1. Background
Many factors influence interindividual variations in the spread of epidural local anesthetics, and some of them are controversial (1-13). However, it is difficult to predict the extent of sensory block after the epidural injection of local anesthetics either alone or in combination with opioids (14).
Conventional epidurography of the spine after the epidural injection of contrast material is useful to visualize the catheter tip and to predict the extent of sensory block (13) or to guide interventional pain management (15, 16). In a previous computed tomography (CT) epidurographic study without multiplanar reconstruction (17), focusing on the failures of postoperative analgesia, we reported an abnormal spread of contrast material in a number of patients despite effective postoperative analgesia. However, we did not assess the correlation between the extent of the sensory block and the spread of the contrast medium on CT epidurography. This subject has rarely been studied (13, 18, 19), and all but one of these studies (13) showed that the spread of the contrast medium was not correlated with the extent of the sensory block. However, the statistical analysis of this single study was considered inadequate. The discordant results of these studies may be explained by the difficulty in interpreting radiographs, as the assessment of the distribution of the contrast medium was performed after conventional epidurography of the spine.
Low-dose CT imaging with digital multiplanar reconstruction provides better visualization of the anatomy of the epidural space (19) and more accurate information on the spread of the contrast medium in the epidural space compared to conventional radiography (20).
2. Objectives
The primary objective of this study was to evaluate, by CT imaging and digital multiplanar reconstruction, the spread and distribution of contrast medium injected into the epidural space through a catheter inserted in a low thoracic position for postoperative analgesia, while the secondary objective was to evaluate the relationship between the sensory block and CT spread (of local anesthetics and the contrast medium) in the epidural space after two consecutive injections.
3. Materials and Methods
The study was approved by the local institutional review board (March 2015), and informed consent was obtained for each patient. Inclusion criteria were patients who were scheduled to have thoracic epidural analgesia for major abdominal surgery in a patient-controlled analgesia mode in combination with a continuous infusion of ropivacaine, as is our current practice. Exclusion criteria involved refusal to participate in the study or any contraindications to the placement of an epidural catheter such as anticoagulation or local or general infection, mobilization difficulties, previous spine surgery, iodine allergy, renal impairment, or the failure of epidural analgesia. Patients were included only on postoperative day three before removing the catheter. The baseline ropivacaine infusion, started immediately postoperatively, was stopped one hour before the CT scan.
Patients were placed in the supine position on the examination table with their arms raised above the head. Two injections (5 mL each) were administered at an interval of 15 minutes.
The iodinated solution injected into the epidural catheter had the following composition:
- 4 mL of lidocaine (15 mg/mL)
- 1 mL of Iopamiron (200 mg Iodine/mL) (a nonionic, low-osmolar iodinated contrast medium)
Low-dose CT scans were performed, immediately after each injection, with a GE Lightspeed Multislice (16-slice) scanner. Image acquisition was performed by transverse slices of the cervico-thoraco-lumbar spine with an interslice gap of 0.4 mm. At the end of the examination, images were reconstructed in the three axial, sagittal, and coronal planes. The distribution of the contrast medium was analyzed at the foramina, immediately after each injection, by a radiologist blinded to the level of analgesia results. The spread of the contrast medium was determined by the number of opacified intervertebral spaces.
Fifteen minutes after each injection, the sensory block was assessed by an anesthetist, blinded to the results of the spread of the contrast material in the epidural space, by means of cold and warm discrimination, using ice cubes. For each patient, after each injection of 5 mL of the mixture, the levels of sensory block on the right and left sides were compared to the number of intervertebral spaces opacified on the CT scan.
3.1. Statistical Analysis
Based on the results of previous studies, the extent of the sensory block was expected to be at least three more segments after the second injection of the contrast medium and the local anesthetic. A sample size of 10 patients was considered to be sufficient to demonstrate a statistically significant difference between injections in the spread of the contrast medium material, with a power of 80% and α risk ≤ 0.05.
Quantitative variables are expressed as mean ± standard deviation. The comparison of clinical and CT-determined levels obtained after each injection of 5 mL was performed by the Student's paired t-test (P = .05). The correlation between the two methods (CT scan and clinical examination) was analyzed by Spearman’s test (P = .05). The concordance between the two methods was analyzed by the Bland and Altman method, comparing the relationship of the difference of each value to the mean (21). Clinical sensory block was considered to be the reference method. Mean levels (clinical and CT) were plotted on the x-axis, and the limits of agreements were calculated using the mean differences. The 95% confidence interval was equal to the bias ± 1.96 standard deviations (SD). Agreement was assessed on the clinical significance of the difference between the two methods. A difference of more than two segments was considered to be unacceptable. For the overall analysis, a two-sided P value < 0.05 was considered statistically significant. SAS statistical software version 9.2 (Cary, NC, USA.) was used.
4. Results
Ten patients aged 29 - 71 years were included in the study. Patient characteristics are summarized in Table 1.
| Characteristics | Results |
|---|---|
| Age, y | 53 ± 14 |
| Gender (M/F) | 6/4 |
| Weight, kg | 70.4 ± 18 |
| Height, cm | 168 ± 10 |
| Type of surgery | 1 hepatectomy, 1 gastrectomy, 6 colectomies and 2 posterior pelvectomies |
Demographic Characteristics (n = 10)
The epidural catheter was inserted between T8 and T12 in all patients prior to surgery. The catheter was inserted into the epidural space to a depth of 4 - 5 cm (aimed cephalad) in all patients. Pain scores (assessed by the visual analogic scale) were less than 30 mm at rest and less than 50 mm on effort for all patients.
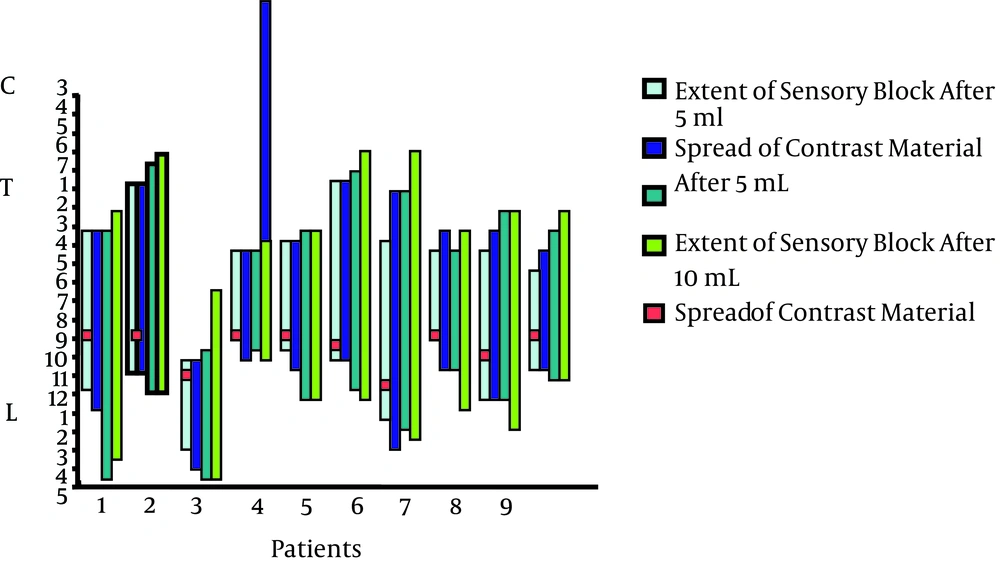
A predominant cephalad spread of contrast medium from the site of injection was observed in all cases but one (Figure 1, patient 3).
The mean levels of sensory block on the right and left sides were calculated for each patient (Figure 1, Table 2). A significant difference in the number of dermatomes of sensory block was observed between injections (P < 0.001), with a marked interindividual variability in the levels for the same volume of injection.
| After 5 mL | After 10 mL | Significance | |
|---|---|---|---|
| Number of sensory blocked dermatomes on the right | 7 ± 3.2 | 10.4 ± 4.3 | < 0.001 |
| Number of sensory blocked dermatomes on the left | 8.8 ± 2.8 | 11.7 ± 2.6 | < 0.001 |
| Number of intervertebral spaces opacified on the right | 8.4 ± 3.3 | 10.8 ± 4.4 | < 0.001 |
| Number of intervertebral spaces opacified on the left | 9.8 ± 3.4 | 13 ± 3.4 | < 0.001 |
Number of Sensory Blocked Dermatomes and Intervertebral Spaces Opacified on the Right and Left Sides After Injection of 5 mL and 10 mL of Solution
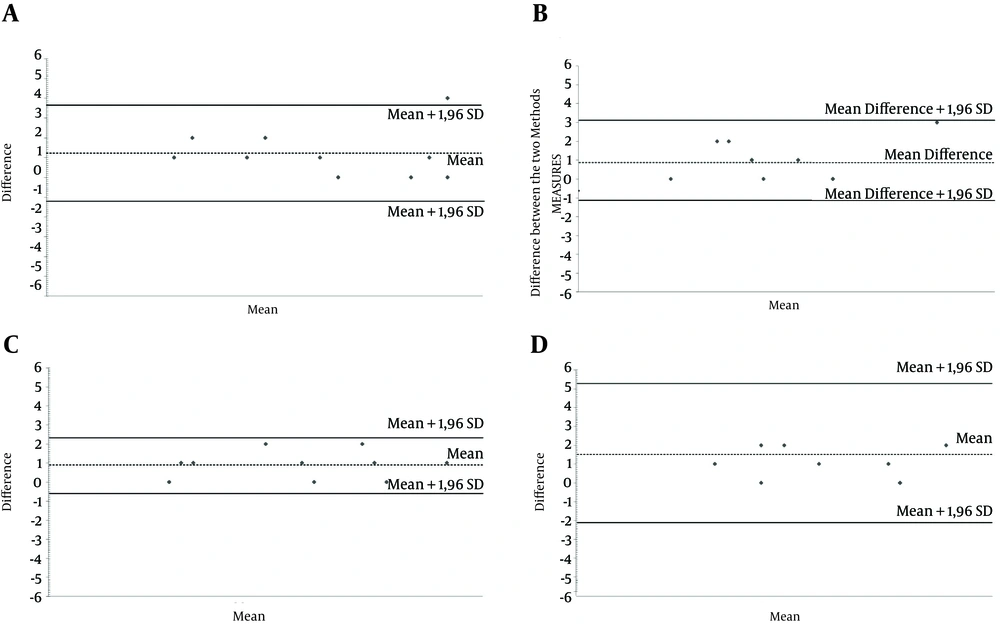
The spread of the contrast medium was correlated with the extent of the sensory block. Contrast material spread more extensively than the sensory block by an average of one dermatome, with a range from T3 to T5 dermatomes. On CT epidurography, there was a significant correlation between the extent of the sensory block and the contrast medium distribution. The results of the correlation analysis are detailed in Table 3, expressed as a straight correlation equation and correlation coefficient (R2). Concordance between the two methods is presented in Figure 2 A, B, C, and D.
| R2 | P Value | |
|---|---|---|
| Right side after 5 mL, y = 0.8919x - 0.4351 | 0.8397 | < 0.05 |
| Left side after 5 mL, y = 0.8222x + 0.6 | 0.9219 | < 0.05 |
| Right side after 10 mL, y = 0.9771x - 0.4575 | 0.9666 | < 0.005 |
| Left side after 10 mL, y = 0.6812x + 2.4891 | 0.6684 | < 0.01 |
Correlation Between CT Epidurography and Clinical Sensory Block
A, Concordance Between the Two Methods on the Right Side After Injection of 5 mL; B, Concordance Between the Two Methods on the Left Side After Injection of 5 mL; C, Concordance Between the Two Methods on the Right Side After Injection of 10 mL; D, Concordance Between the Two Methods on the Left Side After Injection of 10 mL
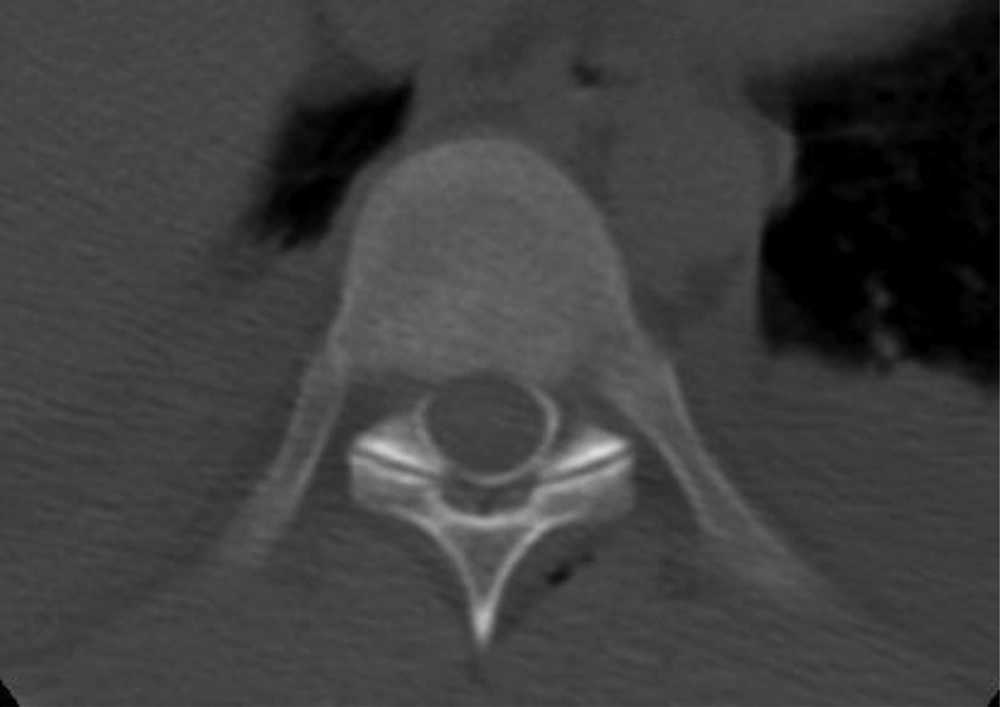
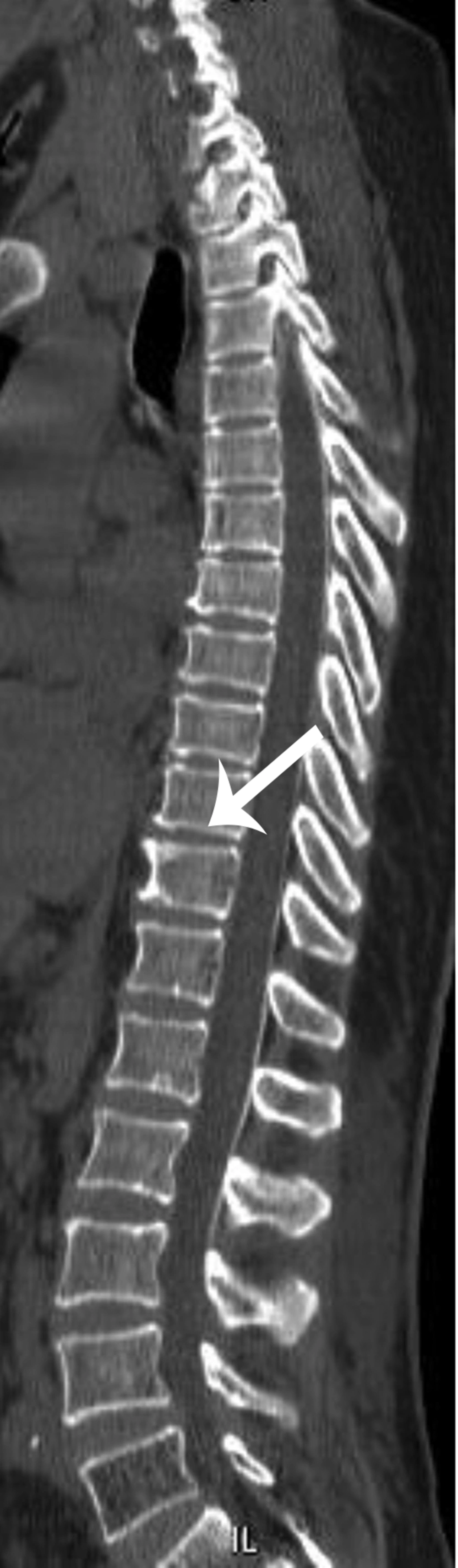
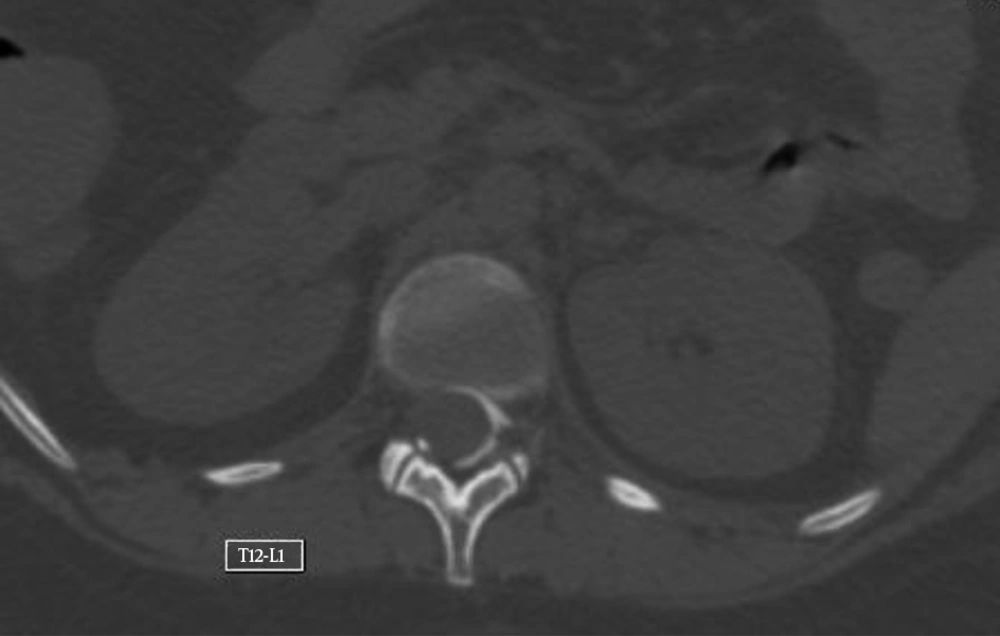
The transverse and sagittal spread of the contrast medium in the epidural space is shown in Figures 3 and 4.
A bilateral double dermatome gap in the clinical sensory block was observed in two patients, corresponding to the same radiological absence of opacification (Figure 5).
Another patient presented left-right asymmetry in the spread of the contrast medium and the level of sensory block (Figure 6).
The spread of the contrast and the extent of the clinical sensory block and level of insertion of the catheter are displayed in Figure 1, after the first and second injection of 5 mL of contrast. A significant difference in the number of dermatomes of sensory block was observed between the first and second injections (P < 0.001).
Contrast material was distributed from T12-L1 to L3-L4 on the right and from T9-T10 to L4-L5 on the left.
An asymmetrical spread of the contrast medium was observed on either side of the catheter insertion site, with marked interindividual variability in the levels of sensory block for the same volume of injection.
5. Discussion
This study shows the asymmetrical spread of contrast medium around the level of insertion of the epidural catheter, detected by CT scan epidurography. The spread of the contrast medium significantly increased after the second injection of 5 mL, but not proportional to the dose. After the second injection, the number of dermatomes of sensory block increased by 32%. However, the spread of the contrast was not uniform at the various levels of the diffusion space. The contrast medium spread more extensively than the sensory block by an average of one dermatome, with a range from 3 to 5 dermatomes. The level of injection into the epidural space is one of the factors determining the distribution and extent of segmental nerve block, as, after thoracic epidural injection, local anesthetics spreads equally in the cephalad and caudal directions (22).
In the present study, the number of opacified intervertebral spaces ranged from 4 to 15 after the first injection of 5 mL and from 5 to 17 after the second injection. Marked interindividual variability and asymmetrical spread of contrast material on either side of the catheter insertion site were observed.
Three routes of spread of the contrast medium (23, 24) along the lines of least resistance within the epidural space have been described: longitudinally in the craniocaudal axis, laterally through the foramina, and circumferentially around the dura. In our patients in whom effective postoperative epidural analgesia was achieved, CT epidurography of the distribution of a mixture of local anesthetic and contrast material showed significant interindividual variability, with the asymmetrical spread of the contrast material/local anesthetics solution in both the transverse and longitudinal planes.
On transverse slices of the spine in the 10 patients studied, the distribution of contrast material in the epidural space was not always uniform. Contrast material was predominantly observed in the posterolateral regions of the epidural space with leakage into the foramina, already demonstrated in several CT studies of the epidural space (25-27), probably because the procedure was performed in a supine position. We have also previously reported that successful postoperative epidural analgesia with local anesthetics and opioids designed to ensure sensory block does not necessarily require the symmetrical spread of the contrast material on CT epidurography (17). Contrast medium spread homogeneously in the longitudinal plane in 8 out of 10 patients. Two patients presented a defect of the contrast material within a homogeneous diffusion space. In another study, histological examination of transverse cryomicrotome slices of the spine (28) also showed heterogeneous spread after the injection of dye into the epidural space, in which the dye travelled along vascular and fatty tissues. An anatomical feature of the epidural space could explain the opacification defects observed in some patients.
The relationship between the injected volume and the spread of contrast material is not linear. In our study, after the second injection, the spread of contrast material increased by an average of only 32%. Under these conditions, it is difficult to predict the longitudinal spread of contrast material and to establish a relationship between the volume of injection and the extent of the sensory block. In contrast to the original description by Bromage (3), Grundy et al. reported that when the volume of local anesthetic injected into the epidural space was doubled from 10 to 20 mL, the extent of the sensory block increased by only three segments (2). These results were confirmed by several other studies (10, 13, 29).
In our study, the levels of sensory block correlated with the spread of the contrast material in the epidural space, but the correlation between the two measuring methods was not clinically acceptable, as in clinical practice, a difference of one or two segments would be acceptable, but CT can overestimate the clinical estimation by up to five segments. Three studies (13, 18, 19) analyzed the correlation between the level of analgesia and the spread of contrast material in the epidural space. These studies distinguished the local anesthetic injection time from the contrast injection time and evaluated the spread of contrast material only by conventional epidurography. In one study (18), volumes of 3 mL and 8 mL were injected into the epidural space, and no correlation was demonstrated between the spread of the contrast material, evaluated by conventional epidurography, and the level of sensory block. However, a more recent study by Yokoyama et al. (13) demonstrated such a correlation, but the Bland and Altman test was not performed to assess the agreement between the two methods of measurement. A post hoc Bland and Altman test performed for this study (13) failed to demonstrate any correlation between the spread of contrast material and the extent of sensory block (30). Our results are therefore in agreement with those of previous studies. However, in contrast with other studies, we used low-dose CT epidurography with three-dimensional digital reconstruction, which could improve the measurement of the spread of the contrast material (25, 31, 32). Nevertheless, our results failed to demonstrate a strong correlation between the sensory block and the spread of contrast material in the epidural space.
The presence of a differential block could explain why the observed level of sensory block is more limited than the spread of contrast material in the epidural space. The presence of a differential sensory block after epidural anesthesia has already been reported (33). The extent of light touch and cold temperature discrimination was greater than that of pinprick analgesia after the injection of 2% lidocaine into the epidural space. Other studies confirmed these findings (34, 35). Epidural anesthesia causes a differential block, depending on the diameter and length of the neurons and the dose of local anesthetics in contact with the neurons (36-41). The volume of local anesthetics at the extremities is likely lower than in the rest of the spreading zone of the solution, and the dose of local anesthetics at the extremities is not sufficient to achieve light touch and temperature analgesia.
5.1. Conclusions
The lack of prediction of the spread of contrast material and the absence of a strong correlation between clinical assessment and CT epidurography with digital reconstruction justifies the assessment of the sensory block for each patient after an epidural injection of local anesthetics. Under these conditions, dose titration is the best way of ensuring acceptable epidural analgesia. As the spread of local anesthetics is not always homogeneous, the combination of opioids with their nonsegmental mechanism of action might be justified in order to improve the quality of the sensory block.