1. Background
The major classification of difficult laryngoscopy is defined by Cormack-Lehane as a view of the glottis during laryngoscopy. The incidence of difficult intubation is estimated 3% - 18%. Difficult intubation is associated with serious complications such as brain damage due to hypoxia and hypocarbia (1). Other side effects include tooth damage caused by repeated attempts at intubation, laryngospasm, and bronchospasm (1). The ability of anesthesiologist to predict the likelihood of difficult intubation, accurate training of resident anesthesiologists or clinicians, and the use of advanced equipment for intubation can significantly reduce the risk of anesthesia and increase the success rate of intubation (2-4). Endotracheal intubation is an important step in all cases of general anesthesia and should be performed quickly and correctly. Effective airway management is also the main part of emergency situations and resuscitations. In some situations such as obesity, a difficult intubation can be anticipated; therefore, alternative methods and devices should be considered before induction of anesthesia (5).
The Macintosh laryngoscope blade is commonly used, but sometimes maintenance of the airway and intubation is difficult. Owing to these difficulties and for intubation training, other devices such as GlideScope® and the laryngeal mask airway should be available. Literature reviews showed that various devices for difficult intubation are made and tested such as the video laryngoscope GlideScope® (GVL, Saturn Biomedical System Inc.), which is widely used in difficult intubations (6, 7), and the McCoy laryngoscope with a flexible blade (2).
Therefore, the current study aimed at comparing 3 laryngoscopes, namely the McCoy, GlideScope®, and Macintosh laryngoscopes, in patients with obesity that intubation is usually difficult for them and previous studies produced conflicting results (8-10).
2. Methods
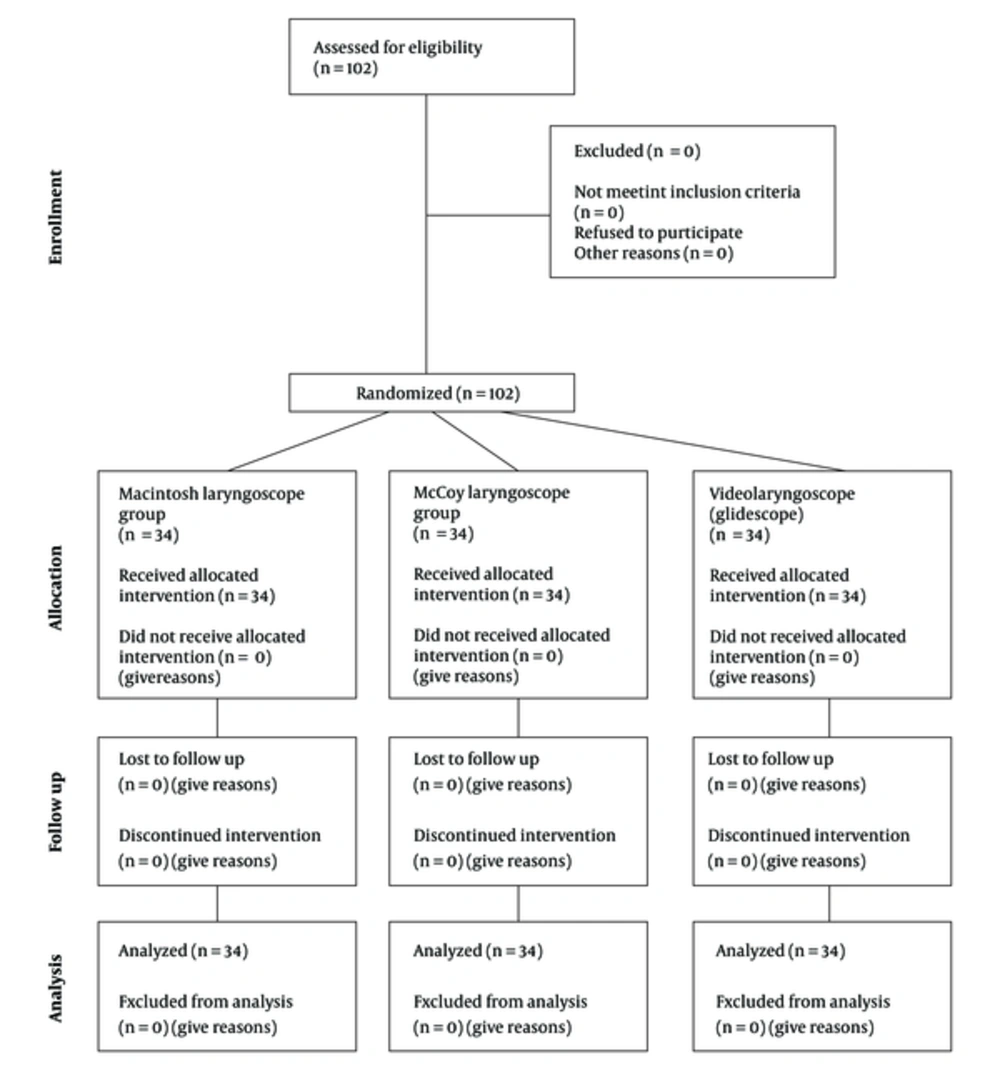
In the current prospective, randomized clinical trial, after receiving approval from the vice chancellor for research and local ethics committee of Mashhad University of Medical Sciences (No. 931362), 102 patients with obesity who were candidates for elective surgery and had ASA (American society of anesthesiologists) class I or II physical status were selected. The patients had a body mass index (BMI) of > 30 kg/m2 (Figure 1). Before surgery, written informed consent was obtained from the patients. Patients with renal insufficiency (Creatinine level of > 1.5 mg/dL) and impaired liver function (aspartate aminotransferase (AST) level of > 40 U/L and alanine aminotransferase (ALT) level of > 40 U/L) due to airway edema or intubation delay problems; ischemic or valvular heart disease; airway trauma; abscess or lump in the neck or throat; oropharyngeal masses, neck, pharynx, or larynx; and coagulopathy were excluded from the study.
At the physical preoperative examination, airway assessment was performed including Mallampati score, thyromental distance (TMD), and neck circumference. The patients were monitored (heart rate, blood pressure, and peripheral capillary oxygen saturation) and infused simultaneously with 5 mL/kg saline. Subsequently, all the patients were anesthetized using the same technique with 40 µg/kg midazolam, 2 µg/kg fentanyl, 5 mg/kg thiopental, and 0.6 mg/kg atracurium.
All the patients were equally and randomly divided into 3 groups with a random number generator and numbered envelops (Figure 1). Subsequently, the patients in each group were intubated using the Macintosh, McCoy, or GlideScope® laryngoscope, and capnography was used to confirm successful intubation. All the intubations were performed by the same person. The patients were blind to their groupings, but blinding of the anesthesiologist was not possible. The number of attempts required for successful intubation, and the laryngoscopy time (time from entry of the laryngoscope into the mouth until tube insertion) were recorded. On the basis of the observed laryngoscopic view, the Cormack-Lehane score (1 - 4) and percentage of glottic opening (POGO; 1% - 100%) were recorded for each patient. The POGO represents the POGO observed, defined by the linear span from the anterior commissure to the interarytenoid notch. The POGO replaces the Cormack-Lehane grades 1 and 2 with a continuous numerical value. A 100% POGO is a full view of the glottis from the anterior commissure to the interarytenoid notch. A POGO of 0 means that even the interarytenoid notch is not seen. Alternative methods for difficult intubation, such as fiberoptic laryngoscopy and laryngeal mask airway were also available for use.
2.1. Statistical Analyses
The sample size in the 3 groups was calculated based on the study by Tseng (11) using the SigmaPlot version 12.5 software (2015; Systat Software Inc. San Jose, USA). According to the expected difference in mean intubation time among the groups, which was 10 seconds, at least 33 patients were needed in each group; with a first type of error of 0.05 (α = 0.05) and a confidence coefficient of 80% (β = 0.2); 34 patients were enrolled in each group.
To perform data analysis, the SPSS software version 16 (SPSS Inc.,IL, USA) was used. The Kolmogorov-Smirnov test was used to test the normal distribution of data. Continuous variables were expressed as mean ± standard deviation (SD), and categorical variables as frequencies and percentages. To compare quantitative variables with normal distributions in the 3 groups, analysis of variance (ANOVA) with a post hoc Tukey test was used; in case of non-normal distribution, a Kruskal-Wallis test. Categorical data were analyzed using chi-square test or the Fisher exact test. To investigate the correlation between the 2 variables, the Spearman correlation test was used. A P value of ≤ 0.05 (2-sided) was considered to indicate a statistically significant result.
3. Results
The demographic characteristics of the study patients including gender, age, and BMI, as well as preoperative examination results such as Mallampati score, neck circumference measurement, and TMD are shown in Table 1. No statistically significant difference was observed among the 3 groups, indicating that the general characteristics of the 3 study groups were comparable.
The laryngoscopy times (from entry of the laryngoscope until tracheal tube insertion), the Cormack-Lehane scores during laryngoscopy, and POGO are shown in Table 2. The shortest laryngoscopy time was in the GlideScope® group, and the longest time was in the McCoy laryngoscope group, with statistically significant differences (P = 0.001). The highest Cormack-Lehane score was observed when the GlideScope® method was used (P = 0.04). The POGO achieved during laryngoscopy using the McCoy laryngoscope was the highest and therefore, the most appropriate (P = 0.009).Success rate, defined as the number of attempts taken to achieve a successful intubation, was evaluated and no significant difference was observed among the 3 groups (P = 0.2).
In the current study, the relationships of laryngoscopy time with demographic parameters and preoperative examination results were compared. A positive significant relationship was observed between BMI and laryngoscopy time (P = 0.023). BMI was not significantly different among the 3 groups; therefore, this variable was not a confounder. A direct relationship was observed between neck circumference and laryngoscopy time (P = 0.008). Mallampati score had a significant relationship with laryngoscopy time (P = 0.000).
| Parameter | GlideScope® (N = 34), | Macintosh Laryngoscope (N = 34) | McCoy Laryngoscope (N = 36) | P Value |
|---|---|---|---|---|
| Male | 16 (47) | 17 (50) | 24 (67) | 0.2* |
| Age, t | 46.55 ± 10.55 | 46.52 ± 11.09 | 45.8 ± 10.81 | 0.9** |
| BMI, kg/m2 | 34.64 ± 1.75 | 34.63 ± 2.02 | 33.98 ± 2.3 | 0.3** |
| Malampati score (1 - 4) | 2.36 ± 0.6 | 2.59 ± 0.7 | 2.36 ± 0.6 | 0.4** |
| Thyromental distance, cm | 2.84 ± 0.36 | 2.64 ± 0.4 | 2.75 ± 0.4 | 0.14** |
| Neck circumference, cm | 43.36 ± 2.1 | 43.67 ±1.5 | 43.69 ± 1.9 | 0.8** |
Demographic Dataa
| Parameter Assessed | GlideScope® (N = 34) | Macintosh Laryngoscope (N = 34) | McCoy Laryngoscope (N = 36) | P Value* |
|---|---|---|---|---|
| Intubation time, min | 10.8 ± 23.82 | 11.18 ± 28.44 | 14.3 ± 34.47 | 0.001 |
| Cormack-Lehane score (1 - 4) | 1.9 ± 0.8 | 1.76 ± 0.81 | 1.52 ± 0.9 | 0.04 |
| POGO score (1 - 100) | 62 ± 28 | 69 ± 30 | 82 ± 31 | 0.001 |
Comparison of Intubation Time, Cormack-Lehane Score, and POGO in the Study Groups in Patients with Obesitya
4. Discussion
Results of the current study showed significant differences in laryngoscopy time among the 3 methods. Some studies showed that Macintosh laryngoscope provided a superior glottis view in comparison with the standard blade and McCoy laryngoscopes (9, 12). On the other hand, in other studies, McCoy or standard blade laryngoscopes provided better glottis views on laryngoscopy and intubation (8, 13, 14).In the current study, the POGO obtained with the McCoy laryngoscope was significantly higher than the ones obtained with the 2 other methods, but the laryngoscopy time when using the McCoy laryngoscope was longer than those of the 2 other methods.
On the other hand, increased intubation time was among the influencing factors of hypoxia (6); therefore, methods that can decrease intubation time can solve the intubation problems in people with obesity to a large extent. In a previous study, the authors stated that GlideScope® laryngoscope could decrease intubation time better than Macintosh laryngoscope (6). In another study, the authors stated that both the GlideScope® and video laryngoscopes were more appropriate than the Macintosh laryngoscope for airway management (8).
In another study, the intubation success rate with the GlideScope® laryngoscope was higher than that of the Macintosh laryngoscope. Intubation time was also shorter in the GlideScope® group (10). However, some other studies indicated that the Macintosh laryngoscope was better and more rapid than the video laryngoscope (15-18). The Macintosh laryngoscope, with a shorter intubation time, was superior. In the current study, the success rate showed no significant difference among the three groups (P = 0.2).
In fact, airway management is one of the main challenges in patients with obesity. Accurate training of resident anesthesiologists or clinicians, and the use of advanced equipment for intubation can significantly reduce the risk of anesthesia and increase the success rate of intubation. Patients with obesity are at risk of hypoxemia during endotracheal intubation due to the increased frequency of intubation and decreased apnea tolerance (3, 4, 6). Previous studies investigated the problems associated with laryngoscopy in people with obesity and reported that age, gender, and the position of the upper teeth could become a problem in laryngoscopy, but BMI did not have any effects (19). Intubation problems are directly linked to laryngoscopy, and it is reported that laryngoscopic problems are directly linked to BMI (20). Some studies concluded that intubation is more difficult in patients with obesity than in patients with normal weight (20-22); whereas in another study, no relationship was observed between BMI or obesity and intubation (1). In the current study, BMI and neck circumference were directly related to laryngoscopy time and tracheal tube insertion, because as BMI and neck circumference increase, longer time is needed for laryngoscopy.
A previous study suggested that intubation of patients with obesity takes slightly longer time using the GlideScope® laryngoscope than the Macintosh direct laryngoscope, possibly due to the narrow oropharyngeal space (6). However, in the current study, laryngoscopic and intubation time in patients with obesity was shorter using the GlideScope® laryngoscope than the Macintosh and McCoy laryngoscopes.
The first limitation of the current study was the absence of comparison between specialists with different levels of experience in video laryngoscopy, which had a significant influence on the evaluation methods used. The second limitation was the lack of blinding to the intubation methods used in the study. The third limitation was that the assessments of the POGO and Cormack-Lehane scores were subjective, not purposeful and accurate. The fourth limitation was insufficient experience with the McCoy laryngoscope.
In conclusion, in the current study, the best method to reduce intubation time in patients with obesity was employing the GlideScope® laryngoscope, and the least appropriate method was employing the McCoy laryngoscope. In addition, the direct relationships of BMI and neck circumference with laryngoscopy time were observed in all the three methods. The obtained results suggested that in patients with high BMI, the GlideScope® laryngoscope should be used to reduce laryngoscopy time.