1. Background
Endotracheal intubation (ETI) is an excellent example of a complex life-saving intervention performed on critical care patients. Trainees in the field of critical care patient provision (e.g., paramedic students, emergency medicine residents, and anesthesia residents) often acquire ETI skills through repeated exposure thereto, gained in the controlled operating room setting under the guidance of attending anesthesiologists or nurse anesthetists.
Intubation training is one of the most important subjects in the curriculum of anesthesiology residents. There are two methods of teaching in this regard; either at the patient’s bedside in the operating room or through the use of simulation exercises involving a mannequin which allows residents to directly practice on the patient in a safe situation. The second choice is preferred nowadays as patient safety concerns are considered to be of utmost importance. Recently, pre-clinical modes of practical learning have been the focus of many researchers (1). Experience with intubation skills that are exercised in a controlled way enhances residents’ confidence and reduces stress prior to having to work in a real-life situation, such as the operating room (2-4). Simulation-based learning is an increasingly included component in educational strategies. Recently, the use of sophisticated mannequins was introduced in college laboratories for the purposes of teaching intubation skills. In addition, the benefits of using mannequins to teach practical courses is supported in numerous studies (5-7). The objective of the current study was to evaluate the effects of intubation skill training using mannequins in a knowledge, attitudes, and practices study because there is a paucity of relevant studies on this subject in our country and mannequin-based training is underutilized for logistical reasons.
3. Methods
3.1. Study Population
After obtaining approval from the Tehran University of Medical Science Research Ethics Board, our study was registered on the IRCT.IR website using the following number: IRCT2014040917198N1. All novice anesthesiology residents (24) at Sina Hospital, Tehran University of Medical Sciences, Tehran, Iran, were included in the study and invited to participate in the intubating skill training through a small group workshop held at Sina Hospital’s college laboratories. The exclusion criterion for participation in the study was a history of participation by the residents in a previous intubation training program.
The residents were invited to attend five sessions (two theoretical sessions, each of roughly two hours’ duration; and three practical sessions, each lasting approximately four hours), in a 16-hour workshop over four days of training involving the use of an identical procedure on two mannequins. This was an uncontrolled, educational experimental study. The first-year anesthesia residents were not divided into two groups as the intention was to ensure that they would all participate in an educational course that would be beneficial to them.
Personnel from five faculties contributed to the training program, with representation from two of the faculties at each practical session. One of the instructors was assigned to each theoretical session for the small group. Eligible residents enrolled in three small groups for the theoretical sessions and were taught the same theory. Training for intubation and laryngoscopy on mannequins was included in the practical classes. Each session lasted four hours for three consecutive days. Upon termination of the program, residents were allowed to practice intubation on patients in the operating room under the strict supervision of attending anesthesiologists. Residents’ behavior and practical performance was measured as a primary outcome during the intubation attempts in the operating room. Thereafter, they were asked to complete a predefined five-point Likert scale questionnaire on 10 critical items. The inclusion of the 10 items was thoroughly discussed and agreed upon by faculty members in the department of anesthesiology and critical care at Sina hospital and comprised key steps to be taken by residents when performing successful and safe intubation. Each anesthesia resident was individually assessed by a representative from each of the five participating anesthesia faculties. A secondary outcome was to determine residents’ attitudes to the training program in general, in addition to evaluating whether or not an improvement had occurred with regard to their theoretical knowledge between the start and the end of the training program.
3.2. Evaluation Format
The effect of the educational sessions on participants’ knowledge was evaluated using a pre- and post-test. The test comprised 20 multiple-choice questions, included to determine whether or not a novice anesthesiology resident had acquired key knowledge on intubation skills. The same questionnaire was completed by the study participants prior to the start of the workshop and on conclusion of the study.
Residents’ attitudes towards the program were assessed using a self-assessment form containing 10 interpretative questions designed using a five-point Likert scale format (where 1 = strongly agree, 2 = somewhat agree, 3 = neutral or no opinion, 4 = somewhat disagree, and 5 = strongly disagree) completed by the participants on conclusion of the both theoretical and practical training courses.
Details of the questionnaire that was administered to the study participants are included in Table 1.
| The Study Participants Were Asked the Following 10 Questions | |
|---|---|
| 1 | Do you feel that the program covered all you needed to know for intubation? |
| 2 | Do you believe that the program increased your knowledge of intubation? |
| 3 | Do you feel that you can perform intubation independently having completed the program? |
| 4 | Do you feel less anxious than you felt previously? |
| 5 | Do you feel that you are more confident about performing intubation independently having completed the program? |
| 6 | Do you have a positive attitude towards mannequin-based training? |
| 7 | Do you think that the program was scheduled in a logical order? |
| 8 | Do you believe that the theoretical and practical training had a synergistic effect in enhancing your learning? |
| 9 | Would you recommend this educational program to other trainees? |
| 10 | Were you satisfied in general with the overall training course? |
The effect of the educational course on the practical skills of residents was assessed using a questionnaire completed by the faculty personnel. This questionnaire contained 10 interpretative questions designed using a two-point Likert scale format (where 0 = No and 1 is Yes) in which 10 practically oriented items (previously agreed upon by the faculties of the department of anesthesiology and critical care) were considered.
The questionnaire was answered by representative personnel in the five faculties on the performance of each resident after monitoring their intubation attempts in the first week of practice at the patient’s bedside in the operating room.
Details of the questionnaire that was administered to the faculty personnel are included in Table 2.
| 10-Question Self-Assessment Form by Supervising Faculty Personnel | |
|---|---|
| 1 | Did the trainee check the laryngoscope before the commencement of intubation and handle it with his or her left hand? |
| 2 | Did the trainee check the endotracheal tube before intubation? |
| 3 | Did the trainee stand in the correct position (e.g., above the patient’s head)? |
| 4 | Did the trainee insert the endotracheal tube appropriately in the correct side of the patient’s mouth? |
| 5 | Did the trainee take the endotracheal tube in his or her right hand with its curve facing upwards? |
| 6 | Did the trainee complete the intubation process in less than 30 seconds? |
| 7 | Did the trainee take care to avoid hurting the teeth and soft tissue in the patient’s mouth? |
| 8 | Did the trainee check the correct insertion of the endotracheal tube following intubation using appropriate means? |
| 9 | Did the trainee seem to be less anxious than a typical novice anesthesiology resident? |
| 10 | As a representative of your faculty, were you satisfied with the overall performance of this novice anesthesiology resident? |
All of the faculties were informed of the study objectives, the content of the questionnaires, and the method of evaluation before commencement of the study in order to minimize errors in the survey process and to standardize the approach of the instructors to the assessment procedure.
3.3. Statistical Analysis
Statistical analysis was conducted using SPSS® version 17. Pre- and post-workshop scores were compared between groups using the Wilcoxon signed-rank test. A P-value of < 0.050 was considered to be statistically significant. The multiple choice question scores of the participants were recorded before and after the training program. The paired t-test was used to compare the results.
4. Results
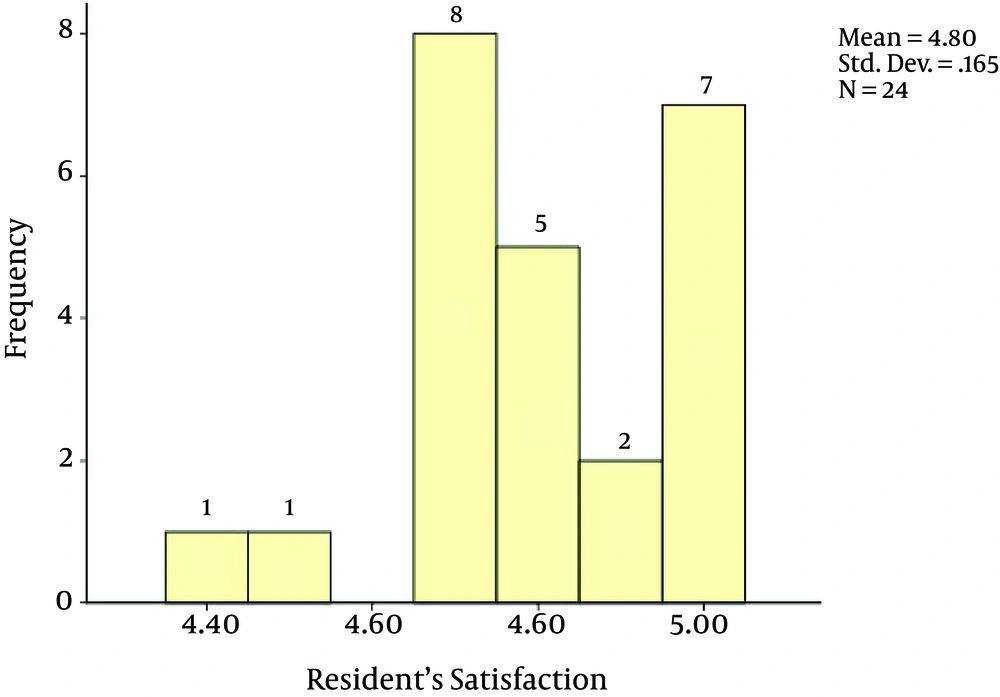
All of the 24 study participants completed the survey (100%). The satisfaction of the study participants with the mannequin-based training course is depicted in Table 3. The mean score of the respondents regarding their attitudes towards the training course was 4.8 out of 5.0 (96%), with a relatively low corresponding standard deviation of 0.16.
| Statistics | Values |
|---|---|
| N | 24.00 |
| Mean | 4.80 |
| Median | 4.80 |
| Standard deviation | 0.17 |
| Minimum | 4.40 |
| Maximum | 5.00 |
The mean score following faculty assessment of the residents’ practical skills was 4.6 out of 5.0 (92%), with a relatively low corresponding standard deviation of 0.13 (Table 4). The multiple choice questionnaire scores of the study participants were compared before and after the workshop and the results were statistically significant (P = 0.001) (Table 5).
| Statistics | Values |
|---|---|
| N | 24.00 |
| Mean | 4.64 |
| Median | 4.61 |
| Standard deviation | 0.14 |
| Minimum | 4.44 |
| Maximum | 4.88 |
| Scores | Mean | Standard Deviation | P-Value |
|---|---|---|---|
| Pre | 9.08 | 3.00 | 0.001 |
| Post | 17.08 | 0.06 |
An score of 4.7 out of 5.0 for attitudes was recorded for most of the residents (33%). Twenty-nine per cent (n = 7) of the residents were completely satisfied with the training course (Figure 1).
5. Discussion
This study was rare in that it focused on the impact of mannequin-based learning on novice anesthesiology residents. The main finding of this study was that simulated training was an appealing educational modality, the use of which allowed residents to practice intubation directly on a mannequin patient and acquire technical expertise in a safe way.
Lucisano et al. conducted a systematic review of four main medical databases (Medline, PshycInfo, Web of Science, and CINAHL) and identified 34 articles on simulation-based training in the field of airway management. Of these, only six studies were conducted on anesthesia providers (8). In addition, it was found that the beneficial impact of simulation-based learning on medical students has been reported elsewhere (9-12).
By contrast, Borges et al. reported that simulation-based programs may not benefit the practical performance of trainees and adherence to the American Society of Anesthesiologists difficult airway algorithm in real-life situations (13). Somewhat surprisingly, it was suggested in the study by Finan et al. that novice pediatric anesthesiology residents, who underwent a two-hour course on mannequin-based intubation training, were not as qualified as those who did not when facing real-life intubation challenges in newborn infants (14).
The results of the current study indicate that training using mannequins was an acceptable means through which novice anesthesiology residents could acquire intubation skills. The cause of the discrepancy between our study findings and those of Finan et al. could be that a mannequin used to simulate a newborn infant may not be as lifelike as a mannequin that is made to resemble an adult. In addition, the study by Finan et al. was performed in a critical care setting whereby patients are not usually anesthetized and paralyzed when intubated. In particular, intensive care unit infants are known to struggle vigorously when attempts are made to still them for intubation purposes. Thus, high-fidelity simulation of a struggling newborn infant is likely to be greatly diminished, if not impossible.
Issenberg et al. reported that the allocation of a small group to each session allowed residents adequate time for practice further and to obtain feedback from the attending anesthesiologists (15). The positive attitudes of residents in our study, who had been placed into small groups, supports Issenberg’s findings.
Some researchers claim that ongoing training throughout the residency, rather than the delivery of workshop education as a one-time intervention, is particularly important in ensuring procedural skill retention (16, 17). In the current study, having received inspiration from the previously mentioned studies and with that objective in mind, we enhanced memory retention by designing three simulation-based training sessions over three consecutive days. Thus, a decrease in sensory motor memory was avoided and memory retention enhanced in the anesthesiology residents through the repetition of a number of given skills. A significant delay between each experience was also eliminated as the training sessions were held over three consecutive days. Regardless, it is understood that the acquisition of intubation skills is a gradual process, and assimilated by residents via repeated practise on human subjects following their residency.
Crabtree et al. considered a correlation between the simulated performance of fiberoptic intubation and clinical skills but did not find a significant one because their single outcome measure was time to completion. They explained that the inclusion of this outcome affected the ability to detect an improvement in performance (18).
Simulation was perceived as enjoyable by students in another pilot study. Although there was a greater improvement in the results pertaining to the multiple choice questions post teaching in the simulator group by comparison with that in the lecture group, the baseline scores were higher for the latter (19).
Medical teaching methods are also changing. Currently, students are encouraged to become self-learners, receive less didactic instruction, utilize peer group interactions more frequently, and increasingly use portable self-accessible technology (20). We designed a practical questionnaire based on objective measures to enhance the value of our evaluation of trainees in order to accommodate these issues.
5.1. Limitations
We might be criticized for not asking the patients on whom our anesthesiology residents practiced intubation about their assessment of whether or not it had been performed well. We assessed the impact of our training course on the residents (healthcare providers). Our intention was not to evaluate the effects of our intervention on patient outcomes (healthcare receivers). Furthermore, intubation is a critically important skill and should be performed under the meticulous supervision of an expert clinician. It would not be ethical to allow residents to make mistakes for learning purposes as this would result in patient harm.
It might be construed that a limitation of our study was that we did not evaluate the potential for a decrease in skills acquired over time, thought to occur following initial training and practice. However, this is not indicated at all in anesthesia residents as they are required to repeatedly practice intubation on patients throughout their residency. However, a decrease in skills might be applicable to non-anesthesiology medical staff who participate in a simulation-based program but then lose their skills over time due to lack of practice.
A control group of residents was not included in this study. This might have decreased its value with regard to the ability to make a statistical comparison, but it is noteworthy that we included 10 objective measures (as opposed to subjective ones) from various faculties in order to evaluate intubation in patients by the residents. In addition, we thought that it would be unethical to deprive certain novice anesthesiology residents of the opportunity to practice intubation on mannequins before operating on patients. Lastly, while blinding participants to the study objectives is an acknowledged study strength, it was not possible in this case.
5.2. Conclusion
Teaching intubation skills using mannequins to first-year anesthesiology residents through small group workshops led to a significant improvement in their level of knowledge and high levels of faculty satisfaction. However, it is recommended that further studies are conducted in which a control group of residents is included to confirm these results.