1. Background
Endoscopic sinus surgery is the most common surgery in the field of ear, nose, and throat that causes improvements in clinical symptoms of the patients with rhinosinusitis (1). In ear, nose, and throat surgery, like other surgeries, an anesthesiologist plays an important role in the accurate and uncomplicated surgery (2).
Complications of surgeries are low but in case of major bleeding, they can affect the surgery’s outcome (3), following the onset of complications such as meningitis, blindness, and entering the intracranial space; it increases cerebrospinal fluid leakage (4).
To stop the bleeding, two procedures are typically used:
1. Local materials and vasoconstrictive and cocaine, phenylephrine, and epinephrine (5)
2. The creation of controlled hypotension
If the mean arterial pressure reaches less than 50 - 55 mmHg, controlled hypotension impairs the brain autoregulation and decreased coronary blood flow (CBF), especially causing cerebral ischemia in the elderly; for this reason, controlled hypotension is contraindicated in the people. Furthermore, in patients with coronary artery disease, controlled hypotension reduces the CBF and creates the risk of ischemic heart (6). Inhaled anesthetics such as isoflurane plus fentanyl narcotic such as remifentanil are extremely helpful to maintain blood pressure levels in a normal manner. Remifentanil, due to its efficiency, is constantly used in most cases (6, 7).
Isoflurane is an inhalation anesthetic drug and an isomer of enflurane (CHF2 - O - CHCl - CF3) that its metabolism is slower than halothane and enflurane. Isoflurane metabolism is a result of the oxidation of α-carbon that is made by the liver enzyme that consequently, trifluoromethylester metabolite is produced (7, 8).
Like other inhalational anesthetic agents, isoflurane determines drug concentrations in the CNS of anesthesia depth. The speed of reaching a sufficient concentration of drug to the CNS (Speed of the anesthesia induction) depends on several pharmacokinetic factors that affect drug absorption and distribution through the body. These factors also affect the speed of recovery from anesthesia after using the drug (8, 9).
Pharmacokinetic factors are affected by the solubility of gases, the relative gas pressure in the breathing air, the speed of ventilation, and the amount of blood flow to the lungs (9, 10).
The primary reason for the decrease in the mean of isoflurane-induced arterial pressure is a decrease in systemic vascular resistance. Reduction in systemic vascular resistance induced by isoflurane is dose-dependent that creates more hypertension drop at higher doses followed by tachycardia (9, 11).
Given the importance of bleeding and hemodynamic changes during endoscopic sinus surgery, we decided to assess different percentages of isoflurane in order to compare hemodynamic changes, as well as estimate the optimum effects of different percentages and suggest them to be used.
2. Objectives
This study aimed at comparing different doses of isoflurane on hemodynamic changes and bleeding in patients undergoing endoscopic sinus surgery under general anesthesia.
3. Methods
This study is an interventional randomized clinical trial in the operating room, Ahvaz Imam Khomeini hospital in the years 2014 - 2015 that was conducted after approval by the Ethics Committee, Ahvaz Jundishapur University of Medical Sciences (IRCT registration number: IRCT2016011526025N1). Based on the inclusion criteria, 90 patients, who were candidates for endoscopic sinus surgery and in the age range of 18 - 50 years, and ASA class I and II, were selected and divided into three groups based on random numbers. Before starting the study, written informed consent was obtained from all participants.
3.1. Inclusion Criteria
The 18 - 50 years old patients, who were candidates for endoscopic sinus surgery, ASA class I and II.
In all patients before induction of anesthesia, a standard monitoring, including ECG, noninvasive blood pressure, and pulse oximetry was performed.
3.2. Exclusion Criteria
A history of obstructive pulmonary problems, diabetes, uncontrolled high blood pressure, kidney disease, ischemic heart disease, liver disorders, drug sensitivity to isoflurane, and patient reluctance. Before the surgery, a blood sample was collected to determine Hb and Hct.
After receiving 5 cc/kg of crystalloid solutions and monitoring, ECG, Pulse oximetry, and NIBP, patients underwent an induction of general anesthesia with midazolam 0.05 mg/kg, fentanyl 2 μ/kg, sodium thiopental 5 mg/kg, atracurium 0.5 mg/kg and after four minutes, they were intubated with an appropriate-size tracheal tube and underwent the intermittent positive-pressure ventilation (IPPV).
After induction of anesthesia, for the maintenance of anesthesia the patients in the first, second, and third groups underwent isoflurane (manufactured by Piramal, America), respectively 1%, 1.2%, and 1.5% and received an infusion of remifentanil 0.1 μ/mg/min, as well.
To evaluate the hemodynamic conditions, the heart rate and blood pressure were monitored every ten minutes. Intraoperative bleeding during the surgery was measured as follows, suction and gauzes (a small gauze was considered 20 cc and a long gauze completely soaked in blood was considered to be 50 cc. All surgeries were done by an expert surgical team.
The aim of systolic blood pressure was 90-100 mmHg and if systolic blood pressure was lower than 80 mmHg and mean arterial BP was less than 60 mmHg, the case was positive and for the treatment. In addition to the administration of fluids, the injection of remifentanil infusion and blood pressure correction were stopped.
After the end of the surgery, the anesthesia in three drug-receiving groups was stopped and after spontaneous breathing, neostigmine 0.05 mg/Kg and atropine 0.02 mg/kg were reversed and the endotracheal tube was removed.
After transferring the patient to the recovery ward, a blood sample was taken from all patients for the determination of Hb six hours after the surgery. The operation time was recorded.
3.3. Statistical Analysis
All data were analyzed by the SPSS version 22 and one-way analysis of variance (ANOVA), analysis of completed or post hoc with Tukey test, repeated measures ANOVA and descriptive analyses, including mean, standard deviation, and frequency distribution were performed. The P value < 0.001 was considered statistically significant.
4. Results
In this study, patients were divided into three groups, of which 52 patients were male and 38 were female. The average age of 1, 2, and 3 groups was 38.03, 35.07, and 31.73 years, respectively. There was not a statistically significant difference among the three groups.
Before and after induction, there was no significant difference among the three groups.
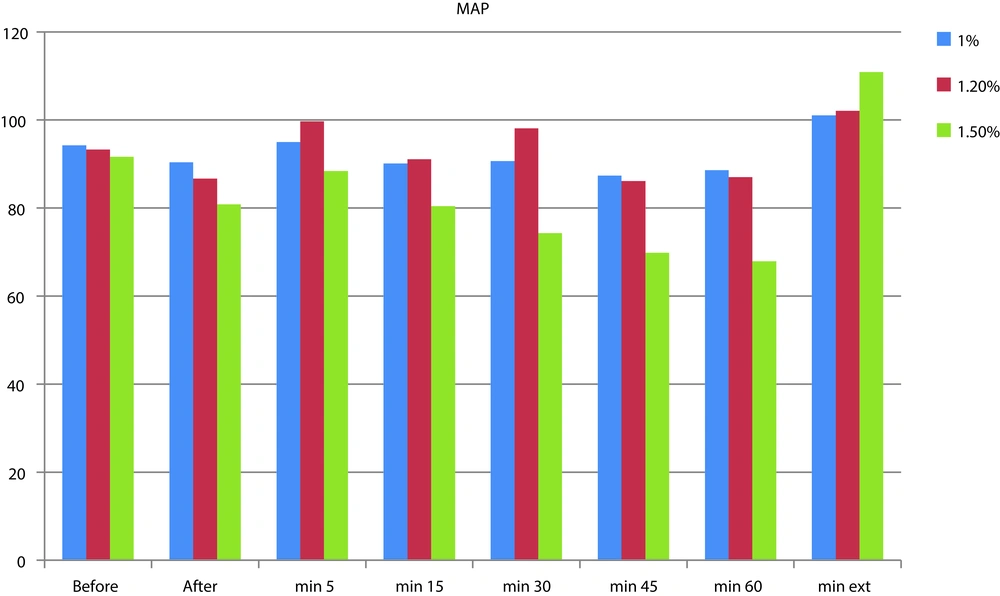
There was a significant difference between group 2 in MinBP and minHR at minute of 5 (Table 1 and Figure 1).
| MinBP Time | Group 1 | Group 2 | Group 3 | P Value | ||
|---|---|---|---|---|---|---|
| Groups 1 and 2 | Groups 1 and 3 | Group 2 and 3 | ||||
| Before induction | 7.64 ± 94.22 | 8.22 ± 93.27 | 6.03 ± 91.66 | 20.440 | 0.520 | 0.426 |
| After induction | 7.51 ± 90.38 | 6.41 ± 86.68 | 6.97 ± 80.83 | 0.106 | 0.005 | 0.018 |
| In minute of 5 | 8.58 ± 95.00 | 5.55 ± 99.71 | 5.88 ± 88.41 | 0.024 | 0.001 | 0.0001 |
| In minute of 15 | 6.54 ± 90.13 | 5.94 ± 91.11 | 7.45 ± 80.44 | 0.838 | 0.0001 | 0.0001 |
| In minute of 30 | 9.37 ± 90.69 | 6.72 ± 89.11 | 7.56 ± 74.33 | 0.724 | 0.0001 | 0.0001 |
| In minute of 45 | 9.07 ± 87.37 | 6.16 ± 86.14 | 8.31 ± 69.83 | 0.820 | 0.0001 | 0.0001 |
| In minute of 60 | 5.54 ± 88.64 | 8.24 ± 87.05 | 7.73 ± 67.92 | 0.675 | 0.0001 | 0.0001 |
| After extubation | 5.95 ± 101.08 | 102.11 ± 5.80 | 7.88 ± 110.87 | 0.416 | 0.486 | 0.491 |
Comparison of MinBP in Groups 1, 2, and 3
BP in 15, 30, 45 and 60 minutes showed significant differences among 1, 2, and 3 groups (Table 1).
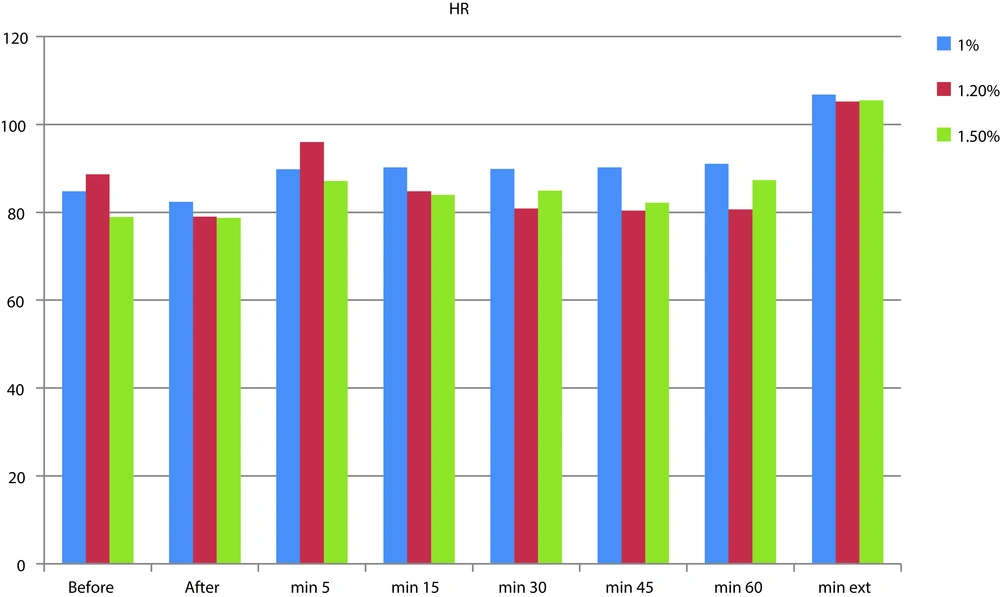
There was a significant difference among 1, 2 and 3 groups in MinBP at minutes of 15, 30, 45, and 60 (Table 2 and Figure 2).
| HR Time | Group 1 | Group 2 | Group 3 | P Value | ||
|---|---|---|---|---|---|---|
| Groups 1 and 2 | Groups 1 and 3 | Groups 2 and 3 | ||||
| Before induction | 11.49 ± 84.80 | 14.50 ± 88.66 | 9.42 ± 78.93 | 0.428 | 0.146 | 0.006 |
| After induction | 16.51 ± 82.37 | 9.49 ± 79.00 | 6.78 ± 78.73 | 0.123 | 0.014 | 0.201 |
| In minute of 5 | 8.12 ± 89.80 | 9.49 ± 95.96 | 6.08 ± 87.13 | 0.010 | 0.406 | 0.0001 |
| In minute of 15 | 9.30 ± 90.27 | 7.98 ± 84.77 | 4.45 ± 83.94 | 0.020 | 0.006 | 0.910 |
| In minute of 30 | 11.22 ± 89.86 | 7.13 ± 80.88 | 5.09 ± 84.90 | 0.0001 | 0.056 | 0.136 |
| In minute of 45 | 90.23 ± 9.82 | 7.70 ± 80.40 | 7.37 ± 87.20 | 0.0001 | 0.344 | 0.0065 |
| In minute of 60 | 11.23 ± 91.03 | 6.35 ± 80.66 | 6.43 ± 87.33 | 0.0001 | 0.203 | 0.007 |
| After extubation | 10.23 ± 106.80 | 9.43 ± 105.23 | 7.78 ± 105.46 | 0.789 | 0.842 | 0.995 |
Comparison of HR in Groups 1 and 2 and 3
There was a significant difference between group 1 and 2 in HR at minutes of 15, 30, 45, and 60 (Table 2).
There was not a significant difference among the groups in MinBP and HR after extubation.
The average operation time in 1, 2, and 3 groups were 90.15 minutes, 88.26 minutes, and 88.96 minutes, respectively; Thus there was no significant difference among the three groups (Figure 2).
There was not a significant difference in HR before and after surgery among the three groups.
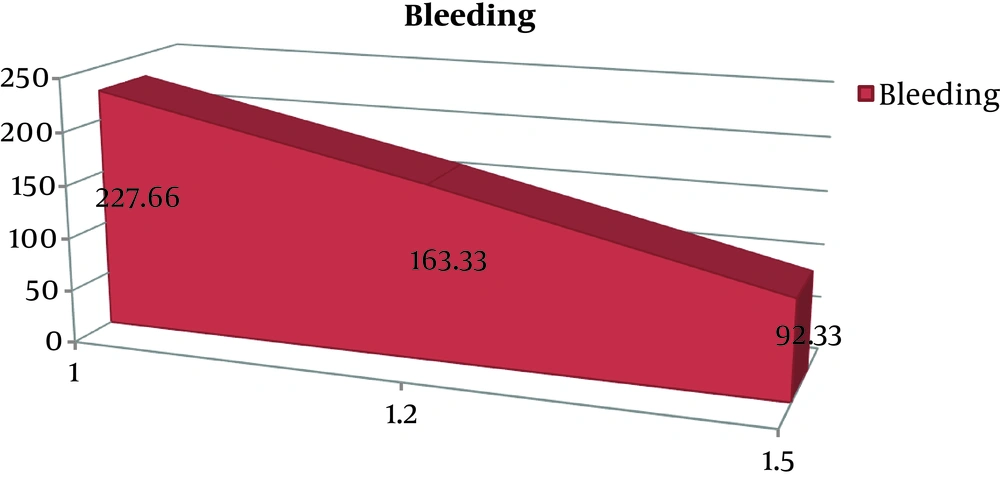
The mean of bleeding in the first group (227.66 cc), second group (163.33 cc) and third group (92.33 cc) were significantly reduced (P = 0.011). There was a significant difference between groups 1 and 2, groups 1 and 3, and groups 2 and 3 (Table 3 and Figure 3).
| Intra-Operating Bleeding | |
|---|---|
| Group 1 | 227.66 ± 95.4 |
| Group 1.2 | 163.33 ± 54.35 |
| Group 1.5 | 92.33 ± 44.32 |
| P value | 0.0001 |
Intraoperative Bleeding in Three Groups (Mean ± SD)
There was not a significant difference in hemoglobin changes before and after surgery among three groups (Table 4).
| Before | After | |
|---|---|---|
| Group 1 | 15.26 ± 1.34 | 12.73 ± 1.24 |
| Group 1.2 | 13.2 ± 1.86 | 12.9 ± 1.18 |
| Group 1.5 | 13.30 ± 1.01 | 13.2 ± 1.48 |
| P value | 0.446 | 0.892 |
Hemoglobin Before and After Operation (Mean ± SD)
5. Discussion
As the results showed, there was a significant difference mean of arterial blood pressure in 15, 30, 45, and 60 minutes between groups 1 and 2 and also between groups 2 and 3, which showed there was a greater reduction in mean blood pressure following an increase in the percentage of isoflurane gas.
Furthermore, there was a significant difference in the heart rate in 30, 45, and 60 minutes between groups 1 and 2 and the average heart rate in the group 2 was less than in the group 1 in different time periods.
There was a significant difference in the amount of bleeding between groups 1 and 2, as well as between groups 2 and 3, which implies a greater reduction in the amount of bleeding following an increase in the percentage of isoflurane gas.
In a study in America in 1999, Pavlin et al. compared the effects of Pofol and isoflurane in endoscopic sinus surgery. The groups receiving isoflurane 2% and Pofol, both were treated with infusion 200 mcg/min. In this study, the amount of bleeding in Pofol group was 53.44 cc and in isoflurane group, it was 94.88 cc that there was a statistically significant difference (P value < 0.001); moreover, the results of our study in the 2% isoflurane group were similar to 1.5% isoflurane group.
In a study conducted by Ghodrati et al. in Firuzgar Hospital, Tehran in 2011, the maintenance of anesthesia was done with continuous infusion of 100 - 150 mcg/kg/min in the Pofol group, and in the isoflurane group after induction of anesthesia. Two percent isoflurane1 and remifentanil 0.1 - 0.25 μ/kg were used in the two groups. The results of the study showed that the average amount of bleeding in Pofol group (35.3 ± 1 cc) was less than the amount of bleeding in the isoflurane group (91.1 cc) (P value = 0.001); Therefore, it is concluded that is an amount of bleeding in the isoflurane group (91.18 cc) in this finding is consistent with our study in group 3 that received isoflurane 1.5% (92.33).
In a study by Hasani et al. in Rasul Akram Hospital, Tehran in 2003, a comparison between two groups: Remifentanil-pofol A, and isoflurane-remifentanil B showed that the amount of bleeding in group A was 28.47 cc and in group B it was 28.47 cc, which there was not a significant difference between the two groups. In this study, 1% isoflurane was used.
In a study published in 2005, Manola et al. showed that a combination of remifentanil-pofol and a combination of sufentanil-sevoflurane are effective in improving hemodynamic conditions in patients undergoing endoscopic sinus surgery (12).
In a study in Germany in 2003, Eberhart et al. confirmed the improvement of hemodynamic conditions by the use of Alfentanil-isoflurane compared with propofol and remifentanil that this result is not consistent with our study (13).
In a study in Tehran in 2004, Sadeghi et al. compared the mean arterial blood pressure in two groups: Isoflurane-remifentanil and group B propofol-remifentanil, subsequently the study’s findings showed that there was a significant difference between the two groups, thus a combination of isoflurane and remifentanil may help to maintain hemodynamic stability (14).
In a study in Mashhad in 2009, Hosseinzadeh et al. found a significant relationship between two groups: Isoflurane and completely intravenous method, additionally they indicated that heart rate drop was longer than inhalation using intravenous anesthesia.
5.1. Study Limitations
Among the obstacles during the study, it can be pointed out to the problem of preparing remifentanil drugs in a short period of time, which was resolved in coordination with the drug distribution center. Overall, based on the findings from this study and comparing it with other studies in this field, it can be inferred that the combination of isoflurane is an important help for maintaining the hemodynamic stability. To control blood pressure and reduce bleeding during endoscopic sinus surgery, 1.5 and 1.2 percent isoflurane are recommended; however, it is recommended that further studies should be done in this regard.