1. Introduction
Right ventricular perforation by an endocardial lead is not common, but it is considered a potentially life threatening complication of pacemaker implantation (1). Because the right ventricular (RV) wall is thinner than the left, perforations to the RV is not surprising. Myocardial perforation may occur due to improper force on the leads against the RV free wall during implantation. “However, intraoperative RV perforation due to pacing catheter after its successful and uneventful insertion is a rare complication.” (2). Here, we report a case of cardiac arrest due to RV perforation associated with a permanent pacemaker lead during off-pump coronary artery bypass graft (OPCAB) surgery that was treated successfully with emergency on-pump coronary artery bypass graft (ONCAB) surgery.
2. Case Presentation
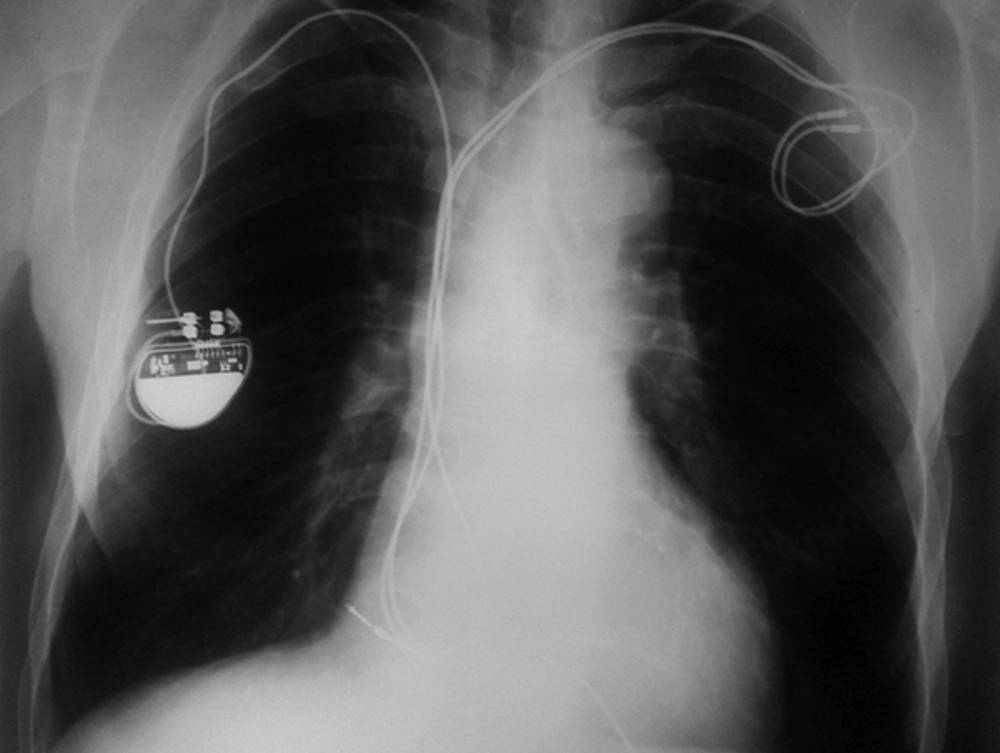
A 68-year-old male was admitted to the emergency room with retrosternal chest pain. A year ago, he underwent implantation of a dual chamber permanent pacemaker due to symptomatic complete atrioventricular block. Because he experienced pacemaker failure 2 months earlier, a single chamber permanent pacemaker was implanted in the right ventricle for him through right subclavian vein. Chest x-ray findings indicated a dual chamber leads through left subclavian vein and a single chamber permanent pacemaker lead through right subclavian vein in the right ventricle (Figure 1). The angiography report revealed that the patient had a patent left main artery (LMA) and a 3- vessel disease involving the left anterior descending (LAD), second obtuse marginal (OM), and right coronary arteries (RCA). Therefore, the patient was a candidate for elective OPCAB surgery after reprogramming the pacemaker to VOO mode.
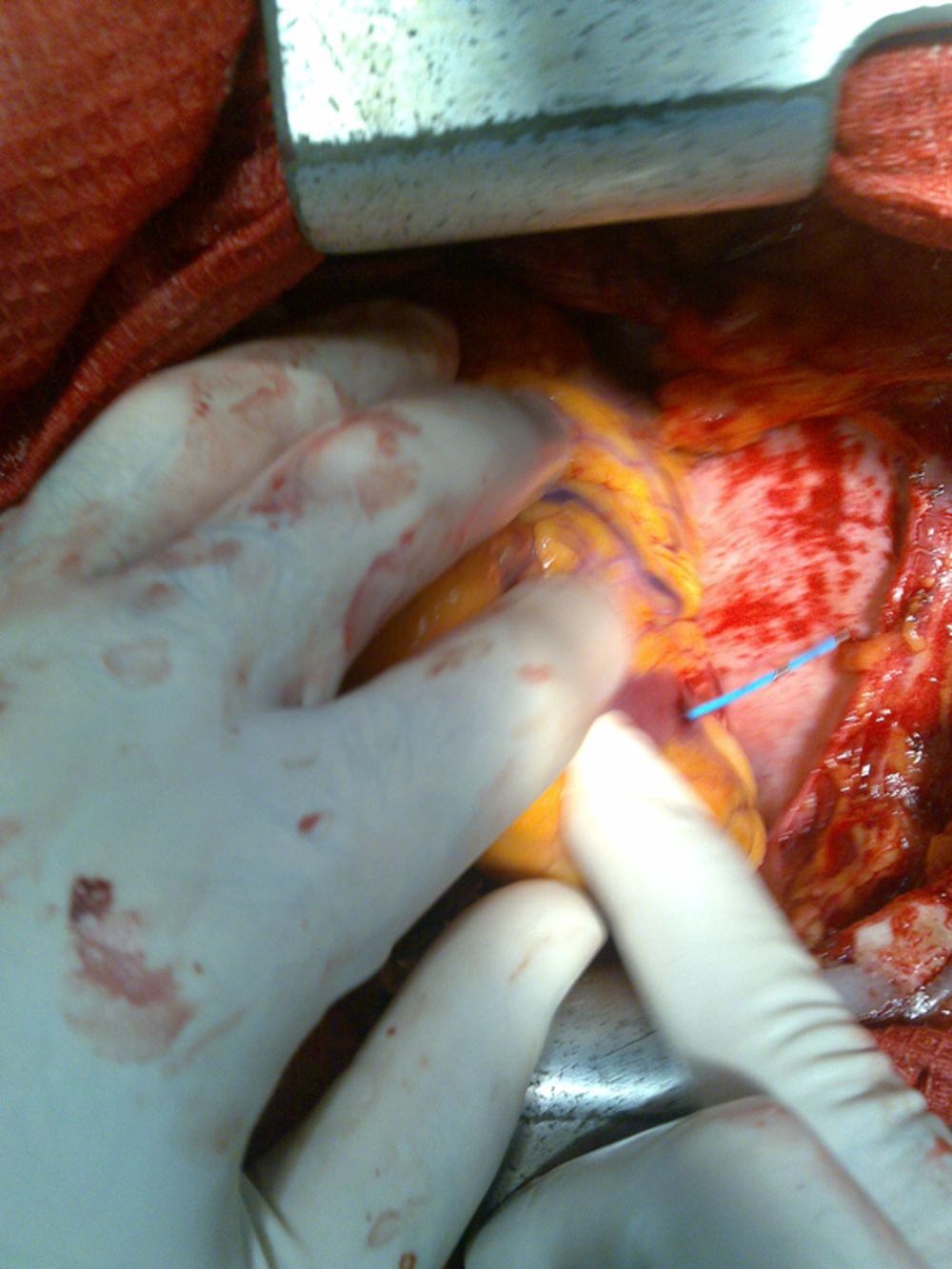
Under general anesthesia with standard monitoring for cardiac anesthesia using a bipolar ESU (electro surgical unit) and after completion of the anastomosis LIMA to LAD while lifting the cardiac ventricular apex for anastomosis to OM artery, suddenly the RV was perforated by the tip of the ventricular lead of the previous dual chamber pacemaker (Figure 2). Then, blood pressure decreased rapidly and the patient unexpectedly experienced cardiac arrest. Immediately, the patient was resuscitated with administration of epinephrine (up to 4 mg), atropine (up to 2 mg), and internal cardiac massage for 7 minutes. After establishing CPB (cardio-pulmonary bypass), dexamethasone 8 mg, thiopental sodium 3 mg/kg, lidocaine 1 mg/kg, and magnesium sulfate 30 mg/kg were administrated intravenously according to our institutional protocol. When all the grafts anastomoses were performed successfully, the RV perforation was repaired with a pledgetted mattress suture, and the perforated lead was withdrawn slowly as the suture was tightened.
Subsequently, the patient was rewarmed and weaned off CPB with the same single chamber permanent pacemaker (VOO Mode). The previous dual chamber pacemaker leads were not removed because of technical difficulties of extraction of the leads.
The operation was uneventful and the patient was extubated after 6 hours with the same permanent pacemaker (VOO Mode). He was completely alert with no hemodynamic complications. Finally, he was discharged from the hospital in a good overall condition, with the same single chamber permanent pacemaker (VVI mode).
3. Discussion
One of the potential complications of permanent cardiac pacing lead positioning is cardiac perforation, which can have severe clinical consequences including pericardial effusion, cardiac tamponade, pneumothorax, and death (3). RV perforation generally manifests during implantation or within 24 hours of implantation and has a prevalence rate of 0.1% to 6% (4, 5). The predictors of lead perforation are temporary pacemaker implantation, corticosteroid use, active fixation leads, low body mass index, old age, female gender, and concomitant anticoagulation therapy (6, 7). In our case, the intraoperative predictors of lead perforation were old age, concomitant anticoagulation therapy, leads of 2 pacemakers, and excessive manipulation of heart during OPCAB. Perforation most often occurs in the apex or free wall of the RV outflow tract, frequently at the time of pressure by straight stylet during implantation, which is perpendicularly transmitted to the heart wall, and when the excessive length of the lead under tension is left and generates additional force leading to perforation. As expected during OPCAB, greater changes arise when the heart is positioned to expose the lateral wall compared with the anterior aspect of the heart (6, 7).
Patient management strategy should depend on the dynamics of symptoms, pericardial effusion, and hemodynamic status (3). Some clinicians propose that the diagnosis of lead perforation requires lead removal. However, some other clinicians suggest that the removal of a chronically perforated lead in the absence of pacemaker malfunction is not necessary (8). The implantation of epicardial leads should be considered in the case of open chest surgery. Chowdhry V et al. reported a case of intra operative RV perforation due to temporary pacing catheter during OPCAB surgery. Their patient did not suffer a cardiac arrest and managed successfully with epicardial pacing during OPCAB surgery (2). However, in our case, the patient suffered from cardiac arrest, and intraoperative RV perforation seemed to be related to having 2 pacemakers’ leads and excessive manipulation of the heart during OPCAB surgery. Because cerebral injury is a major complication during cardiac arrest, thus a number of medications including steroids, magnesium sulfate, lidocaine and barbiturates, which seem to be useful in protecting the brain, were used (9).
3.1. Conclusion
Immediate changing from OPCAB to ONCAB surgery might be a life- saving method without any complication to adequately manage intraoperative right ventricular perforation accompanied by cardiac arrest even several minutes after cardiac arrest. Therefore, to avoid this complication, we advise an elective ONCAB surgery in such patients because it prevents the emergency conversion of OPCAB to ONCAB surgery, which has a very high mortality and morbidity.