1. Background
Pain is a common side effect of most procedures in the emergency department (ED). Even with minor surgical wounds, there is some degree of local inflammation that stimulates the surrounding nociceptors and causes pain during the healing process (1-6). Postoperative analgesia can help prevent chronic pain and is also essential for better recovery and patient satisfaction. Narcotics are very important in postoperative pain management, but they have some dose-dependent side effects, thus multimodal analgesia is preferred (1, 2, 6-15). Cryotherapy is a relatively noninvasive and cost-effective technique for pain management in cases of trauma or disease (14-27). It has been used in sports medicine to relieve pain caused by soft tissue injuries due to the relatively small number of side effects (7, 16, 19, 21, 22, 24). Cryotherapy can also be used to reduce postoperative pain (13, 18, 20, 25, 26).
2. Objectives
Patients, healthcare teams, and insurers are constantly looking for cost-effective strategies to reduce the use of analgesic medications. We believed it to be prudent to investigate the effect of cryotherapy as an analgesic for minor procedures. We hypothesized that patients receiving cryotherapy before receiving local anesthetic injections in the ED would report lower pain scores, need fewer narcotic medications, and have shorter hospital stays.
3. Methods
3.1. Subjects
The present study was conducted as a randomized, three-center, single-blinded (investigator-blinded) clinical trial. The study was conducted in accordance with the principles of the Declaration of Helsinki. This trial was also registered on the international clinical trials registry platform (registration number: IRCT201307238543N4 at http://www.who.int/ictrp). Patients admitted to our teaching university hospital’s ED from May 2013 to March 2014 were enrolled in the study if they had a simple superficial laceration, which was defined as a laceration involving only the epidermis and dermis. Patients with lacerations extending beyond the dermis were excluded. Patients were also excluded from the study if they had severe injuries and fractures at other sites of the body with intolerable and intense pain, were younger than 10 years of age, or could not cooperate to precisely state their pain score (patients with mental retardation or known psychiatric disorders). Patients who had received any other local or systemic analgesics or sedative drugs were similarly excluded. The study was based entirely on its design, and there was no subject attrition during the follow-up period nor did any of the patients change groups during the course of this study. The researchers obtained informed consent from all the patients before the study began.
3.2. Randomization and Cryotherapy Administration
A random number generator was used to randomly assign the subjects to the two groups. The first group (cryotherapy group) received ice packing prior to the injection and the second (control group) did not. Due to the nature of the procedure (i.e., the application of an ice pack over the wound site), blinding of the patients and staff was impossible. The investigator, who was an attending emergency physician and was not involved in the patients’ care, was blinded to the randomization until the end of the procedure. The researchers used reusable ice bags that were brought to the operating room for the subjects in the cryotherapy group by the study coordinator. We applied a dressing to the wound and then used ice packs over the dressing. The ice pack was held in place for 5 minutes. Thereafter, the procedure (i.e., infiltration of local anesthetic drug and suturing) commenced. In our teaching hospitals, lidocaine (Lidocaine Pasteur 1% 50 mL vial) is available for local anesthesia, and all local infiltrations are done with it. Pain scores were obtained from the patients before and after the procedure using a numeric rating scale. An intention-to-treat analysis was subsequently conducted.
3.3. Outcomes Measures
The primary outcome measure was the pain score before (after completion of 5 minutes cryotherapy) and immediately after the procedure. The patients were instructed to rate their pain intensity on a continuous 10-cm numerical rating scale in which 0 represented no pain and 10 was equated with the worst pain imaginable (28). Secondary outcomes included changes in vital signs and side effects. Vital signs were documented before, during, and after the procedure using patient charts and confirmed with the patient’s nursing team. Side effects were assessed according to the patient’s history and a physical examination.
3.4. Data Analysis
Power calculations indicated a requirement of 31 patients per research arm. In part, this calculation was based on previous publications examining the differences in pain scores that led to a change in pain perception by patients (29-32). A sample of 33 patients per group was required to detect a 15% difference in pain scores between the 2 groups, assuming a 0.05 level of significance and a power of 90%. Descriptive analyses were conducted using demographic, clinical, and surgical variables. Other than sex (expressed as percent male), data were expressed as mean and standard deviation (SD). Comparisons between the randomized groups were achieved using an independent t-test and a Mann–Whitney U test for the parametric and nonparametric data, respectively. A chi-squared test was used in the qualitative analysis. A p value of 0.05 was used as the level of significance. The results were analyzed using the Statistical Package for Social Science for Windows version 19 (SPSS Inc.).
4. Results
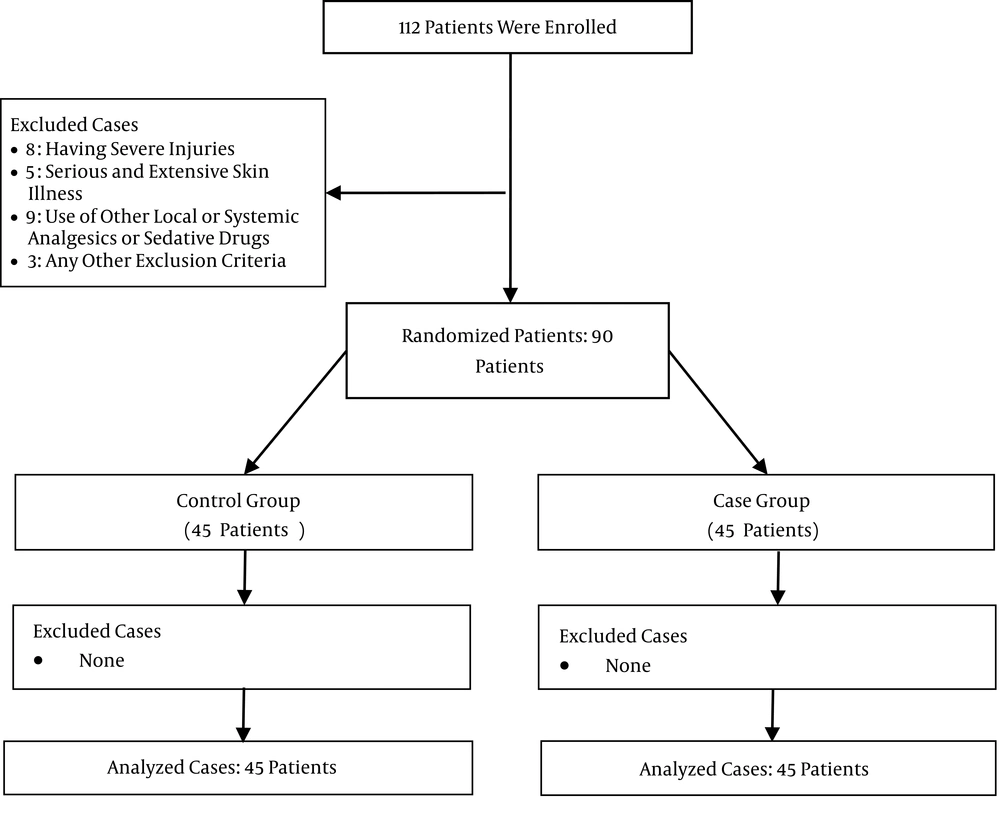
A total of 112 patients were considered suitable candidates to participate in the study. Of them, 22 patients were excluded, and ultimately, 90 patients were enrolled in the study; 45 patients were included in each group (Figure 1). There were no statistical differences in any of the baseline preoperative characteristics (age, sex) between the 2 groups (Table 1).
| Characteristics | Randomization | P value | |
|---|---|---|---|
| Control | Ice | ||
| Age, mean (SD) | 32.24 ± 2.11 | 32.91 ± 2.09 | 0.823 |
| Sex, male (%) | 36 (80) | 33 (73.3) | 0.619 |
The majority of the subjects’ lacerations (32.2%) were on the face, followed in order by lacerations on the forearm and leg. There were no statistical differences between the 2 groups in terms of incision length and the site of the wound (Table 2). There was no intraoperative administration of NSAIDs, acetaminophen, or any narcotic medications in either group.
| Characteristics | Randomization | P Value | |
|---|---|---|---|
| Control | Ice | ||
| Laceration size, cm, mean (SD) | 3.11 ± 0.19 | 3.35 ± 0.22 | 0.410 |
| Wound site | 0.898 | ||
| Face (%) | 20 (44.45) | 21 (46.57) | |
| Forearm (%) | 8 (17.78) | 6 (13.34) | |
| Leg (%) | 3 (6.67) | 3 (6.67) | |
| Other (%) | 14 (31.11) | 15 (33.33) | |
The pain scores were significantly lower in the cryotherapy group before and after the procedure (P < 0.001; Table 3).
| Characteristics | Randomization | P Value | |
|---|---|---|---|
| Control | Ice | ||
| Pain score before procedure, mean (SD) | 3.84 ± 0.26 | 2.27 ± 0.22 | < 0.001 |
| Pain score after procedure, mean (SD) | 5.62 ± 0.30 | 3.62 ± 0.30 | < 0.001 |
Shivering was observed markedly more frequently in the cryotherapy group (P < 0.001), but it was well controlled once the nursing staff had provided blankets. There was no statistically significant difference in wound infection when comparing the 2 groups (P = 0.783; Table 4).
| Characteristics | Randomization | P value | |
|---|---|---|---|
| Control | Ice | ||
| Shivering (%) | 16 (35.55) | 38 (84.44) | < 0.001 |
| Infection (%) | 2 (4.45) | 3 (6.67) | 0.783 |
5. Discussion
Acute pain is a serious issue worldwide and represents a major clinical, social, and economic problem. Under-treatment of pain due to poor medical practice results in many adverse effects (33).
We performed a randomized controlled trial to assess the impact of cryotherapy (ice packs) on pain reduction due to the pinprick from local anesthetic injection as well as complications of wound closure for patients undergoing wound management in EDs. Our results showed that the simple method of placing an ice pack on the laceration site reduces pain during and after the procedure, and cryotherapy could thus be complementary to other pain management strategies because it is easy, affordable, and well received by patients, with minimal to no toxicity.
Cryotherapy has been shown to reduce postoperative pain in studies conducted by surgical subspecialties: otolaryngology, orthopedics, obstetrics, ophthalmology, and plastic surgery (30-43). A Cochrane review of local cooling to reduce perineal trauma sustained during childbirth provides us with some evidence of the safe and effective use of cryotherapy. The review looked at 10 studies, which included 1825 women, that compared the application of multiple cooling therapies such as ice, ice gel packs, cold baths, and cold packs to the affected area (40). One study showed that women had lower pain scores at 24 and 72 hours postpartum when ice packs were used (43).
The mechanism of action of cryotherapy is multifold. It reduces inflammation and swelling, which facilitates cell oxygenation (14, 15, 18, 20, 23, 26). Cryotherapy also slows the cellular metabolic rate, thereby reducing oxygen demand in an environment of reduced oxygen accessibility (14, 15), and limits the production of tissue-damaging free radicals via suppression of exotoxins. Additionally, cryotherapy can prevent neural plasticity and chronic pain by decreasing free nerve ending sensitivity, increasing nerve firing thresholds, and slowing synaptic activity (23, 26, 27). These neural effects increase the patient’s pain threshold and can diminish the need for pharmacologic interventions, such as narcotics or local anesthetics (18, 19, 27). While only a few studies have focused solely on the effect of cryotherapy on abdominal incisions, there is also a paucity of randomized controlled trials. In our study, a change in the pain score was evident during and after the procedure with cryotherapy. Although the absolute numbers were small, the changes were perceptible to the patients. Certainly, it is an inexpensive intervention and particularly ideal in resource-constrained facilities, such as those in developing communities.
In the present study, the analgesic effect of cooling was assessed and found to be associated with less pain. In previous studies, some herbal extracts, such as Juglans regia leaves and the aerial parts of Melissa officinalis, were used successfully in mice as antinociceptives (44, 45) and could be considered for evaluation on real patients in EDs in future studies. Certain studies have also shown that some non-pharmaceutical methods such as listening to a recitation of the Holy Quran prior to a surgical procedure could be useful and effective procedures to decrease anxiety in patients and thus the sensation of pain (46).
5.1. Limitations
There were several limitations to this study. Due to the nature of the procedure (i.e., the application of an ice pack over the wound site), blinding of the patients and staff was not possible, therefore the subjects were only blindly randomized. Gel packs can be used instead of ice packs in future studies to reduce the possibility of leakage from the ice packs, which was a rare occurrence in our study. The positive compression effect, which was not the subject of this study, may also contribute to pain relief and could be an interesting topic for future study. As with all studies, some confounders may not have been considered by the researchers. Finally, a study of the blood level of inflammatory markers in the patients in the cryotherapy group may have proved helpful.
5.2. Conclusion
Ice-pack application is a simple, cost-effective adjuvant to standard procedural pain management. Although it can cause some shivering in patients, it does not lead to significant complications in patients undergoing ED wound management.