hypertension. The authors found no significant differences between the two groups regarding hemodynamic parameters like heart rate and systolic, diastolic, and mean arterial blood pressure, both before intubation and 1, 3, and 5 minutes afterwards. They concluded that both the fentanyl clonidine and fentanyl lidocaine combinations effectively decrease the stress response to endotracheal intubation.
2. Objectives
Since intravenous lidocaine and oral clonidine are financially less demanding and more easily accessible in our practice, we conducted a study to compare lidocaine with oral clonidine on attenuation of hemodynamic responses to laryngoscopy and tracheal intubation, among controlled hypertensive patients undergoing elective surgeries.
3. Patients and Methods
This randomized, double-blinded clinical trial was performed in Dr. Shariati Hospital at Tehran University of Medical Sciences, with the clinical trial registration number of “IRCT2014102819731N1”. The study protocol conformed to the ethical guidelines of the 1989 Declaration of Helsinki, and ethical approval was provided by the Ethical Committee of Tehran University of Medical Sciences, Tehran, Iran.
The participants were eighty-six ASA class II patients, all aged 18 to 65-years-old with controlled hypertension, who were scheduled for elective orthopedic, gynecologic, urologic or general surgeries under general anesthesia. Written informed consent was obtained separately from each patient before surgery. Patients undergoing heart surgery, those who were ASA class III or above, and those who had congestive heart failure (CHF), arrhythmia, BMI ≥ 30, a history of allergies to the study drugs, diabetes, pregnancy, or intubation time greater than 15 seconds were excluded. Patients were randomly allocated into the lidocaine (n = 43) or the clonidine (n = 43) group. Since there were many previous studies which used each of these drugs separately with appropriate effects on reducing hemodynamic responses, we did not include control groups and only compared the two drugs with each other. Randomization was by means of computer generated codes. Sealed envelopes containing the meaning of the randomization codes were kept by hospital staff not involved in the study.
Each patient’s envelope was transferred to a specific member of the staff, who gave a 0.2 mg clonidine tablet (Vazonidin® 0.2 mg Tab, Tolidaru, Tehran, Iran) or a placebo to the patients, depending on the randomization, 90 minutes before surgery. In the operating room lidocaine (Amp 50 mg/5 mL, Lignodic® 1%, Caspian, Rasht, Iran) 1.5 mg/kg and saline were prepared in the same shape of syringes according to the randomization code, by an anesthesia staff member that was not involved in the study. Envelopes containing the information about the randomization were sealed and kept in the patient’s folder until the end of the study period. All members of the surgical team, the nursing staff, the patients, and the anesthetist were unaware of the group allocation.
All patients received their morning dose of anti-hypertensive medication before surgery. After arrival in the operating room, a 20-Gauge IV cannula was inserted for each patient and a 3 ml/kg ringer lactate solution was infused. Standard monitoring equipment including ECG, pulse oximetry, and noninvasive blood pressure was attached to the patients. Patients were questioned about dryness of mouth, and each patient’s baseline heart rate, systolic and diastolic blood pressure, and presence of orthostatic hypotension (more than 20% reduction of mean arterial pressure from baseline after the patient sat up after lying on the operating table) was all recorded.
All the patients were preoxygenated for three minutes. Then, 3 mcg/kg of fentanyl and 1.5 mg/kg of lidocaine, or 1.5 mg/kg of saline, according to the allocation, was injected. Anesthesia was induced by sodium thiopental 5 mg/kg, and intubation was facilitated by atracurium 0.5 mg/kg. The laryngoscopy was performed by one anesthesiologist with a standard Macintosh laryngoscope, and the trachea was intubated with an appropriate size cuffed endotracheal tube in less than 15 seconds. Hemodynamic variables including systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial blood pressure (MAP), and heart rate (HR) were recorded before intubation and 1, 3, 5, and 10 minutes afterwards. Complications such as bradycardia (HR < 60) and hypotension (SBP < 90) were also recorded.
3.1. Statistical Analysis
A sample size of 43 patients in each group was calculated to detect a 10% reduction in MAP with a power of 85% and dropout of 5%. The statistically significant level was P < 0.05. Statistical analysis was performed using the SPSS package (version 19, SPSS, Chicago, IL). Normality of the distribution of data was tested by the Kolmogorov-Simirnov test. Hemodynamic variables between the two groups and within each group were analyzed using the repeated measure test. Demographic data were analyzed by an independent t test or Chi-square when appropriate.
4. Results
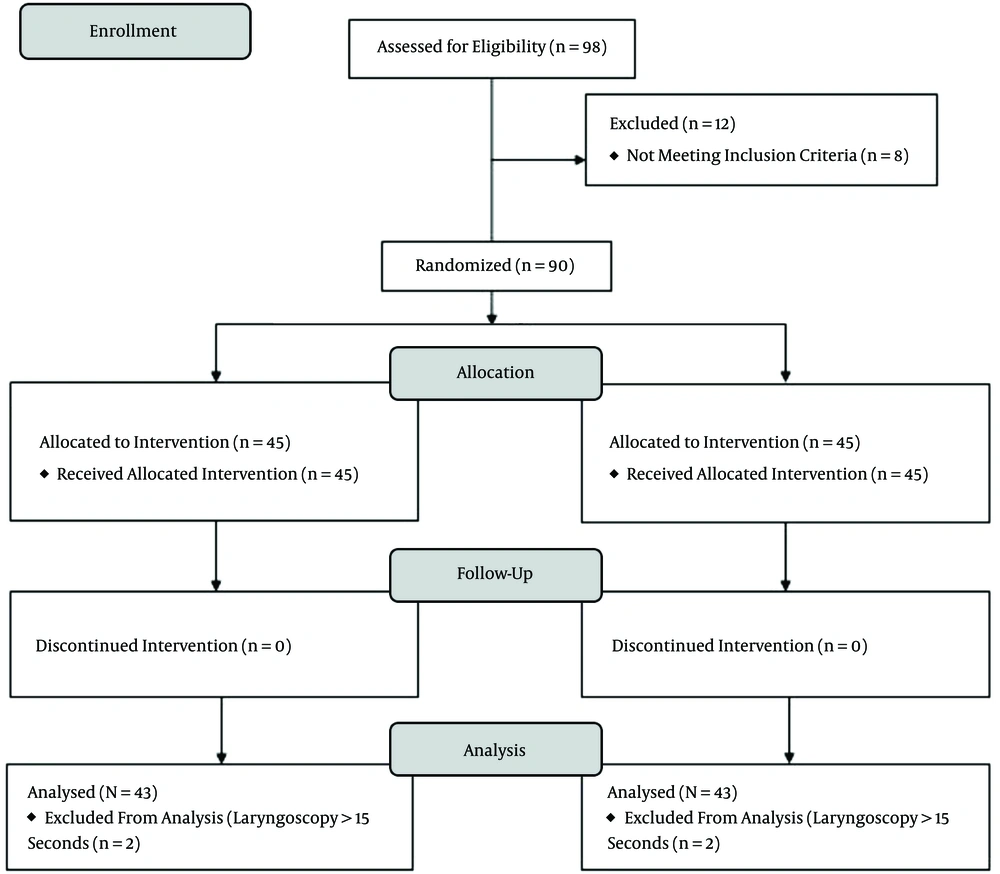
In total, out of ninety-eight patients scheduled consecutively for elective surgeries, eight were excluded due to fulfilling the exclusion criteria and four others for laryngoscopy duration of more than 15 seconds. Finally, 86 patients were allocated for statistical analysis. See the consort flow diagram in Figure 1.
Demographic data were not statistically different between the study groups (Table 1).
There was no significant statistical difference between the two groups of patients regarding HR, SBP, DBP, and MAP before intubation and 1, 3, 5, and 10 minutes after tracheal intubation (Tables 2 - 5).
| Heart Rate, beats/min | Clonidine Group | Lidocaine Group | P value |
|---|---|---|---|
| Before intubation | 90.2 ± 130.1 | 70.2 ± 11.6 | 0.31 |
| 1 minute after intubation | 80.4 ± 15.0 | 77.8 ± 23.4 | 0.54 |
| 3 minutes after intubation | 75.4 ± 13.4 | 76.2 ± 18.3 | 0.82 |
| 5 minutes after intubation | 72.8 ± 12.0 | 74.0 ± 16.2 | 0.70 |
| 10 minutes after intubation | 69.2 ± 16.0 | 72.1 ± 15.4 | 0.39 |
| Systolic Blood Pressure, mmHg | Clonidine Group | Lidocaine Group | P value |
|---|---|---|---|
| Before intubation | 88.9 ± 34.3 | 83.1 ± 36.8 | 0.45 |
| 1 minute after intubation | 114.5 ± 45.6 | 122.5 ± 41.2 | 0.39 |
| 3 minutes after intubation | 85.0 ± 50.0 | 96.4 ± 48.0 | 0.28 |
| 5 minutes after intubation | 85.4 ± 44.1 | 81.8 ± 45.8 | 0.71 |
| 10 minutes after intubation | 88.9 ± 41.0 | 94.4 ± 36.6 | 0.51 |
| Diastolic Blood Pressure, mmHg | Clonidine Group | Lidocaine Group | P value |
|---|---|---|---|
| Before intubation | 67.6 ± 13.1 | 67.6 ± 11.0 | 0.97 |
| 1 minute after intubation | 79.3 ± 19.9 | 86.1 ± 20.0 | 0.12 |
| 3 minutes after intubation | 75.0 ± 14.4 | 77.2 ± 14.6 | 0.49 |
| 5 minutes after intubation | 71.6 ± 14.1 | 73.9 ± 12.1 | 0.41 |
| 10 minutes after intubation | 71.0 ± 15.1 | 71.5 ± 11.7 | 0.85 |
| Mean Arterial Blood Pressure, mmHg | Clonidine Group | Lidocaine Group | P value |
|---|---|---|---|
| Before intubation | 74.7 ± 15.8 | 72.8 ± 14.6 | 0.57 |
| 1 minute after intubation | 91.0 ± 22.9 | 98.2 ± 21.4 | 0.13 |
| 3 minutes after intubation | 76.2 ± 19.6 | 76.5 ± 19.4 | 0.92 |
| 5 minutes after intubation | 76.2 ± 19.6 | 76.5 ± 19.4 | 0.92 |
| 10 minutes after intubation | 77.0 ± 19.0 | 79.1 ± 15.8 | 0.56 |
There were also no significant differences within each group in hemodynamic responses at the measured points (P > 0.05). Twenty patients in the clonidine and three patients in the lidocaine group complained of mouth dryness (P = 0.001). Fourteen patients in the clonidine and four patients in the lidocaine group had bradycardia (P = 0.008). Nineteen patients in the clonidine and six patients in the lidocaine group had orthostatic hypotension before induction of anesthesia, which was corrected by intravenous fluid infusion (P = 0.002).
5. Discussion
The present study showed that both oral clonidine (0.2 mg) and intravenous lidocaine (1.5 mg/kg) were equally effective in decreasing hemodynamic stress responses (HR, SBP, DBP, and MAP) to laryngoscopy and tracheal intubation in controlled hypertensive patients. Endotracheal intubation is a stressful noxious stimulus, resulting in a marked increase in the sympathetic amines (adrenaline and noradrenaline), and leads to complications, especially in patients with cardiovascular diseases. These complications include increases in blood pressure and heart rate that may cause tachyarrhythmia. In normal patients, these responses are generally well-tolerated, whereas in patients with cardiovascular diseases, they may cause cerebral hemorrhage, left ventricular failure, and in rare conditions, myocardial ischemia (1, 2, 22).
Our data confirm and extend the results of other investigators who showed that clonidine and lidocaine separately were effective in blunting reflex tachycardia and hypertensive responses associated with intubation in patients undergoing general anesthesia (3, 4, 13-20). In a study by Hassani et al. (4) on 37 hypertensive patients, fentanyl and fentanyl plus lidocaine decreased the hemodynamic response to tracheal intubation; however, fentanyl plus lidocaine was not more effective than fentanyl alone. Their study had no placebo control group and their findings regarding the effect of lidocaine plus fentanyl correlated to our study, but they did not use clonidine in the other group.
In a study by Sameenakousar et al. (3) the effect of intravenous fentanyl was compared with intravenous clonidine on hemodynamic responses to laryngoscopy and tracheal intubation. They found that clonidine was better than fentanyl for attenuating the hemodynamic responses, and it remained so till the end of 10 minutes. So, they recommended intravenous clonidine 2 μg/kg 5 minutes before the laryngoscopy to attenuate the sympathetic response to the laryngoscopy and the intubation. Their results were different to ours, which may be due to different drug doses and route of drug administration. On the other hand, they did not give fentanyl to the clonidine group. They also did not compare complications between the two groups.
There was just one directly comparable study, by Routray et al. (21) which compared fentanyl-lidocaine with fentanyl-clonidine on hemodynamic responses to tracheal intubation in 40 hypertensive patients. They found no significant differences between the two groups’ hemodynamic parameters, and concluded that both the fentanyl clonidine and fentanyl lidocaine combinations effectively decreased the stress response to endotracheal intubation. Our results correlated positively with the Routray study, but the method of anesthesia and route of drug administration was different, which was due to the form of drug availability in our practice (21).
There are a number of limitations to our assessment. Mainly, we did not include lidocaine or clonidine as a separate group because there were many studies about using each drug separately showing appropriate effects on reducing hemodynamic responses. Although the bioavailability of oral and intravenous routes of drug administration may be different, since we had just oral form of clonidine, we compared two routine and economic drugs available in our practice.
Clonidine and lidocaine were equally effective in decreasing hemodynamic stress responses to laryngoscopy and tracheal intubation in controlled hypertensive patients, although complications including mouth dryness, bradycardia, and orthostatic hypotension were significantly more prevalent in the clonidine group before induction of anesthesia. It seems reasonable to study more groups of patients to compare the effect of premedication by oral clonidine and other oral drugs with lidocaine on hemodynamic variables after tracheal intubation.