1. Background
Endotracheal suctioning is a common method frequently used by nurses in intensive care units (ICUs) to maintain gas exchange, adequate oxygenation, and alveolar ventilation in patients under mechanical ventilation (1). Tracheal tube suctioning is a stressful and uncomfortable procedure and may cause complications such as vagal stimulation, increased respiratory rate, atelectasis, hypoxia, increased intracranial pressure, damage to the lining of the chip area, cardiac dysrhythmia, bleeding, and an increased risk of hospital-acquired infections. These physiological complications can also affect the central nervous system, leading to manifestations such as agitation, pain, hallucinations, aggression, delusions, anxiety, and the severity of the disease (2-5). Thus, one important goal of caring for patients undergoing mechanical ventilation is to prevent the above-mentioned complications by keeping the air passage open and providing the highest amount of gas exchange (6).
The two standard and well-known methods for suctioning lung secretions are the open suction system (OSS) and the closed suction system (CSS). The OSS works by disconnecting the ventilator circuit and inserting a catheter. In CSS, suction is done using a catheter in an enclosed sheath attached to the inside of the trachea without disconnecting the ventilator circuit (7-9).
Different studies have compared the two systems with regard to physiological disorders, oxygenation, and ventilation changes and have succeeded in demonstrating the advantages of one endotracheal suctioning method over the other. Open suction is reportedly associated with inadequate arterial saturation, inability to maintain a positive end expiratory pressure (PEEP), and increased heart rate, blood pressure, and cardiac arrhythmias. Furthermore, OSS exposes the personnel to infectious discharge from patients. It also exposes patients’ artificial air passages to microbial contamination. Furthermore, in some studies, CSS has demonstrated fewer physiological complications than has OSS (7, 10, 11).
Suctioning is accompanied by pain, fear, and sensations of suffocation commonly associated with patients’ loss of breath (3, 12). According to published research, most adult patients in ICUs experience pain and agitation resulting in physical and psychological complications that may last many years after discharge from the hospital (13). These patients’ discomfort is often accompanied by signs and symptoms of agitation in the form of behavioral, physical, and psychological changes (14, 15). Mechanically ventilated patients are unable to express their feelings orally, and these communication difficulties lead to chaotic and disturbing situations for patients hospitalized in ICUs such as desperation and fear of being excluded from treatment decisions (16, 17).
The abundance of noise, light, and other stimuli in ICU environments may also lead to more discomfort and agitation in patients. Agitation is an observable sign that may occur alone or together with severe anxiety, delusions, and impaired brain function (18, 19).
Recent guidelines on the management of pain, agitation, and delirium in adult patients recommend a systemic and rigorous evaluation of pain in critically ill patients, particularly because pain is consistently undertreated in adult patients. The goals of control and management of patients’ pain, agitation, and delirium should constantly be focused on patients’ comfort and safety to mitigate short-term and long-term problems associated with excessive or inadequate treatment (2, 20-22).
Considering the high level of mental-emotional turmoil experienced by mechanically ventilated patients and the importance of such patients’ comfort in achieving the desired treatment outcomes, assessing their psychological status and meeting their mental-emotional needs is of great significance. The nurse, as the person with the most important role in suctioning the patient, should be able to manage the suctioning process so that the patient’s pain and agitation is minimized. Pain and agitation should not be ignored or treated with indifference (2, 15, 23).
2. Objectives
This study was conducted with the aim of comparing the effect of open and closed endotracheal suctioning on mechanically ventilated patients’ levels of pain and agitation.
3. Patients and Methods
3.1. Study Design
The study was a single-blind randomized controlled clinical trial conducted in Iran.
3.2. Samples and Setting
The study was conducted in the general intensive care unit (GICU) of Khatam-ol-Anbia hospital and Sina hospital in Tehran, Iran from, spring 2015 to autumn 2015. The criteria for entering the study included the following: obtaining written informed consent from the patient’s family; over 18 years of age; under mechanical ventilation and requiring endotracheal suctioning; consciousness level with a Glasgow coma score of 7 or higher; vital signs within normal limits; no high-dose sedatives or tranquilizers (deep sedition) during the previous six hours; no severe facial trauma; normal hearing and speaking ability (according to medical records and statements of the patient's family); no neurological damage affecting breathing (such as quadriplegia); no record of mental illness or severe neurological problems; and no neuromuscular diseases.
Exclusion criteria consisted of the following: tracheal extubation; need for repeated suctioning or suctioning at intervals shorter than 20 minutes; reduced level of consciousness during suctioning; dysrhythmia; reduced SpO2 level by more than 10% during suctioning; and need for tranquilizers and painkillers in excess of the common treatment protocol.
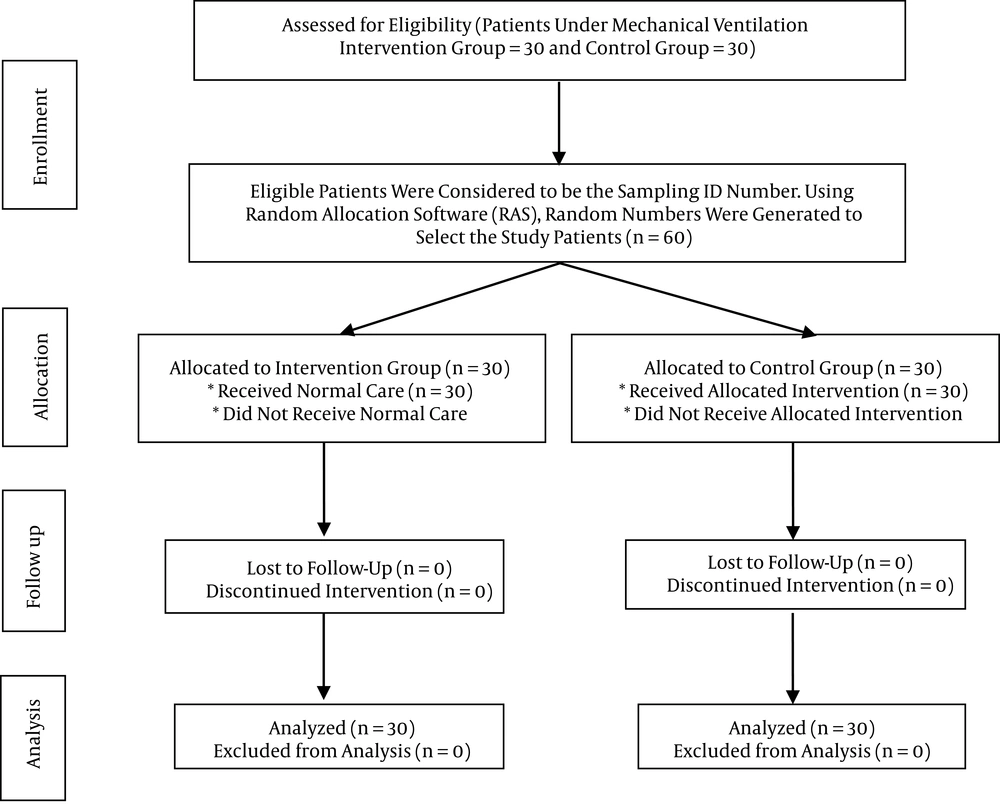
For sampling, we used the random allocation block method. All patients who met the inclusion criteria were recruited. The sample size was calculated using Altman’s nomogram. By considering a confidence interval of 95% and a power of 80%, a sample size of 30 patients was determined for each group.
3.3. Ethical Considerations
The present study was registered on irct.ir with identifying code IRCT201508268650N6 and was registered at the Islamic Azad University ethics committee medical sciences branch of Tehran, Iran (ethical code: IR.IAU.TMU.REC.1394.23). The ethical considerations were related to confidentiality and anonymity during the study period and in publication of the study. The purpose of the study was explained to all patients' families, and informed consent was obtained from the family of each patient who agreed to be included in the study.
3.4. Intervention
Demographic questionnaires were filled out by the researcher based on the patient’s file and statements from the patient’s family. If the criteria necessitating suctioning were present, the suctioning was done for the patient using the standard technique and the sterile method. The sizes of the open and the closed suction catheters were standardized (the suction catheter has an external diameter less than 50% of the size of the endotracheal tube inner diameter). Vital signs were recorded by a monitor. All patients received 100% oxygen for 1 min before suctioning. Immediately after that, endotracheal suctioning by ICU nurses was conducted on a rotating basis for 10 to 15 s with a maximum pressure of 120 mmHg. Following that, the patient was again hyper-oxygenated with 100% oxygen for 1 min, and hemodynamic variables were recorded at five temporal stages (before, during, and immediately after, 5 minutes after, and 15 minutes after the suctioning) for both groups with the monitoring device. The pain and agitation of the two groups were measured using the Richmond agitation sedation scale at the five temporal stages.
3.5. Data Collection
The data collection tool consisted of four parts: the demographic information form, quantitative demographic variables (age and remaining at ICU), qualitative demographic variables (gender, marital status, type of suction, history of intubation), and physiological parameters (heart rate, systolic blood pressure, diastolic blood pressure, mean arterial pressure, and arterial blood oxygen saturation). They were measured using a monitoring device with the trademark “SAADAT”. The devices were assessed and calibrated by servicing companies according to the manufacturers’ manuals.
Patients’ level of pain was recorded and measured using the pain behavior scale designed by Payen et al. (24), which focuses mainly on behavioral indicators of pain (20, 24). The level of agitation was recorded and measured by the Richmond agitation sedation scale designed by Sessler et al. (25) at the five previously mentioned temporal intervals.
3.6. Data Analysis
The data were analyzed using the software SPSS, version 22, and the chi-squared test, t-test, Mann-Whitney test, and analysis of variation (ANOVA) with repeated sizes statistical tests. The P value significance level was set at less than 0.05.
4. Results
In this study, 60 patients under mechanical ventilation were evaluated. According to the results of the independent t-test and chi-squared test, there were no significant differences between the intervention group and the control group in terms of demographic characteristics (Table 1).
Summary Statistics and the Results of the Tests for Comparing Groups for Qualitative Variables
The results demonstrated that the measurement at different temporal stages of the heart rate, systolic blood pressure and diastolic blood pressure variables had a significant difference between the two groups of open suctioning and closed suctioning over time. However, these variables did not show a significant difference between the two groups at all stages, and the pulse rate variable demonstrated a significant difference inside the closed suction group. Also, the time required for heart rate and mean arterial pressure to return to their baseline (initial state) was shorter for CSS. Physiological stability was also better in the CSS group (Table 2).
| Variable | OSS | CSS | P | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before | During the Suction | Immediately After Suctioning | Post-Suctioning 5th Minute | Post-Suctioning 15th Minute | Before | During the Suction | Immediately After Suctioning | Post-Suctioning 5th Minute | Post-Suctioning 15th Minute | ||
| HR (min) | 83.07 (21.00) | 90.00 (19.00) | 93.00 (17.00) | 87.03 (19.04) | 88.00 (18.00) | 80.00 (21.00) | 92.00 (16.00) | 94.00 (17.00) | 85.07 (17.00) | 85.00 (17.00) | P = 0.829; F = 0.047 |
| BP systolic (mmHg) | 133.00 (22.0) | - | 144.07 (27.0) | 134.00 (25.0) | 127.00 (22.0) | 124.00 (20.0) | - | 131.00 (25.00) | 127.00 (19.00) | 123.00 (20.00) | P < 0.630; F = 0.235 |
| BP diastolic (mmHg) | 75.00 (13.0) | - | 81.07 (20.0) | 76.00 (18.0) | 75.03 (17.0) | 72.00 (17.0) | - | 74.00 (18.0) | 71.00 (14.0) | 70.00 (14.0) | P = 0.739; F = 0.112 |
| MAP (mmHg) | 94.00 (15.0) | - | 102.00 (21.0) | 95.00 (19.0) | 92.00 (17.0) | 89.00 (17.0) | - | 93.00 (20.07) | 90.00 (15.0) | 87.00 (15.0) | P = 0.635; F = 0.228 |
| SpO2 (%) | 97.00 (5.0) | 96.00 (3.0) | 96.00 (4.0) | 97.00 (2.0) | 97.00 (3.0) | 98.00 (1.0) | 97.03 (2.0) | 96.00 (3.0) | 97.00 (2.0) | 97.00 (2.0) | P = 0.619; F = 0.250 |
Mean Values of Heart Rate, Arterial Blood Pressure, MAP, and SpO2 in the Patients Who Underwent Endotracheal Suction with the Open and Closed Suction Systems (n = 60)a
Table 3 shows the pain behavior scale in the three areas of facial expression, upper limbs and compatibility with the ventilator for the open and closed suctioning groups. The Mann-Whitney U test did not demonstrate any statistically significant difference between facial expression, upper limbs, and compatibility with the ventilator at the three times after the suctioning in the two groups (P > 0.05). The ANOVA test with repeated measures showed a significant difference inside both groups in the three areas of facial expression, upper limbs, and compatibility with the ventilator (P < 0.001). However, this test did not demonstrate any significant difference between the open and closed suctioning groups in the three areas of facial expression, upper limbs, and compatibility with the ventilator (P > 0.05) (Table 3).
| Item | Measurement Time | Group Opened suctioning | Group Closed Suctioning | Mann -Whitney U Test | ANOVA with Repeated Sizes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Calm | Scowl | Eyes Closed | Grimace | Calm | Scowl | Eyes Closed | Grimace | Group Open | Group Closed | Intergroup | |||
| Facial expression | Before | 25 (83) | 5 (16) | - | - | 26 (86) | 4 (13) | - | - | 0.720 | P < 0.001; F = 104.530 | P < 0.001; F = 78.812 | P = 0.252; F = 1.326 |
| During the suction | - | 18 (60) | 12 (40) | - | - | 14 (46) | 16 (53) | - | 0.305 | ||||
| Immediately after suctioning | 15 (50) | 15 (50) | - | - | 12 (40) | 17 (56) | 1 (3) | - | 0.372 | ||||
| Post-suctioning 5th minute | 29 (96) | 1 (3) | - | - | 28 (93) | 1 (3) | 1 (3) | - | 0.544 | ||||
| Post-suctioning 15th minute | 30 (100) | - | - | - | 28 (93) | 1 (3) | 1 (3) | - | 0.154 | ||||
| Upper limb movements | Description | No moving | Bent limbs | Gathered fingers | Contraction | No moving | Bent limbs | Gathered fingers | Contraction | P < 0.001; F = 37.395 | P < 0.001; F = 54.233 | P = 0.107; F = 2.688 | |
| Before | 15 (50) | 14 (46) | 1 (3) | - | 11 (36) | 18 (60) | 1 (3) | - | 0.328 | ||||
| During the suction | 1 (3) | 18 (60) | 10 (33) | 1 (3) | 1 (3) | 12 (40) | 13 (43) | 4 (13) | 1.000 | ||||
| Immediately after suctioning | 12 (40) | 17 (56) | 1 (3) | - | 8 (26) | 19 (63) | 3 (10) | - | 0.194 | ||||
| Post-suctioning 5th minute | 17 (56) | 13 (43) | - | - | 12 (40) | 17 (56) | 1 (3) | - | 0.168 | ||||
| Post-suctioning 15th minute | 19 (63) | 11 (36) | - | - | 14 (46) | 15 (50) | 1 (3) | - | 0.170 | ||||
| Compatible with ventilator | Description | Tolerate | Cough | Fighting | In-tolerance | Tolerate | Cough | Fighting | In tolerance | P < 0.001; F = 57.225 | P < 0.001; F = 44.157 | P = 0.606; F = 0.268 | |
| Before | 29 (96) | 1 (3) | - | - | 28 (93) | 1 (3) | 1 (3) | - | 0.542 | ||||
| During the suction | 7 (23) | 16 (53) | 7 (23) | - | 7 (23) | 15 (50) | 8 (26) | - | 0.852 | ||||
| Immediately after suctioning | 30 (100) | - | - | - | 100 (30) | - | - | - | 1.000 | ||||
| Post-suctioning 5th minute | 30 (100) | - | - | - | 100 (30) | - | - | - | 1.000 | ||||
| Post-suctioning 15th minute | 30 (100) | - | - | - | 100 (30) | - | - | - | 1.000 | ||||
Behavioral Pain Scale (BPS)a
After comparing the scores obtained using the Richmond agitation sedation scale, it became evident that the mean agitation of patients during suctioning is lower in the intervention group compared to that in the control group. This was not a meaningful finding. Also, after conducting a part-by-part control of different measurement times between the two groups, it became evident that the most agitation occurs during the suctioning, while the patient becomes calm again in the period after the intervention (Table 4).
| Group | Term | Before | During the Suction | Immediately After Suctioning | Post-Suctioning 5th Minute | Post-Suctioning 15th Minute |
|---|---|---|---|---|---|---|
| Group open suctioning | Combative | - | - | - | - | - |
| Very agitated | - | - | - | - | - | |
| Agitated | - | - | - | - | - | |
| Restless | 2 (6) | 12 (40) | 2 (6) | 2 (6) | 2 (6) | |
| Alert and calm | 13 (43) | 3 (10) | 13 (43) | 13 (43) | 13 (43) | |
| Drowsy | 8 (26) | 10 (33) | 8 (26) | 8 (26) | 8 (26) | |
| Light sedation | 3 (10) | 1 (3) | 3 (10) | 3 (10) | 3 (10) | |
| Moderate sedation | 1 (3) | 1 (3) | 1 (3) | 1 (3) | 1 (3) | |
| Deep sedation | 3 (10) | 3 (10) | 3 (10) | 3 (10) | 3 (10) | |
| Unarousable | - | - | - | - | - | |
| Group closed suctioning | Combative | - | - | - | - | - |
| Very agitated | - | 1 (3) | - | - | - | |
| Agitated | - | 2 (6) | 1 (3) | - | - | |
| Restless | 3 (10) | 15 (50) | 6 (20) | 5 (16) | 4 (13) | |
| Alert and calm | 14 (46) | 2 (6) | 10 (33) | 12 (40) | 13 (43) | |
| Drowsy | 8 (26) | 6 (20) | 8 (26) | 8 (26) | 8 (26) | |
| Light sedation | 4 (13) | 4 (13) | 4 (13) | 4 (13) | 4 (13) | |
| Moderate sedation | 1 (3) | - | 1 (3) | 1 (3) | 1 (3) | |
| Deep sedation | - | - | - | - | - | |
| Unarousable | - | - | - | - | - | |
| Mann-Whitney U test | 0.419 | 0.082 | 0.204 | 0.302 | 0.357 | |
| Group open | P < 0.001; F = 19.333 | |||||
| Group closed | P < 0.001; F = 22.255 | |||||
| Intergroup | P < 0.126; F = 2.415 | |||||
Richmond Agitation Sedation Scale (RASS)a
5. Discussion
The findings of this study show that both open and closed endotracheal suctioning lead to an increase in pain and agitation levels in mechanically ventilated patients. Both systems are equal in terms of the severity of pain and agitation. CSS may offer benefits for mechanically ventilated patients based on its innovative characteristics, such as being suctioned by a single nurse (with regard to sterility conditions), reducing the length of the suctioning procedure, reducing the function of the remaining capacity in patients who need end-expiratory positive airway pressure, reducing hemodynamic compromise during suction, reducing leakage of particulate matter, preventing leaking of mucus into space, and reducing the risk of transmission to other patients and nurses. Furthermore, the patient is not detached from the ventilator and ventilation continues during the suctioning. The patient is also calmer and more willing to cooperate (8). CSS has been suggested for use in patients suffering from acute lung injuries or acute respiratory distress syndrome because such patients’ alveoli are more vulnerable (26).
The results reported by Mohammadpour et al. showed no significant difference in the amount pain between the open and closed suction methods (27).
In a study by Acikgoz et al. (28), the pain score obtained in infants with an N-PASS scale during OS was slightly higher compared to that obtained during CS.
Jongerden et al. demonstrated in their study that the mean arterial blood pressure, heart rate, and blood oxygen saturation changed immediately after tracheal suctioning and reached baseline 5 minutes post-suctioning. Changes in heart beat and mean arterial blood pressure were significant after CS and OS, whereas for SpO2, better amounts were observed in the third and fifth minutes after open suctioning (29).
On the other hand, numerous studies report that, reduced costs, and improved care and quality of care. It is well documented that the most important advantage of CSS is the eradication of any weak point due to the detachment of the mechanical ventilation device from the patient. Still, there is little information about the effect of CSS on hemodynamic parameters (30). The results of a study by Evans et al. demonstrated that CS is done more often during the day and that nurses spend less time carrying out CS compared to OS. The CS procedure requires less time and fewer nurses than OS. It also causes fewer physiological complications in patients (7). The results of another study by Corley et al. showed that end-expiratory lung volume improved more slowly with CS compared to OS at all time points. Although CS reduced the lung volume lost during suction, there is less recovery of volume after the suctioning. Thus, the use of CS cannot be advised to protect lung volumes after suctioning (26).
5.1. Conclusion
Overall, according to the findings of this study, changes in the level of pain and agitation were observed over time in the two groups receiving open and closed suctioning, but the type of suctioning system used had no effect on the level of pain and agitation in mechanically ventilated patients. No difference was observed between the two suctioning methods in terms of the level of pain and agitation in the present study. Nonetheless, with regard to studies on the control of these two methods with other clinical variables such as physiological disorders, oxygenation, and ventilation changes, and considering the advantages of CS, the researchers suggest that other studies should be done with larger sample sizes.