1. Background
Pain is one of the most common symptoms in patients in the emergency departments (EDs) (1, 2). Furthermore, effective pain reduction increases the patient satisfaction and prevents delayed physical and mental complications such as persistent pain syndrome and pain related anxiety as well as distress (3, 4).
Intravenous opium (morphine) is the most common medication used to decrease pain in the EDs (5-7). Despite the analgesic benefits and availability of morphine, it has some complications such as over sedation and respiratory depression (8). On the other hand, usual dose of 0.1 mg/kg of morphine cannot suppress the severe pain of many patients in EDs (9). Ketamine is an N-methyl-D-aspartate (NMDA) receptor antagonist, which has been utilized since 1970s for anesthesia (10). Due to the rapid onset and the absence of significant respiratory complications, it has been taken into consideration in EDs for procedural sedation analgesia and pain management (11, 12).
Low dose ketamine (LDK), by definition, is applied to doses less than 1 mg/kg (13). From several studies, it has been demonstrated that the addition of LDK to morphine reduced the dose of morphine and its complications (14, 15). Few studies have been carried out to investigate the analgesic effect of ketamine as a single agent in EDs. To the best of our knowledge, this is the first study that compared intravenous LDK at a dose of 0.2 mg/kg with morphine in trauma patients with a large sample size.
2. Objectives
In this study, we compared the analgesic effect of ketamine at a dose of 0.2 mg/kg with intravenous morphine at a dose of 0.1 mg/kg and the secondary outcome was to compare the side effects of these medications.
3. Methods
3.1. Study Designs and Participants
This randomized double-blinded clinical trial was carried out to compare the efficacy and safety of intravenous LDK with intravenous morphine for pain management of trauma patients in the emergency departments of 2 university teaching hospitals (Hazrat Rasool and Haftom Tir) in Tehran, Iran from September 2014 to September 2015. The study was approved by the Iranian registry of clinical trials (IRCT2015111024979N1). The study included trauma patients aged 18 to 70 years with a musculoskeletal pain score of 5 or more on a standard 11-point (0 to 10) numeric rating scale who were referred to the emergency departments. The study protocol was approved by the ethics committee of Iran University of Medical Sciences. Patients who met the following criteria were excluded from the study: instability in vital signs, head trauma, Glasgow coma scale score less than 15, opiate users, psychiatric or cardiac problem, hypersensitivity to ketamine or morphine, pregnancy, breast-feeding, renal or hepatic insufficiency, and contraindications to use both medications such as upper respiratory infections or hypersensitivity.
At first, consent forms containing detailed information of the study were given to the patients and those who declared their satisfaction in participation were included to the study.
3.2. Study Instrument
Pain measurement was accomplished using a 10-cm line with tick marks spaced 1 cm apart. The leftmost mark is labeled “0” and means “no pain” and the rightmost mark is labeled “10” and means “the worst pain imaginable”.
3.3. Intervention
Baseline pain score was determined with numeric rating scale. Patients with pain score of 5 or more were included.
First, baseline characteristics and clinical data were recorded according to the patients’ interview. Then, the patients were randomly assigned (by block randomization method) to 2 groups. The 1st group received 0.2 mg/kg of ketamine and the 2nd group received 0.1 mg/kg of morphine. Each syringe contained a clear colorless solution of either 2 mg/mL ketamine or 1 mg/mL morphine. The medication was injected intravenously by a nurse who was blind to the study protocol. Sufficient pain reduction was defined as a decrease in pain score equal to 3 or more (16). In case of insufficient pain reduction, 3 milligrams of intravenous morphine was injected every 5 minutes as a rescue analgesic. Pain score, blood pressure, heart rate, pulse-oxygen saturation, and drug side effects were assessed at 0, 15, 30, 45, and 60 minutes after drug administration. Nausea was managed by antiemetic. Hypotension was considered present when the systolic blood pressure dropped to 90 mmHg and managed by bolus of fluid. Desaturation was defined as an oxygen saturation of < 92% and managed by head tilt-chin lift and bag- mask ventilation, as needed. Bradycardia was mentioned when the heart rate dropped to less than 60 per minute and managed by 0.5 mg intravenous atropine.
Patient satisfaction was asked 1 hour after drug injection by 5 points level of quality as excellent (point 5), very good, good, fair, and poor. The answers of excellent and very good were supposed as reaching proper analgesic effect.
3.4. Statistical Analysis
Data were analyzed by the SPSS 18 software. Results were presented as mean ± standard deviation for quantitative variables. Pain scores were compared with independent t-test to compare LDK and morphine groups. Paired t-test was used to compare pain scores within groups. All of categorical variables were analyzed by the chi-square test except patient satisfaction, which was analyzed by Fisher’s exact test. A P value of less than 0.05 was considered statistically significant.
The sample size was calculated using the following formula: n = 2 (Z1 - α + Z1 - β)2 σ2 / d2. Effect size (d) and σ was considered 3 and 9, respectively, based on the literature review. Thus, the sample size in each group (LDK or morphine) should be at least 142 patients. We enrolled 332 patients initially to cover the probable data loss.
4. Results
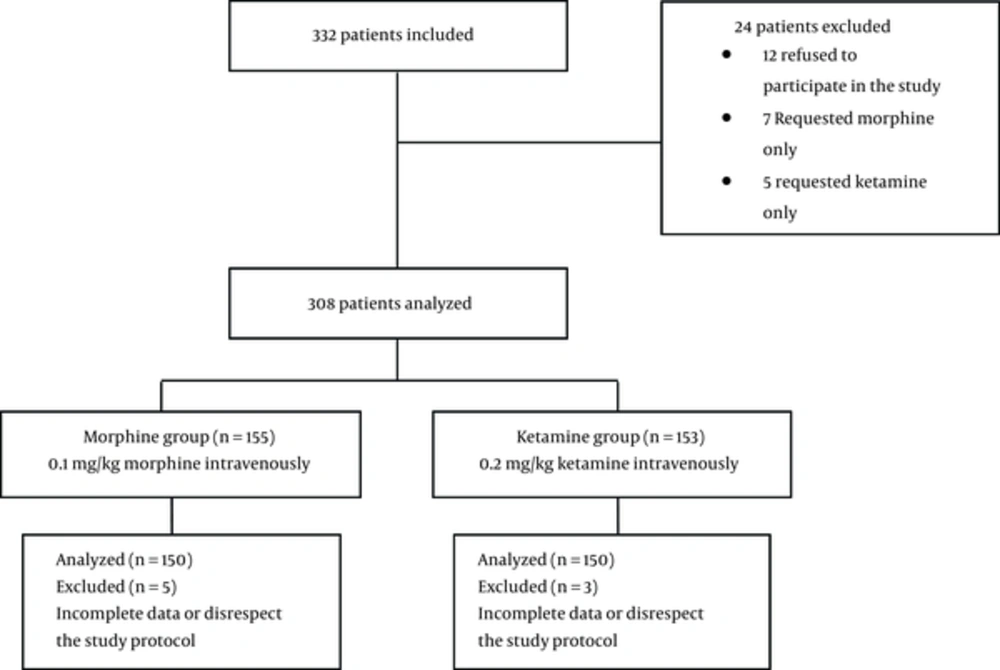
A total of 332 patients were enrolled in the study, however, 32 of them were excluded. All of the 300 patients were randomly divided into 2 equal groups of LDK and morphine. The patient flow diagram is shown in Figure 1. Patients’ demographic characteristics are shown in Table 1. The patients’ mean ages were 34.4 ± 7.6 and 34.1 ± 7.3 years in LDK and morphine groups, respectively. There was no difference between the groups in terms of demographic characteristics (except in weight) or vital signs and baseline pain scores.
| Variables | Morphine Group, n = 150 | Ketamine Group, n = 150 | P Value |
|---|---|---|---|
| Age, mean (SD), y | 34.1 ± 7.3 | 34.4 ± 7.6 | 0.93 |
| Sex, male (%) | 123 (82) | 126 (84) | 0.79 |
| Weight, kg | 68.4 ± 12.9 | 75.1 ± 14.6 | 0.018* |
| Final diagnosis, n (%) | |||
| Fracture | 36 (24) | 42 (28) | 0.64 |
| Soft tissue injury | 114 (76) | 108 (72) | 0.68 |
| Initial vital signs | |||
| SBP, mean (SD), (mm/Hg) | 124.7 ± 12.3 | 123.2 ± 16.4 | 0.60 |
| DBP, mean (SD), (mm/Hg) | 82.2 ± 10.6 | 78.9 ± 13.7 | 0.17 |
| Heart rate, mean (SD), (beats/min) | 81 ± 9.5 | 79.2 ± 12.6 | 0.42 |
| Oxygen saturation, mean (SD), (%) | 97.1 ± 1.4 | 96.6 ± 2.3 | 0.17 |
| Rescue analgesic, n (%) | 15 (10) | 51 (34) | 0.001* |
| Patient satisfaction | |||
| T60, n (%), excellent or good | 114 (76) | 66 (44) | 0.001* |
Patients’ Characteristics and Vital Signs
The mean dose of morphine and ketamine in each group were 6.8 ± 1.2 mg and 14.9 ± 3.3 mg, respectively. A total of 51 patients in the ketamine group and 15 patients in the morphine group required an extra dose of the analgesic (P = 0.01).
In both groups, 15 minutes after injection (T15), the mean pain intensity when compared to the initial pain (T0) had a statistically significant reduction (P = 0.01). Moreover, there was no significant difference between both groups at baseline and T15 in terms of the mean pain intensity. The mean pain intensity at 30, 45, and 60 minutes in the group receiving morphine was lower than the ketamine group and the difference was statistically significant (P = 0.01, P < 0.001, P < 0.001, respectively). In other words, the analgesic effect of ketamine was reduced by passing the time of injection (Table 2).
| Time (min) | Group | P Value | |
|---|---|---|---|
| Ketamine | Morphine | ||
| T0 | 8.1 ± 1.1 | 8.4 ± 0.9 | 0.15 |
| T15 | 4.1 ± 2.8 | 4 ± 2.5 | 0.23 |
| T30 | 4.5 ± 3.1 | 3.8 ± 3 | 0.01* |
| T45 | 4.8 ± 3.2 | 3.4 ± 3.1 | < 0.001* |
| T60 | 4.9 ± 3.3 | 3.2 ± 2.9 | < 0.001* |
Pain Scores (Numeric Rating Scale)
One hour after injection, when the sedation effect of drugs has subsided, the patients’ satisfaction was evaluated. A total of 114 patients of morphine group and 66 patients of ketamine group were satisfied with analgesic effect (P = 0.001).
No life-threatening complication was observed in both groups. Complications include nausea, reduced O2 saturation, dizziness, mood changes, and flushing; all complications were temporary and required no intervention other than oxygenation with nasal cannula. A drop in O2 saturation below 90% and flushing were significantly higher in the morphine group (Table 3).
| Number (%) | Group | P Value | |
|---|---|---|---|
| Ketamine | Morphine | ||
| Nausea | 24 (16) | 26 (17) | 0.51 |
| Flushing | 0 | 54 (36) | < 0.001* |
| Dizziness | 51 (34) | 48 (32) | 0.83 |
| Mood changes | 6 (4) | 4 (2) | 0.24 |
| O2 saturation < 90% | 6 (4) | 27 (18) | 0.02* |
| Hypotension, (SBP < 90 mmHg) | 0 | 0 | - |
Adverse Effects
5. Discussion
The results of this study further illustrated that ketamine, at a dose of 0.2 mg/kg 15 minutes after injection, dramatically reduced the pain in trauma patients. When compared with morphine, there was no statistically significant difference in T15.
Few studies have been carried out to investigate the analgesic effect of pure ketamine in EDs. Ahern et al. (17) carried out a retrospective case series study over 2 years and examined the effects of ketamine in a variety of acute and chronic pain in ED. Ketamine dose utilized was 0.1 to 0.3 mg/kg (5 to 25 mg IV or IM) alone or in combination with other tranquilizer. Of the patients, 92% received 10 to 15 mg of Ketamine. A total of 6% of patients experienced complications, most of them were non-significant. Finally, it can be concluded that LDK is a safe and effective pain relief in ED.
Majidinejad et al. (18) compared 0.5 mg/kg dose of ketamine with 0.1 mg/kg of morphine in 126 emergency patients with long bone fracture. In this study, the reduction of pain in the ketamine group, within 10 minutes after injection, was significant, which was equivalent to morphine group. The complication rate was also significantly higher in the ketamine group.
Motov et al. (19) conducted a study on 90 ED patients with a variety of pains with NRS equal or more than 5. He divided them into 2 groups of 45 subjects and compared the analgesic effect and complications caused by 0.3 mg/kg of ketamine and 0.1 mg/kg of morphine 120 minutes after injection. In this study, LDK was effective in the short term on pain relief similar to morphine. Hence, the rate of complications in the ketamine group was significantly higher than the morphine group.
Miller et al. (20) performed a study on 45 patients (21 patients received 0.1 mg/kg morphine and 24 patients received 0.3 mg/kg ketamine). In this study, recipients of morphine in a time of 100 minutes after injection experienced a slowly reduced pain. The LDK Group, during the first 5 minutes, had the greatest pain reduction; 15 minutes later the effect of ketamine was reduced. Finally, it can be concluded that LDK is not superior to morphine as an analgesic.
Several studies have also examined the safety and analgesic effects of ketamine in pre-hospital. Jennings et al. (21) in a systematic review on the effects of ketamine on reducing pain in pre-hospital trauma patients demonstrated that ketamine, as a safe and effective analgesic, can be utilized in the pre-hospital.
In a non-randomized retrospective cohort study carried out in pre-hospitals in the war zone of Iraq, the analgesic effect of ketamine, at a dose of 0.2 mg/kg, was compared with pentazocine at 0.4 mg/kg and placebo. The authors concluded that intravenous ketamine improved blood pressure and is a good analgesic for low-resource setting (22).
Lak et al. used 0.5 mg/kg followed by a continuous infusion (in a rate of 2 µg/kg/min for the first 24 hours and 1 µg/kg/min for the next 24 hours) of ketamine, in a study on 50 post-nephrectomy cases; they showed a decreased need to analgesics using ketamine compared to placebo (23). Intravenous, subcutaneous, and spray forms of ketamine were shown to decrease children’s pain and the need to analgesics, effectively, in 2 studies on post-tonsillectomy cases (24, 25).
The present study suggests that the analgesic effect of LDK is similar to morphine 15 minutes after injection. In the next few minutes, LDK effect in reducing pain was weakened unlike the morphine group. Previous studies mentioned above also demonstrated the effect of ketamine in the first few minutes after injection. A point of interest in our study was that complications caused in the LDK group were less than the morphine group. Flushing and drop in O2 saturation below 90% in the morphine group was significantly higher. On the other hand, the LDK group required additional tranquilizers; in addition, recipients of morphine were more satisfied with analgesia. This points show the need for further studies with larger sample sizes and different doses of ketamine.
5.1. Limitations
Some side effects such as nystagmus may interfere with blinding the study. The recipients were followed for 60 minutes. Increasing patients’ follow-up time provided the possibility of obtaining valuable results.
5.2. Conclusion
The results of this study suggest that low dose ketamine, at a dose of 0.2 mg/kg in early minutes, leads to significant reduction of pain when compared to that of intravenous morphine. It also created fewer complications than morphine.