1. Background
Acute renal failure based on its definition, sudden worsening of kidney function and reduced glomerular filtration (1, 2), is a common complication of important diseases, major surgeries, and sepsis (3). Acute kidney injury (AKI) is a well-known and prevalent side effect, especially after cardiac surgery, which varies from asymptomatic rises in biochemical markers up to dialysis necessity (4-11).
In cardiac surgery, acute kidney injury may be caused by several mechanisms. During cardiac surgery, especially in cases of cardiovascular instability, usually the mean arterial pressure is less than 80 mmHg. Also, many of these patients have impaired system of kidney self-regulation to keep the glomerular filtration until the mean arterial pressure less than 80 mm Hg is reached, which is due to associated conditions such as aging, atherosclerosis, hypertension, and chronic renal failure, impaired renal function using nephrotoxic drugs, or proinflammatory conditions. Another reason is the initiation of systemic inflammatory response syndrome (SIRS). In fact, proinflammatory conditions such as damage caused by surgery, blood contact with artificial surfaces during cardiopulmonary bypass (CPB), and endotoxemia play a key role in AKI development via inflammation. It seems that SIRS resulting from cardiac surgery works in the same way (4).
Adenosine release as a vascular vasodilator increases after cardiac surgery, which reduces renal and glomerular blood flow, and subsequently causes kidney ischemic damage (12).
Cleveland model is the most common model to predict the probability of AKI after cardiac surgery. AKI risk factors are as follow: female gender (1 point), congestive heart failure (2 points), left ventricular dysfunction(1 point), intra-aortic balloon pump before surgery (2 points), chronic obstructive pulmonary disease (COPD) (1 point), insulin-dependent diabetes(1 point), a history of previous cardiac surgery(1 point), emergent cardiac surgery (2 points), and heart valve surgery with/without CABG (3 points), other cardiac surgery (2 points), preoperative creatinine (Cr) between 1.2 to 2.1 (2 points), and preoperative Cr greater than 2.1 (5 points); the sum of these points show the Cleveland score (Cleveland clinic foundation acute renal failure scoring system) (1, 13).
According to Cleveland model, each of the invoices takes certain points, which ranges between 0 and 17 as a whole. All the patients were categorized based on 3 groups of low with a value of 0 to 2, intermediate with 3 to 5, and high with a value of 6 or larger (14). Accordingly, individuals, who had a higher score, were at a higher risk of AKI. Age, primary disease of the kidney, renal artery disease, hypertension, and atherosclerosis have been identified in other studies as risk factors (1, 3, 13, 15).
RIFLE criteria (risk (increased Cr × 1.5 or GFR decreases > 25%, or UO < 0.5 mL/kg/hr × 6 hrs), injury (increased Cr × 2 or GFR decreases > 50%, or UO < 0.5 mL/kg/hr × 12 hrs), failure (increased Cr × 3 or GFR decreases >75%, or Cr ≥ 4 mg/dL, with acute rise of ≥ 0.5 mg/dL, or UO < 0.3 mL/kg/hr × 24 hrs, or anuria × 12 hrs), loss of kidney function (persistent ARF = complete loss of renal function > 4 weeks), and end-stage renal disease (ESRD)) are used to evaluate the postoperative kidney injury (1, 4, 14, 16).
Treatment with aminophylline, as an antagonist of nonspecific adenosine receptor, increases renal filtration and urine flow and reduces the dialysis necessity (12). Gaffney et al. found that AKI could not significantly be reduced after cardiac surgery (6). In another study, aminophylline showed no effect to prevent acute kidney injury in children recovering from cardiac surgery performed with cardiopulmonary bypass (17). The association between perioperative use of aminophylline infusion and lower incidence of deterioration in renal function following cardiac surgery in high-risk patients has been suggested by Mahaldar et al. (14).
The present study aimed at evaluating the impact of aminophylline on renal function after cardiac surgery hoping to find an appropriate method to reduce AKI.
2. Methods
This was a double- blind randomized controlled trial that evaluated the effect of aminophylline on renal function after cardiac surgery. This study conformed to the ethical guidelines of the 2000 Declaration of Helsinki as reflected in a priori approval by the Iranian Registry of Clinical Trials (IRCT No.: 2015010619470N10),. The sample size was calculated as 144 patients based on the obtained results of similar studies with the P1= 0.14, P2 = 0.015, α = 5%, and the power of 80%. Those patients without arrhythmia, tachycardia, nonoliguric kidney injury, anuria, obstructive uropathy, and congenital anomalies were candidates for cardiac surgery.
After receiving approval from the ethics committee of Shiraz University of Medical Sciences, we obtained informed consent from all 144 patients (95 male and 50 female patients). The primary end points were described as glomerular filtration rate (GFR) and Cr and its relationship with the Cleveland score. Secondary end points were the development of severe acute kidney injury, time between intensive care unit (ICU) admission and first successful extubation, CPB time, blood transfusion volume, urine output(UO), ICU and post intensive care unit (PICU), and length of hospital stay.
In the preoperative examination, the Cleveland score was measured and the patients were categorized based on 3 groups: low, intermediate, and high.
Random numbers were produced from http://www.randomizer.org/ by simple randomization technique, and 2 customized collections of random numbers were generated, which were called 1 and 2. Based on these 2 sets, the patients were assigned into 2 groups of 72 patients.
Routine care was performed for all patients before and after cardiac surgery. The intervention group received 5 mg/kg aminophylline (Sina Daroo, Tehran, Iran) bolus before surgery and after anesthesia induction; then, 0.25 mg/kg/hr of the drug was administered intraoperatively and up to 48 hours after surgery in the ICU cardiac surgery. Similar volume of normal saline was injected to the second group. Serum BUN and Cr, as a marker of kidney function, were measured pre- and postoperatively and for 3 days after the surgery. GFR was measured using the formula of Cockcroft and Gault according to age and serum Cr (CG GFR = (140 - age) × Weight / 72 × Cr); this formula was multiplied by 0.85 for females (14). Patients’ 24- hour UO was calculated up to 2 days after surgery. RIFLE criteria were calculated as well.
Anesthesia was induced by midazolam 0.1 - 0.2 mg/kg, sufentanil 0.7 - 1 mcg/kg, sodium thiopental 1 - 2 mg/kg, and pancuronium 0.2 mg/kg. Anesthesia was maintained using regular inhaled anesthetic agents (eg, isoflurane) during the surgery. All the recruited patients were operated on by one specified surgeon; and the type of inotropic drugs, amount and type of fluids, and blood products used by the surgeon during the operation, aortic cross clamping (ACC), and CPB time were recorded.
In the postoperative ICU, aminophylline was prepared for the infusion by an anesthesia technician for 2 days and placed on infusion pump; and the in charge nurses in the ICU were not aware which patients were receiving the drug or saline. In case of aminophylline medical complications, the ICU supervisor was notified and the drug injection was stopped according to the cardiologist opinion.
The data collected from the study groups were analyzed by SPSS 16 software (SPSS Inc., Chicago, IL). Normality analysis was done by Kolmogorov- Smirnov test normality; the obtained quantitative data were analyzed using Mann- Whitney U test; and the qualitative data analysis was performed by chi- square and t test.
3. Results
The mean age of the patients in this study was 61.31 ± 11.40 years. No significant differences were detected between the 2 groups in the demographic data of the patients including age, weight, height, and CPB time (P* > 0.05). Based on the Cleveland score, as a risk predictor of AKI after cardiac surgery, patients in each group were divided into 2 groups: patients with a score less than 6, and patients with a score greater than 6. Accordingly, among 62 patients in the intervention group (86.1%) and 63 control participants (87.5%), with a score less than 6 based on the statistical analysis, the difference was not quite significant (P* = 0.806). similarly, no statistically significant difference was detected between the 2 groups (13.9% of the patients were in the intervention group and 12.5% in the control group) for the score of more than 6 (P* = 0.805). Moreover, during the operation, 48 patients in the intervention group and 52 in the control group required blood transfusion, and even though fewer individuals in the intervention group received blood transfusion, the difference was not statistically significant. Thus, blood transfusion could not evaluate other outcomes as a confounding factor. Nevertheless, the patients who received medication were extubated earlier than those in the control group, with a significant difference (P* = 0.018).
Postoperation characteristics such as UO were not significantly different between the 2 groups, but the length of ICU and PICU stay were significantly lower in the treatment group (P* = 0.001).
During the operation, 51 patients in the intervention group and 65 in the control group have required inotropic medication. Fewer people in the intervention group received inotropic drugs and there was a significant difference between the 2 groups (P* < 0001) (Error! Reference source not found.).
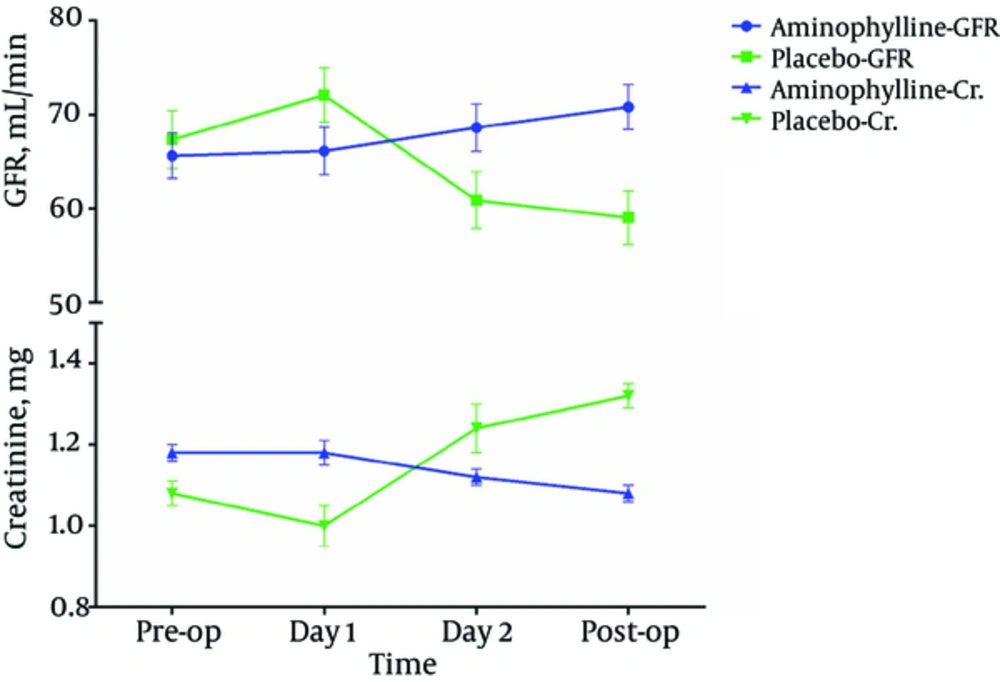
GFR and Cr. values fluctuation in the treatment group was smaller than the placebo group although the differences were not significant in all the follow-up days except for postoperation GFR in the placebo group, which was significantly lower than the preoperation amount (P* < 0.01) (Error! Reference source not found.).
In both groups, there was a GFR reduction and Cr elevation as a result of the increasing duration of CPB and ACC, and the strength was improved by the length of CPB. In other words, the relationship between reduced GFR and increased Cr with increasing duration of CPB was weakly significant (P* = 0.056 and P* = 0.055, respectively), but this relationship was not significant based on the ACC time (P* = 0.28 and P* = 0.18, respectively).
According to the RIFLE criteria, only 3 patients experienced the GFR reduction of more than 25% (risk level) in the treatment group, 1 patient experienced 50% reduction (injury level), and most patients experienced no change or even improved GFR; these amounts were significantly lower than that of the placebo group (P* < 0.05). Accordingly, Cr enhancement in the treatment group occurred only in 2 patients up to 1.5-fold (risk level) and 2 patients up to 2-fold (injury level); and again, the Cr amounts did not change or even decreased in most of the patients; these values were significantly lower than that of the placebo group (P* < 0.05). None of the patients in this study were located in the failure, loss, and ESRD groups. Based on GFR data, the frequency of AKI in aminophylline group was 5% and it was 29.11% in the control group (Error! Reference source not found.).
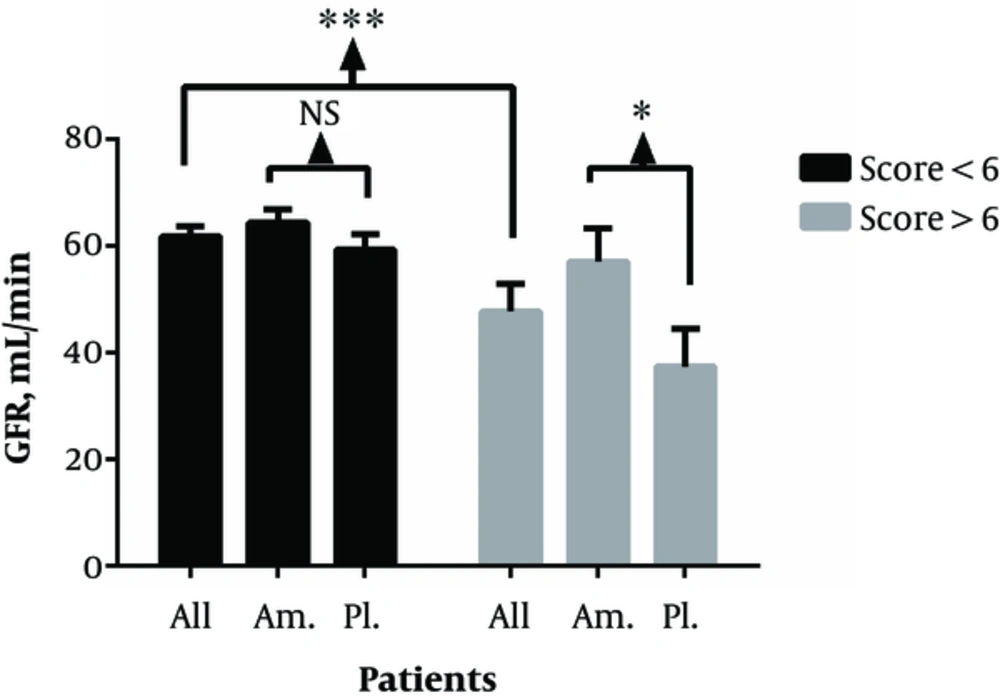
GFR value of all the patients with Cleveland score of less and more than 6 was 61.77 ± 21.97 and 47.73 ± 22.25, respectively, indicating a significant difference between the 2 groups (P* = 0.001). This amount was 64.35 ± 20.08 in aminophylline group by Cleveland score less than 6, indicating no significant difference compared to the placebo group with the GFR values of 59.23 ± 23.56 (P* = 0.139), but GFR value of aminophylline group was 57.06 ± 19.58 with Cleveland score greater than 6, indicating a significant increase compared to that of the placebo group by value of 37.37 ± 21.29 (P* = 0.43) (Error! Reference source not found.).
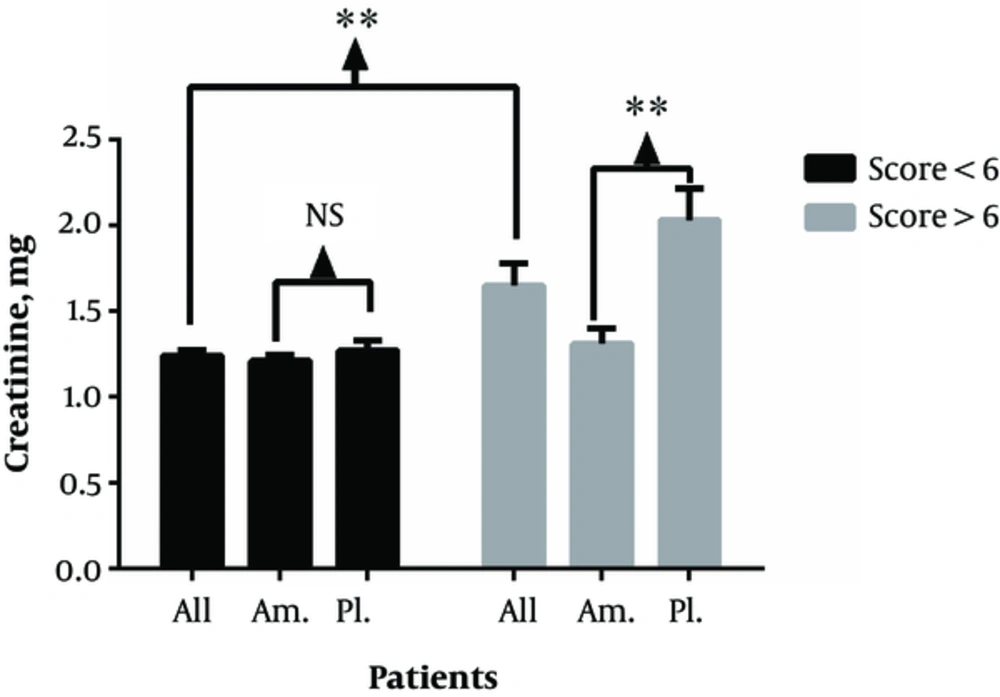
Similarly, Cr values of all the patients with Cleveland score less than 6 was 1.24 ± 0.37, which was significantly lower than that of the group with Cleveland score greater than 6 with the value of 1.65 ± 0.56 (P* = 0.01). Furthermore, comparison between the groups that received aminophylline (1.21 ± 0.27) and placebo (1.27 ± 0.45) showed no significant difference in the amount of Cr in the placebo group when the Cleveland score was less than 6 (P* = 0.91). However, these amounts were significantly different in the treatment group (1.31 ± 0.28) and placebo group (2.03 ± 0.55) with the Cleveland score greater than 6 (P* = 0.002) (Error! Reference source not found.).
In this study, 3 patients experienced tachycardia, and according to the cardiologist opinion, the treatment drug was stopped for 1 to 2 hours and started again. Only 1 patient from the control group died 4 days after surgery.
| Variables | Aminophylline | Placebo | P Value |
|---|---|---|---|
| Age, y | 61.3 ± 10.09 | 65.6 ± 10.10 | 0.128 |
| Weight, Kg | 66.9 ± 10.4 | 65.5 ± 11.7 | 0.460 |
| Height, cm | 164.7 ± 8.21 | 160.8 ± 8.92 | 0.400 |
| Cleveland Score | 3.9 ± 1.2 | 3.9 ± 1.3 | 0.20 |
| CPB time, min | 83.97 ±38.98 | 71.94 ± 21.97 | 0.072 |
| Blood transfusion volume, Bag | 1.47 ± 0.61 | 1.76 ± 0.87 | 0.125 |
| Extubation time, hour | 12.65 ± 10.7 | 17.11 ± 11.8 | 0.018 |
| First day urine output, cc/kg/hr | 1.45 ± 0.39 | 1.46 ± 0.46 | 0.098 |
| Second day urine output, cc/kg/hr | 1.38 ±0.39 | 1.31 ± 0.45 | 0.209 |
| ICU stay length, day | 2.08 ± 0.36 | 2.63 ± 1.15 | 0.001 |
| PICU stay length, day | 4.34 ± 0.67 | 4.87 ± 1.23 | 0.001 |
aData are presented as mean ± SD.
| Group | Epinephrine | Norepinephrine | Dopamine | Total |
|---|---|---|---|---|
| Aminophylline | 36 | 8 | 7 | 51 |
| Placebo | 63 | 1 | 1 | 65 |
| Total | 99 | 9 | 8 | 116 |
| Variables | Group | Total | No Risk | Risk | Injury | Failure | Loss | ESRD |
|---|---|---|---|---|---|---|---|---|
| GFR | Aminophylline | 72 | 68 | 3 | 1 | 0 | 0 | 0 |
| Placebo | 72 | 51 | 18 | 3 | 0 | 0 | 0 | |
| Cr | Aminophylline | 72 | 69 | 2 | 1 | 0 | 0 | 0 |
| Placebo | 72 | 53 | 14 | 3 | 0 | 0 | 0 |
4. Discussion
Considering the mechanism of acute kidney injury after cardiac surgery and the risk factors, this study was designed in 2014 - 2015 to evaluate the effect of aminophylline to prevent kidney damage. Based on regression analysis, it appears that aminophylline, independent of other confounding factors such as CPB and ACC time, preoperation GFR, and Cr, could reduce postoperative kidney injury according to GFR and Cr criteria.
Our results revealed that in the group that received aminophylline, fewer patients needed the inotropic drug, which could be as a result of positive inotropic effect of aminophylline (3). The extubation time was shorter in the treatment group, which was due to the fact that many factors (e.g., anesthetic drugs) could be involved at the time of extubation of the trachea. Thus, this result may not be outstanding for the effect of aminophylline. Similarly, Axelrod et al. found no significant difference between first successful extubation in the patients who received aminophylline and placebo in preventing acute kidney injury (17).
Rising CPB and ACC time led to increased serum creatinine and reduced GFR in all the patients. It seemed that aminophylline independent of other confounding factors such as CPB and ACC time, preoperation GFR, and creatinine could influence GFR and Cr; this finding is consistent with other studies demonstrating that prolonged time of CPB and cross-clamp affected serum Cr levels and GFR as useful parameters for postoperative renal injury (18, 19).
Similar to other studies that used aminophylline or theophylline as adenosine receptor antagonist, we found significant differences between the groups according to RIFLE criteria in assessing the extent of postoperative kidney damage compared with the preoperative (20). As the prominent role of adenosine and its receptors on kidney function and inflammatory processes has been recognized, the potential preventive effect of aminophylline on AKI may be related to its regulatory effects on adenosine receptors (21).
In our study, the patients with the Cleveland score less than 6 showed no significant difference in the GFR and Cr values compared to the placebo group although the placebo group had worse postoperative renal situation in GFR and creatinine compared to the treatment group. However, comparing the amount of GFR and Cr in patients with Cleveland score more than 6 in the 2 groups, we found that the average amounts of GFR and Cr were significantly better in the treatment group compared to the control group. The higher amount of preoperative Cleveland score had a noteworthy impact on the postoperative kidney injury in the intervention group, which could be improved by aminophylline. In contrast to the study by Kramer et al. that found no effect of theophylline on preventing AKI in cardiac surgery patients, it was found that aminophylline infusion in high-risk patients with Cleveland score higher than 6 could lead to a better GFR and Crvalues after surgery (22). These results are consistent with the study of Mahaldar et al., which indicated that intravenous aminophylline could be used in the prevention of AKI as a safe and efficient modality among the high‑risk patients after cardiac surgery (14).
In our study, aminophylline did not result in improved UO in the intervention group, but the length of stay in the ICU and PICU was lower, which could reduce the health care costs.
In the present study, we did not have access to any drugs as a standard treatment of AKI to compare the results with positive controls. We assessed the response of a single dose of aminophylline without a dose-response titration on the prevention of AKI in patients undergoing cardiac surgery; and finally, a longer follow-up could help gain more consistent results. For the future investigations, other existing pathways responsible for AKI and the therapeutic properties of other agents with similar effects as adenosine receptor antagonists could help find a standard remedy for prophylaxis of AKI. Thus, further studies are warranted in this area.
4.1. Conclusion
As a result, it appears that the use of aminophylline before, during, and after heart surgery can reduce the incidence of acute kidney injury. Also, use of this drug may reduce the need for inotropic medication at the time of surgery. The effect of aminophylline on extubation time may not be obvious in patients due to the impact of other factors. However, our study revealed that patients were extubated faster and their length of stay in the intensive care unit was lower compared to the control group. More importantly, aminophylline could reduce the incidence of AKI according to RIFLE criteria and could be used in the prevention of AKI as a safe and efficient modality for the high‑risk patients after cardiac surgery.