1. Background
The placement of a central venous catheter either through the internal jugular or subclavian vein is essential in cardiac surgery (1). The catheter usually has multiple paths through which fluids, blood, or inotropic medication is administered. In addition, the monitoring of central venous pressure as well as pulmonary artery pressure is implemented through central veins (2). One of the critical aspects of cardiovascular assessment is the indirect measurement of central venous pressure (CVP) through the physical examination of blood vessels of the neck, but it is not free from complications. The jugular vein is difficult to palpate in more than 20% of patients, so the measurements of normal, low, or high levels of CVP are inaccurate, especially in critically ill patients. These problems also appear in patients scheduled for surgery; sometimes, even drastic changes of CVP go undetected. As a result, the direct measurement of CVP is frequently required in patients with hemodynamic instability, as well as those undergoing major surgery (3).
On the other hand, the use of central venous cannulation can be associated with side effects, which are both dangerous for patients and can raise costs. Mechanical complications associated with central venous cannulation have been reported in 5% - 9% of patients, infectious complications in 5% - 26%, and thrombotic complications in 2% - 26% of patients. These side effects are associated with several factors, including the anatomy and conditions of patients or the operator’s experience (4). For these reasons, several studies have demonstrated that the use of ultrasound in central venous cannulation can mitigate complications and also reduce the vein access time and related costs (5). In addition, studies have also used ultrasound for pain management following abdominal surgery (6).
2. Objectives
Given the technical difficulties and the risk of serious complications, such as carotid and subclavian artery puncture, pneumothorax, hemothorax, and hematoma in cardiac patients undergoing anticoagulant therapy, this study explored the use of ultrasound technology for the convenient and accurate insertion and reduced complications compared to anatomical landmark-based procedures.
3. Patients and Methods
Initially, 321 patients were randomly assigned to either the control (anatomical landmark-guided) or experimental (ultrasound-guided) groups based upon the order of their entrance to the operating room. Patients who had a right jugular vein cannulation for any reason, such as those who required hemodialysis, were excluded from this study. After obtaining the written informed consent of patients and following the administration of anesthesia and complete monitoring of standards, the procedure was carried out by an anesthesiologist with at least 10 years of relevant work in the field in the landmark-based procedure group and by a sonography specialist who had at least 5 years of relevant experience in the field for the experimental group (ultrasound-guided). Cannulation was implemented using a 7-FR catheter through the right internal jugular vein using the Seldinger approach. The time was calculated by the relevant head nurse using a stopwatch from the moment the needle was inserted until the time of blood aspiration. The number of attempts was recorded in both groups. Moreover, the number of arterial punctures was also recorded, and patients were examined for any sign of swelling or hematoma around the target area or pneumothorax up to 24 hours after the treatment. The preliminary data were recorded in a check list. The data were then input into the Statistical Package for the Social Sciences (SPSS) software, and a descriptive statistical analysis was conducted.
3.1. Cannulation Procedure Using Anatomical Landmarks
Patients were placed in the supine position, and their heads were rotated about 30 degrees to the left. The operator wore sterile gloves, a gown, a cap, and a mask. The skin was disinfected with iodine solution, and sterile drapes were placed on the area. The right internal jugular vein was punctured using a 3.4-inch and 18-gauge needle attached to a 5-cc syringe. Insertion was carried out with the Seldinger approach.
3.2. Ultrasound-Guided Cannulation Technique
The two-dimensional ultrasound linear probe was covered by a 7.5-MHz transducer (Sonosite, USA) using a sterile sheet. The carotid artery and the internal jugular vein were identified by the anatomical features at the site, vein compressibility, vein respiration changes, and pulsation of the carotid artery. All ultrasounds were performed by a single operator. The skin was swabbed with a sterile saline solution, and the probe was placed on the thyroid cartilage under sterile conditions to detect the right internal jugular vein. The location and angle of the needle catheterization was determined by the ultrasound image.
4. Results
In this study, 321 adult patients undergoing cardiac surgery who had been admitted to a general hospital were studied during a 4-month period from the beginning of November until the end of February 2013; 151 of these patients, including 49 females and 102 males, received central venous cannulation using an anatomical landmark-guided technique, while the remaining 170 patients (67 females and 103 males) underwent ultrasound-guided internal venous cannulation. The Chi square test did not show a significant difference between the two groups in terms of gender (P = 0.195)
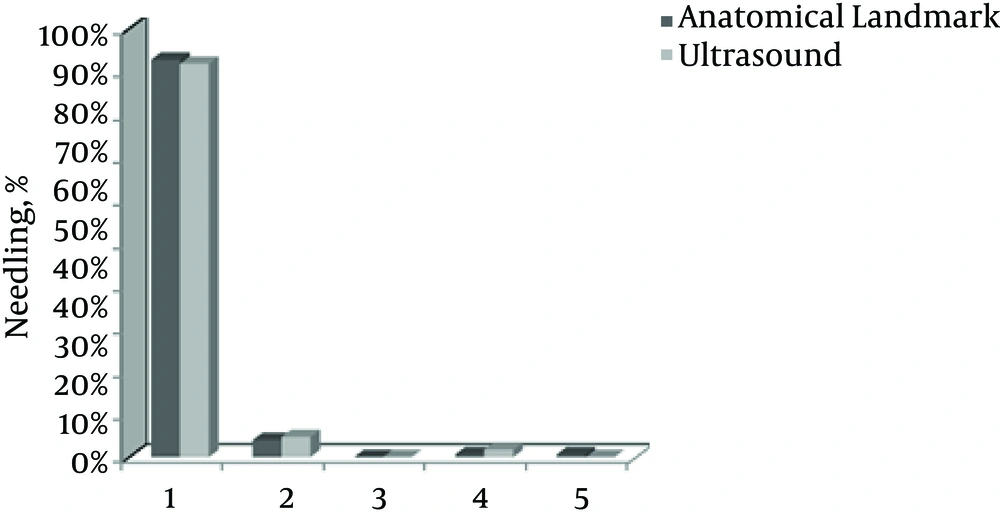
Similarly, the results of an independent t-test did not reveal a significant age difference between the patients in the control group (mean age: 62.15 ± 9.76 years) and the patients in the experimental group (mean age: 64.45 ± 11.29) (P = 0.052). Further, an independent t-test did not demonstrate a significant difference between the two groups in terms of the number of required needlesticks (P = 0.836). As shown in Figure 1, in the anatomical landmark group, catheterization was successful in 92.7% of patients on the first attempt, 4% on the second attempt, and 3.3% in subsequent attempts.
Also, in the ultrasound group, catheterization was successful on the first try in 91.8% of patients, on the second attempt in 4.6%, and on subsequent attempts in 3.6%. The mean number of needlesticks required for the success of the operation was 1.14 in the anatomical landmark group (SD: 0.51) and 1.12 in the ultrasound group (SD: 0.52).
As shown in Table 1, the two groups were compared from different aspects, but no significant difference was observed between the two groups except for the artery puncture (P = 0.04).
| Variable | Positive, % | P Value |
|---|---|---|
| Uncomplicated cannulation | 0.670 | |
| Anatomical landmark cannulation | 6.5 | |
| Ultrasound-guided cannulation | 7.8 | |
| Artery puncture | 0.04 | |
| Anatomical landmark cannulation | 9.9 | |
| Ultrasound-guided cannulation | 4.1 | |
| Emphysema | 0.883 | |
| Anatomical landmark cannulation | 2.0 | |
| Ultrasound-guided cannulation | 1.8 | |
| Pneumothorax | 0.345 | |
| Anatomical landmark cannulation | 0.0 | |
| Ultrasound-guided cannulation | 0.6 | |
| Hematoma | 0.883 | |
| Anatomical landmark cannulation | 2.0 | |
| Ultrasound-guided cannulation | 1.8 |
According to the results, the failure rates of ultrasound-guided cannulation and anatomical landmark-guided cannulation were 0.6% and 1.3, respectively, which were not significantly different (P = 0.494). Further, the reported time required for cannulation was 46.05 ± 12.7 and 45.46 ± 10.9 seconds for the ultrasound-guided and anatomical landmark-guided cannulations, respectively, without any significant difference between the two groups (P = 0.494).
5. Discussion
The results of this study indicated that the two groups were not significantly different in terms of the success rate of catheterization. Our findings were consistent with those of Turker (7) and Ray (2). While Denys et al. reported a success rate of 100% and 88.1% for their ultrasound-guided cannulation group and control group, respectively, in which the two groups were significantly different (8), as shown in other studies (1, 4, 9-11), it seems that this difference may have been due to the fact that limited access to equipment and machinery in Iran has encouraged physicians to use other techniques, such as anatomical landmarks, which explain the insignificant difference between the two techniques.
In this paper, the mean number of needlestick attempts was relatively consistent with the study of Karakitsos (4), although the difference was not statistically significant here but was in Karakitsos’s investigation, which could be due to differences in sample size.
The execution time of the reported procedure in this paper was less than that reported in Turker’s study (7). As for cannulations without complications, Rando’s (12) findings were consistent with this study, in which there were fewer complications in the ultrasound group compared to the anatomical landmark-guided group, though the difference was not significant.
This study showed that the artery puncture made using the anatomical landmark-guided technique was greater than the ultrasound-guided procedure during catheterization, which is in line with the results of Rirapetian (1).
In this study, factors such as obesity, tracheostomy, and thrombosis were exclusion criteria because they made the anatomic landmarks difficult to locate.
5.1. Conclusion
According to the results of this study, under current conditions and due to limited resources and a lack of adequate training, the use of anatomical landmarks will continue to be the preferred method of treatment in Iran.